Sun, Dec 14, 2025
| فارسی
Volume 30, Issue 1 (Continuously Updated 2024)
IJPCP 2024, 30(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Moshtaghi E, Bayazi M H, Rigi Koote B. Comparing the Effects of CBT Plus tDCS or Pharmacotherapy on Depressive Symptoms, Inhibition, and Cognitive Flexibility in Stroke Patients: A Randomized Clinical Trial. IJPCP 2024; 30 (1) : 4835.1
URL: http://ijpcp.iums.ac.ir/article-1-4070-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4070-en.html
1- Department of Psychology, Torbat-e Jam branch, Islamic Azad University, Torbat-e Jam, Iran.
2- Department of Psychology, Torbat-e Jam branch, Islamic Azad University, Torbat-e Jam, Iran. ,bayazi@iautj.ac.ir
3- Department of Clinical Psychology, Child and Adolescent Health Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
2- Department of Psychology, Torbat-e Jam branch, Islamic Azad University, Torbat-e Jam, Iran. ,
3- Department of Clinical Psychology, Child and Adolescent Health Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
Keywords: Cognitive-behavioral therapy, Pharmacotherapy, Citalopram, depression, Inhibition, cognitive flexibility, Stroke
Full-Text [PDF 6626 kb]
(972 Downloads)
| Abstract (HTML) (2575 Views)
Full-Text: (404 Views)
Introduction
Stroke accounts for 2.5% of all deaths worldwide. It causes severe disabilities among survivors, making it the leading cause of disability. In the post-stroke period, the occurrence of depression and neuropsychological disorders is highly prevalent. Approximately 30% of stroke survivors experience depression and about 70% suffer from neuropsychological disorders, posing a significant burden on healthcare systems and patients. Neuropsychological disorders are usually characterized by specific deficits in learning, working memory, executive functions (such as inhibition and cognitive flexibility), attention, and processing speed.
Cognitive flexibility (the ability to shift between tasks), is one of the main dimensions of executive functioning that allows a person to control their actions and flexibly adapt to changing environments. Cognitive flexibility is mainly processed in the ventrolateral prefrontal cortex. Cognitive inhibition referees to the ability to stop a mental process, intentionally or unintentionally, for mental suppression of competing information. Cognitive inhibition activates the prefrontal cortex, left anterior insula, and dorsal frontal inhibitory system. In addition, parts of the dorsal anterior cingulate are involved during cognitive inhibition. Impairment of this cognitive function is a core feature of many major psychiatric disorders, including depression.
This study aims to compare the effectiveness of cognitive-behavioral therapy (CBT) combined with transcranial direct current stimulation (tDCS) versus CBT combined with pharmacotherapy in reducing depressive symptoms and improving executive functions (inhibition and cognitive flexibility) in stroke patients.
Method
This is a randomized controlled clinical trial with a pre-test/post-test/two-month follow-up design. The study population consists of all stroke patients referred to Dr. Hashemzahi's neurology clinic in Zahedan, south of Iran, in 2022. Initially, 138 individuals were assessed for eligibility. After applying the inclusion criteria, 57 individuals entered the study stages, and finally, data from 45 participants were analyzed. The eligible patients who were selected using a convenience sampling method and randomly assigned into three groups of 15. All participants completed three computerized tests at baseline including Stroop test, Go/No Go test, and Beck Depression Inventory (BDI). The first group received CBT plus tDCS (2 mA, five sessions per week for 4 weeks). The second group received CBT plus pharmacotherapy (10 mg citalopram for three weeks), and the third group received no intervention. At the end of the interventions and after two months, the computerized tests and BDI were administered again to all participants in three groups. The CBT was conducted at 12 sessions according to Kootker et al.'s CBT protocol for stroke patients. The data were analyzed by the mixed analysis of variance (ANOVA) in SPSS software, version 29.
Results
The results of mixed ANOVA indicated that the effects of time and group were significant on depression symptoms, but the interaction effect of time and group was not significant (Table 1). This means that depression scores were significantly different between at least two groups. Post hoc tests showed that two intervention groups were significantly different compared to the control group, but there was no significant difference between the two intervention groups. In other words, both CBT+tDCS and CBT+pharmacotherapy significantly reduced depression symptoms, and there was no significant difference between their effectiveness. Additionally, the comparison of three evaluation phases showed that depression level was significantly different between pre-test and post-test and between pre-test and follow-up phases, indicating the maintained effect of the interventions. However, changes in depression scores over three periods were not significantly different between the three groups.
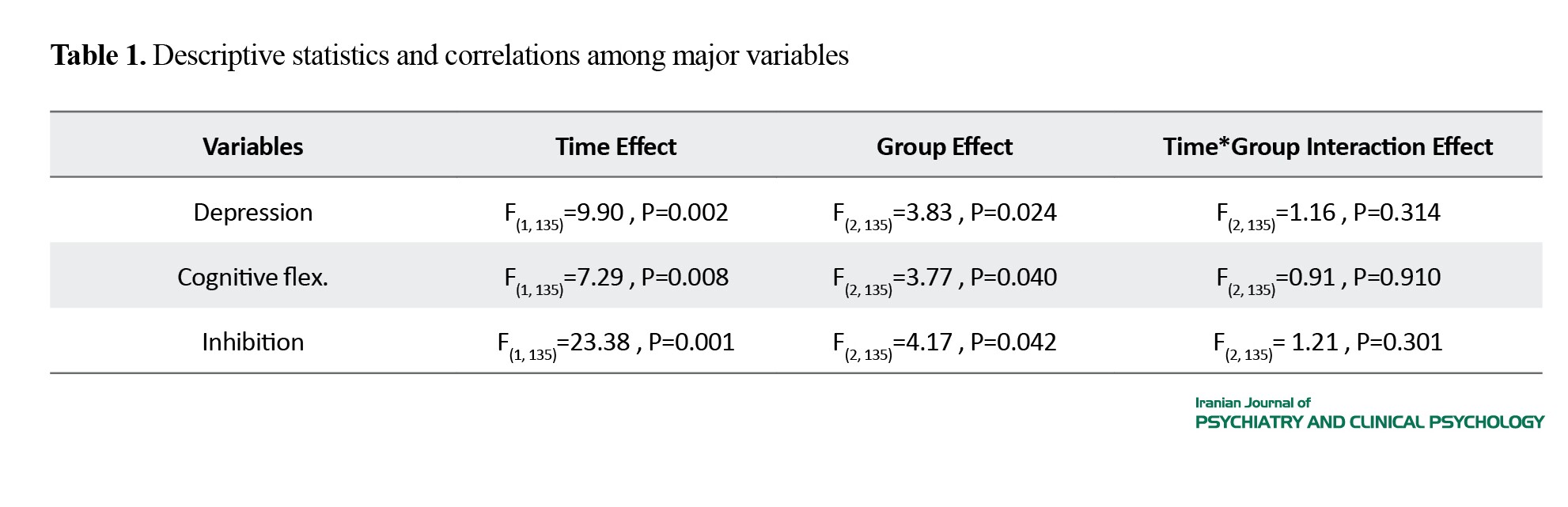
Regarding cognitive flexibility and inhibition, the results indicated that the effect of time and group on both variables were significant, but the interaction effect of time and group was not significant. Post hoc tests indicated that only the CBT+tDCS was significantly different compared to the control group. Additionally, the differences in two variables were significant only between pre-test and post-test phases, and the effect was not maintained in the follow-up phase. Therefore, it can be said that the three groups had different trends over time.
Conclusions
The CBT combined with tDCS has a long-term effect on reducing depression symptoms and short-term effects on improving cognitive functions, including inhibition and cognitive flexibility in stroke patients. The CBT combined with pharmacotherapy (10 mg citalopram) has a long-term effect on alleviating depression symptoms but it has no significant effect on the cognitive functions.
Ethical Considerations
Compliance with ethical guidelines
A written informed consent was obtained from the participants and their information was kept confidential. They were free to leave the study at any time. This study was approved by Islamic Azad University, Torbat-e-Jam Branch (Code: IR.IAU.TJ.REC.1402.003) and was registered by the Iranian Registry of Clinical Trials (ID: IRCT20230618058511N1).
Funding
This study was from the PhD thesis of Elahe Moshtaghi, funded by Islamic Azad University, Torbat-e-Jam Branch.
Authors contributions
Conceptualization and design: Elahe Moshtaghi and Mohammad Hossein Bayazi; data collection, data analysis, and initial draft preparation: Elahe Moshtaghi; supervision: Mohammad Hossein Bayazi; data analysis and interpretations: Behzad Rigi Koote. All authors read and approved the final version of the manuscript.
Conflicts of interest
According to the authors, there is no conflict of interest.
Acknowledgments
The authors would like to thank Dr. Hashemzahi and the staff of his neurology clinic, as well as all participants for their cooperation in this research.
Stroke accounts for 2.5% of all deaths worldwide. It causes severe disabilities among survivors, making it the leading cause of disability. In the post-stroke period, the occurrence of depression and neuropsychological disorders is highly prevalent. Approximately 30% of stroke survivors experience depression and about 70% suffer from neuropsychological disorders, posing a significant burden on healthcare systems and patients. Neuropsychological disorders are usually characterized by specific deficits in learning, working memory, executive functions (such as inhibition and cognitive flexibility), attention, and processing speed.
Cognitive flexibility (the ability to shift between tasks), is one of the main dimensions of executive functioning that allows a person to control their actions and flexibly adapt to changing environments. Cognitive flexibility is mainly processed in the ventrolateral prefrontal cortex. Cognitive inhibition referees to the ability to stop a mental process, intentionally or unintentionally, for mental suppression of competing information. Cognitive inhibition activates the prefrontal cortex, left anterior insula, and dorsal frontal inhibitory system. In addition, parts of the dorsal anterior cingulate are involved during cognitive inhibition. Impairment of this cognitive function is a core feature of many major psychiatric disorders, including depression.
This study aims to compare the effectiveness of cognitive-behavioral therapy (CBT) combined with transcranial direct current stimulation (tDCS) versus CBT combined with pharmacotherapy in reducing depressive symptoms and improving executive functions (inhibition and cognitive flexibility) in stroke patients.
Method
This is a randomized controlled clinical trial with a pre-test/post-test/two-month follow-up design. The study population consists of all stroke patients referred to Dr. Hashemzahi's neurology clinic in Zahedan, south of Iran, in 2022. Initially, 138 individuals were assessed for eligibility. After applying the inclusion criteria, 57 individuals entered the study stages, and finally, data from 45 participants were analyzed. The eligible patients who were selected using a convenience sampling method and randomly assigned into three groups of 15. All participants completed three computerized tests at baseline including Stroop test, Go/No Go test, and Beck Depression Inventory (BDI). The first group received CBT plus tDCS (2 mA, five sessions per week for 4 weeks). The second group received CBT plus pharmacotherapy (10 mg citalopram for three weeks), and the third group received no intervention. At the end of the interventions and after two months, the computerized tests and BDI were administered again to all participants in three groups. The CBT was conducted at 12 sessions according to Kootker et al.'s CBT protocol for stroke patients. The data were analyzed by the mixed analysis of variance (ANOVA) in SPSS software, version 29.
Results
The results of mixed ANOVA indicated that the effects of time and group were significant on depression symptoms, but the interaction effect of time and group was not significant (Table 1). This means that depression scores were significantly different between at least two groups. Post hoc tests showed that two intervention groups were significantly different compared to the control group, but there was no significant difference between the two intervention groups. In other words, both CBT+tDCS and CBT+pharmacotherapy significantly reduced depression symptoms, and there was no significant difference between their effectiveness. Additionally, the comparison of three evaluation phases showed that depression level was significantly different between pre-test and post-test and between pre-test and follow-up phases, indicating the maintained effect of the interventions. However, changes in depression scores over three periods were not significantly different between the three groups.
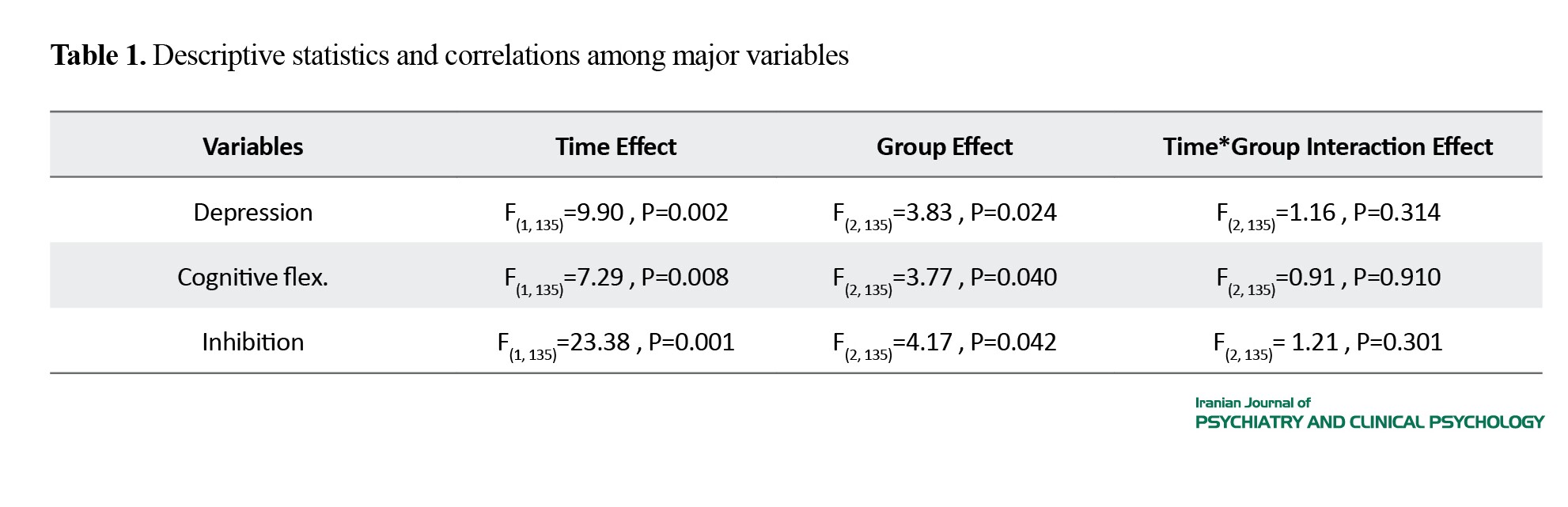
Regarding cognitive flexibility and inhibition, the results indicated that the effect of time and group on both variables were significant, but the interaction effect of time and group was not significant. Post hoc tests indicated that only the CBT+tDCS was significantly different compared to the control group. Additionally, the differences in two variables were significant only between pre-test and post-test phases, and the effect was not maintained in the follow-up phase. Therefore, it can be said that the three groups had different trends over time.
Conclusions
The CBT combined with tDCS has a long-term effect on reducing depression symptoms and short-term effects on improving cognitive functions, including inhibition and cognitive flexibility in stroke patients. The CBT combined with pharmacotherapy (10 mg citalopram) has a long-term effect on alleviating depression symptoms but it has no significant effect on the cognitive functions.
Ethical Considerations
Compliance with ethical guidelines
A written informed consent was obtained from the participants and their information was kept confidential. They were free to leave the study at any time. This study was approved by Islamic Azad University, Torbat-e-Jam Branch (Code: IR.IAU.TJ.REC.1402.003) and was registered by the Iranian Registry of Clinical Trials (ID: IRCT20230618058511N1).
Funding
This study was from the PhD thesis of Elahe Moshtaghi, funded by Islamic Azad University, Torbat-e-Jam Branch.
Authors contributions
Conceptualization and design: Elahe Moshtaghi and Mohammad Hossein Bayazi; data collection, data analysis, and initial draft preparation: Elahe Moshtaghi; supervision: Mohammad Hossein Bayazi; data analysis and interpretations: Behzad Rigi Koote. All authors read and approved the final version of the manuscript.
Conflicts of interest
According to the authors, there is no conflict of interest.
Acknowledgments
The authors would like to thank Dr. Hashemzahi and the staff of his neurology clinic, as well as all participants for their cooperation in this research.
References
- Zhao Y, Zhang X, Chen X, Wei Y. Neuronal injuries in cerebral infarction and ischemic stroke: From mechanisms to treatment. International Journal of Molecular Medicine. 2022; 49(2):15.[DOI:10.3892/ijmm.2021.5070] [PMID]
- Andres W, Rothstein A, Elser H, Sloane KL, Gottesman RF, Kasner SE, et al. Trends in the prevalence of stroke among community-dwelling individuals in the US, 1999-2018. JAMA Neurology. 2023; 80(6):646-8. [DOI:10.1001/jamaneurol.2023.0742] [PMID]
- Fiuji H, Namayandeh S, Jam Barsang S, Erfani M. Epidemiologic study of the main risk factors for one year ischemic stroke and surivial in patients admitted to the Neurology Department of Ghayim Hospital in Mashhad, Iran, 2015. The Journal of Tolooebehdasht. 2020; 19(2):33-42. [DOI:10.18502/tbj.v19i2.3394]
- Medeiros GC, Roy D, Kontos N, Beach SR. Post-stroke depression: A 2020 updated review. General Hospital Psychiatry. 2020; 66:70-80. [DOI:10.1016/j.genhosppsych.2020.06.011] [PMID]
- Rost NS, Brodtmann A, Pase MP, van Veluw SJ, Biffi A, Duering M, et al. Post-stroke cognitive impairment and dementia. Circulation Research. 2022; 130(8):1252-71. [DOI:10.1161/CIRCRESAHA.122.319951] [PMID]
- Robinson RG, Jorge RE. Post-stroke depression: A review. American Journal of Psychiatry. 2016; 173(3):221-31. [DOI:10.1176/appi.ajp.2015.15030363] [PMID]
- Guo J, Wang J, Sun W, Liu X. The advances of post-stroke depression: 2021 update. Journal of Neurology. 2022; 269(3):1236-49. [PMID]
- Shi Y, Yang D, Zeng Y, Wu W. Risk factors for post-stroke depression: A meta-analysis. Frontiers in Aging Neuroscience. 2017; 9:218. [DOI:10.3389/fnagi.2017.00218] [PMID]
- Grajny K, Pyata H, Spiegel K, Lacey EH, Xing S, Brophy C, et al. Depression symptoms in chronic left hemisphere stroke are related to dorsolateral prefrontal cortex damage. The Journal of Neuropsychiatry and Clinical Neurosciences. 2016; 28(4):292-8. [DOI:10.1176/appi.neuropsych.16010004] [PMID]
- Gonzalez J, Morales IS, Villarreal DM, Derrick BE. Low-frequency stimulation induces long-term depression and slow onset long-term potentiation at perforant path-dentate gyrus synapses in vivo. Journal of Neurophysiology. 2014; 111(6):1259-73. [DOI:10.1152/jn.00941.2012] [PMID]
- Alavian F, Haizadeh S. [Cognitive disorders resulting from stroke (Persian)]. Advances in Cognitive Sciences. 2018; 20 (3):15-33. [Link]
- Reichenberg A. The assessment of neuropsychological functioning in schizophrenia. Dialogues in Clinical Neuroscience. 2010; 12(3):383-92. [DOI:10.31887/DCNS.2010.12.3/areichenberg] [PMID]
- Buttelmann F, Karbach J. Development and plasticity of cognitive flexibility in early and middle childhood. Frontiers in Psychology. 2017; 8:1040. [DOI:10.3389/fpsyg.2017.01040] [PMID]
- Povroznik JM, Ozga JE, Vonder Haar C, Engler-Chiurazzi EB. Executive (dys) function after stroke: special considerations for behavioral pharmacology. Behavioural Pharmacology. 2018; 29(7):638-53. [DOI:10.1097/FBP.0000000000000432] [PMID]
- Hung Y, Gaillard SL, Yarmak P, Arsalidou M. Dissociations of cognitive inhibition, response inhibition, and emotional interference: Voxelwise ALE meta-analyses of fMRI studies. Human Brain Mapping. 2018; 39(10):4065-82. [DOI:10.1002/hbm.24232] [PMID]
- Harfmann EJ, Rhyner KT, Ingram RE. Cognitive inhibition and attentional biases in the affective go/no-go performance of depressed, suicidal populations. Journal of Affective Disorders. 2019; 256:228-33. [DOI:10.1016/j.jad.2019.05.022] [PMID]
- Starkstein SE, Hayhow BD. Treatment of post-stroke depression. Current Treatment Options in Neurology. 2019; 21(7):31. [DOI:10.1007/s11940-019-0570-5] [PMID]
- Wang SB, Wang YY, Zhang QE, Wu SL, Ng CH, Ungvari GS, et al. Cognitive behavioral therapy for post-stroke depression: A meta-analysis. Journal of Affective Disorders. 2018; 235:589-96. [DOI:10.1016/j.jad.2018.04.011] [PMID]
- Withers H, Plumbley-Jones J, Pyatt E, Williams L, Yule L, Kyte D. The effectiveness of cognitive behavioural therapy versus antidepressants for treatment of post-stroke depression in adults. The British Student Doctor Journal. 2021; 5(1):5-17. [Link]
- Zhang C, He L, Li Z, Qiu H, Wang X, Zhang Y. Effectiveness of non-pharmacological interventions for treating post-stroke depression: Study protocol of an umbrella review of systematic reviews and meta-analyses. Medicine. 2021; 100(51):e28370. [DOI:10.1097/MD.0000000000028370] [PMID]
- Bucur M, Papagno C. A systematic review of noninvasive brain stimulation for post-stroke depression. Journal of Affective Disorders. 2018; 238:69-78. [DOI:10.1016/j.jad.2018.05.026] [PMID]
- Hassan AB, Danazumi MS, Abdullahi A, Yakasai AM. Effect of transcranial direct current stimulation (tDCS) delivered via dorsolateral prefrontal cortex on central post-stroke pain and depression: A case report. Physiotherapy Theory and Practice. 2022; 38(11):1799-806. [DOI:10.1080/09593985.2021.1891591] [PMID]
- Chan MMY, Yau SSY, Han YMY. The neurobiology of prefrontal transcranial direct current stimulation (tDCS) in promoting brain plasticity: A systematic review and meta-analyses of human and rodent studies. Neuroscience & Biobehavioral Reviews. 2021; 125:392-416. [DOI:10.1016/j.neubiorev.2021.02.035] [PMID]
- Oldrati V, Schutter DJLG. Targeting the human cerebellum with transcranial direct current stimulation to modulate behavior: A meta-analysis. The Cerebellum. 2018; 17(2):228-36. [DOI:10.1007/s12311-017-0877-2] [PMID]
- Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, et al. Clinical research with transcranial direct current stimulation (tDCS): Challenges and future directions. Brain Stimulation. 2012; 5(3):175-95. [DOI:10.1016/j.brs.2011.03.002] [PMID]
- Utz KS, Dimova V, Oppenländer K, Kerkhoff G. Electrified minds: Transcranial Direct Current Stimulation (tDCS) and Galvanic Vestibular Stimulation (GVS) as methods of non-invasive brain stimulation in neuropsychology-a review of current data and future implications. Neuropsychologia. 2010; 48(10):2789-810. [DOI:10.1016/j.neuropsychologia.2010.06.002] [PMID]
- Rodríguez-Gómez JR, Dávila-Martínez MG, Collazo-Rodríguez LC. Factor structure of the Beck Depression Inventory-(BDI-II) with Puerto Rican elderly. Puerto Rico Health Sciences Journal. 2006; 25(2):127-32. [PMID]
- Bagharian Sararoudi R, Bahrami Ehsan H, Gilani B, Sanei H. [Perceived personal control and depression after heart attack (Persian)]. Journal of Clinical Psychology 2009; 1(2). [Link]
- Segal DL, Coolidge FL, Cahill BS, O’Riley AA. Psychometric properties of the Beck Depression Inventory-II (BDI-II) among community-dwelling older adults. Behavior Modification. 2008; 32(1):3-20. [DOI:10.1177/0145445507303833] [PMID]
- Brunetti R, Indraccolo A, Del Gatto C, Farina B, Imperatori C, Fontana E, et al. eStroop: Implementation, standardization, and systematic comparison of a new voice-key version of the traditional stroop task. Frontiers in Psychology. 2021; 12:663786. [DOI:10.3389/fpsyg.2021.663786] [PMID]
- Khodadadi M, Feyzi Daryati MR, Movahedi Y, Ahmadi I. [Assessment of attention bias in the cognitive processing of neutral and emotional words Using semantic Strop test (Persian)]. Shenakht Journal of Psychology and Psychiatry. 2014; 1(1):23-30. [Link]
- Vila J, Guerra P, Muñoz MA, Vico C, Viedma-del Jesús MI, Delgado LC, et al. Cardiac defense: From attention to action. International Journal of Psychophysiology. 2007; 66(3):169-82. [DOI:10.1016/j.ijpsycho.2007.07.004] [PMID]
- Sue Baron I. Delis-Kaplan executive function system. Child Neuropsychology. 2004; 10(2):147-52. [DOI:10.1080/09297040490911140]
- Ghadiri F, Jazayeri A, A'shayeri H, Ghazi-Tabatabaei M. The role of cognitive rehabilitation in reduction of executive function deficits and obsessive-compulsive symptoms in schizo-obsessive patients. Archives of Rehabilitation. 2007; 7(4):11-24. [Link]
- Li H, Zhu N, Klomparens EA, Xu S, Wang M, Wang Q, et al. Application of functional near-infrared spectroscopy to explore the neural mechanism of transcranial direct current stimulation for post-stroke depression. Neurological Research. 2019; 41(8):714-21. [DOI:10.1080/01616412.2019.1612539] [PMID]
- Kootker JA, Rasquin SM, Smits P, Geurts AC, van Heugten CM, Fasotti L. An augmented cognitive behavioural therapy for treating post-stroke depression: Description of a treatment protocol. Clinical Rehabilitation. 2015; 29(9):833-43. [DOI:10.1177/0269215514559987] [PMID]
- Kootker JA, Rasquin SM, Lem FC, van Heugten CM, Fasotti L, Geurts AC. Augmented cognitive behavioral therapy for poststroke depressive symptoms: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2017; 98(4):687-94. [DOI:10.1016/j.apmr.2016.10.013] [PMID]
- Goerigk SA, Padberg F, Chekroud A, Kambeitz J, Bühner M, Brunoni AR. Parsing the antidepressant effects of non-invasive brain stimulation and pharmacotherapy: A symptom clustering approach on ELECT-TDCS. Brain Stimulation. 2021; 14(4):906-12. [DOI:10.1016/j.brs.2021.05.008] [PMID]
- Ahrens J, Shao R, Blackport D, Macaluso S, Viana R, Teasell R, et al. Cognitive-behavioral therapy for managing depressive and anxiety symptoms after stroke: A systematic review and meta-analysis. Topics in Stroke Rehabilitation. 2023; 30(4):368-83. [DOI:10.1080/10749357.2022.2049505] [PMID]
- LeMoult J, Gotlib IH. Depression: A cognitive perspective. Clinical Psychology Review. 2019; 69:51-66. [DOI:10.1016/j.cpr.2018.06.008] [PMID]
- Godlewska BR, Harmer CJ. Cognitive neuropsychological theory of antidepressant action: A modern-day approach to depression and its treatment. Psychopharmacology. 2021; 238(5):1265-78. [DOI:10.1007/s00213-019-05448-0] [PMID]
- Shiozawa P, Fregni F, Benseñor IM, Lotufo PA, Berlim MT, Daskalakis JZ, et al. Transcranial direct current stimulation for major depression: An updated systematic review and meta-analysis. International Journal of Neuropsychopharmacology. 2014; 17(9):1443-52. [DOI:10.1017/S1461145714000807] [PMID]
- De Raedt R, Leyman L, Baeken C, Van Schuerbeek P, Luypaert R, Vanderhasselt MA, et al. Neurocognitive effects of HF-rTMS over the dorsolateral prefrontal cortex on the attentional processing of emotional information in healthy women: An event-related fMRI study. Biological Psychology. 2010; 85(3):487-95. [DOI:10.1016/j.biopsycho.2010.09.015] [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2023/12/4 | Accepted: 2024/08/10 | Published: 2024/07/31
Received: 2023/12/4 | Accepted: 2024/08/10 | Published: 2024/07/31
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |