Tue, Jan 27, 2026
| فارسی
Volume 31, Issue 1 (Continuously Updated 2025)
IJPCP 2025, 31(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Razavi K, Poshtmashhadi M, Pourmohamadreza-Tajrishi M, Yarandi R B. Symptoms of Attention Deficit/Hyperactivity Disorder, Sleep Problems, and Executive Dysfunction, as Predictors of Sluggish Cognitive Tempo, in Children With High-Functioning Autism Spectrum Disorder. IJPCP 2025; 31 (1)
URL: http://ijpcp.iums.ac.ir/article-1-4317-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4317-en.html
1- Department of Psychology and Education of Exceptional Children, Faculty of Behavioral Sciences and Mental Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Psychology and Education of Exceptional Children, Faculty of Behavioral Sciences and Mental Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,mp.mashhadi@gmail.com
3- Psychosis Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Department of Biostatistics and Epidemiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Psychology and Education of Exceptional Children, Faculty of Behavioral Sciences and Mental Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Psychosis Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. & Department of Biostatistics and Epidemiology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Keywords: Sluggish cognitive tempo (SCT), Cognitive disengagement syndrome (CDS), Autism spectrum disorder (ASD), Children, Attention deficit disorder/hyperactivity disorder, Sleep problems, Executive functions
Full-Text [PDF 6173 kb]
(383 Downloads)
| Abstract (HTML) (562 Views)
Full-Text: (432 Views)
Introduction
Sluggish cognitive tempo (SCT), recently known as cognitive disengagement syndrome (CDS), is a relatively new clinical construct that refers to a set of cognitive and behavioral symptoms including lethargy, daydreaming, drowsiness, being easily confused, and slow thinking and responding. Most initial studies on SCT had focused on the empirical distinction between SCT and the inattentive type of attention deficit/hyperactivity disorder (ADHD). Following the emergence of additional evidence highlighting the differences between SCT and ADHD, researchers increasingly investigated the causes, correlates, and consequences of SCT. Their findings indicated that SCT is significantly linked to ADHD, sleep problems, executive functioning problems (particularly in metacognitive areas such as planning and organization), and symptoms of autism spectrum disorder (ASD). Most SCT studies have been conducted on ADHD samples and the general population, while SCT is prevalent among children with ASD. Few studies have explored the relationship between SCT and other symptoms in ASD children. In Iran, there has been no research on SCT in children with ASD. Therefore, this study aims to investigate the ADHD symptoms, sleep problems, and executive functions as predictors of SCT in Iranian children with high-functioning ASD.
Method
This is a descriptive-correlational study. The participants were the parents of 122 children aged 6-12 with high-functioning ASD selected from specialized autism schools in Tehran, Iran. Data was collected using the convenience sampling method from January to February 2024. The parents who scored 55-70 in the Gilliam Autism rating scale-third edition and had a score above the cut-off point on the SCT scale were selected. They completed the online forms of the Swanson, Nolan, and Pelham rating scale (SNAP-IV), the children’s sleep habits questionnaire (CSHQ), and the coolidge personality and neuropsychological inventory for children (CPNI).
The SPSS software, version 27 was used for data analysis. The Shapiro-Wilk test was first employed to assess the normality of data distribution. Pearson’s correlation test was then used to calculate the correlation between the variables. Finally, multiple regression analysis was used to find the predictors. The significance level was set at 0.05.
Results
The final analysis was conducted on the parents of 116 children. Since the skewness and kurtosis values for all variables fall within the range of -2 to 2, the distributions were considered normal. Furthermore, the Shapiro-Wilk test results showed all variables had a normal distribution (P>0.05).
The results in Table 1 indicated that SCT, as the criterion variable, had a positive and significant association with three variables: Inattention, decision-making/planning, and organizing.
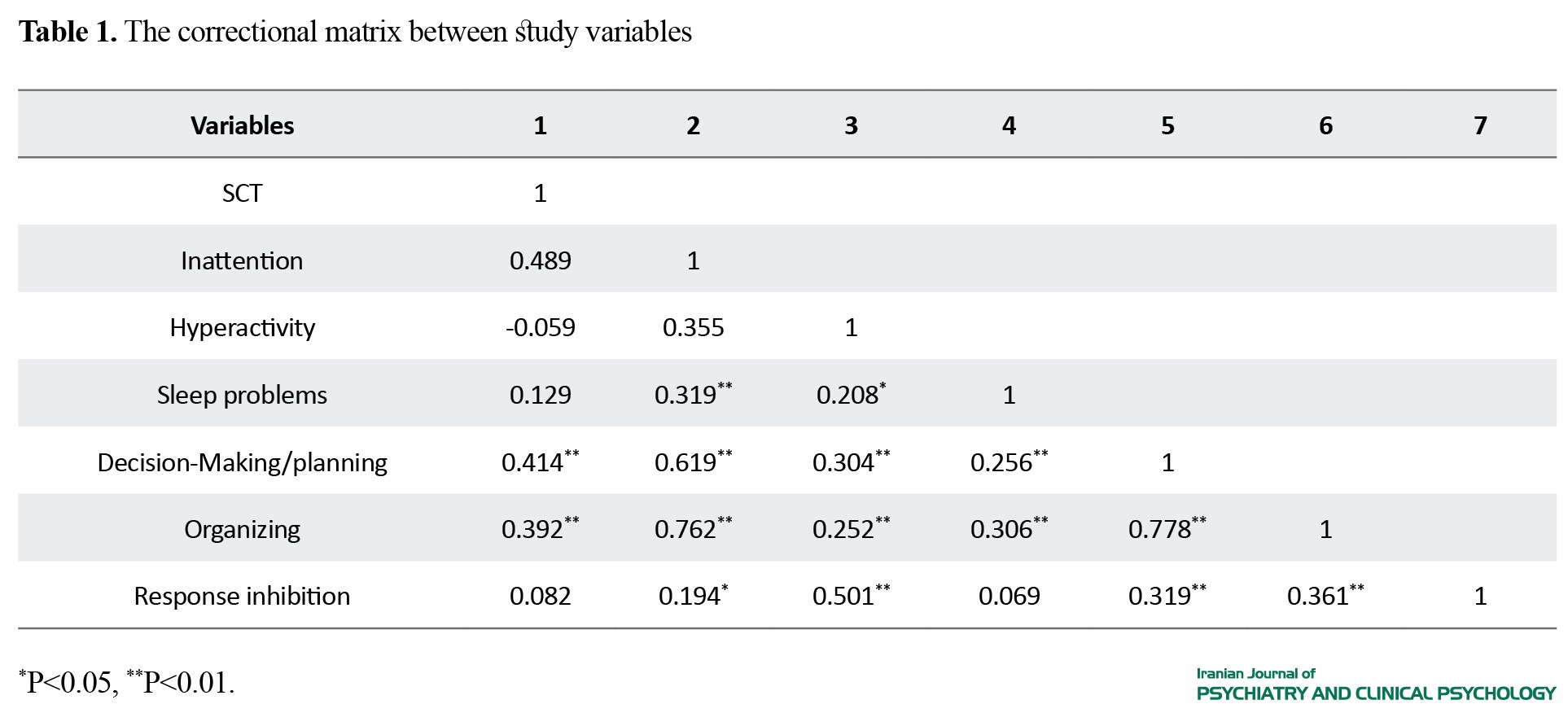
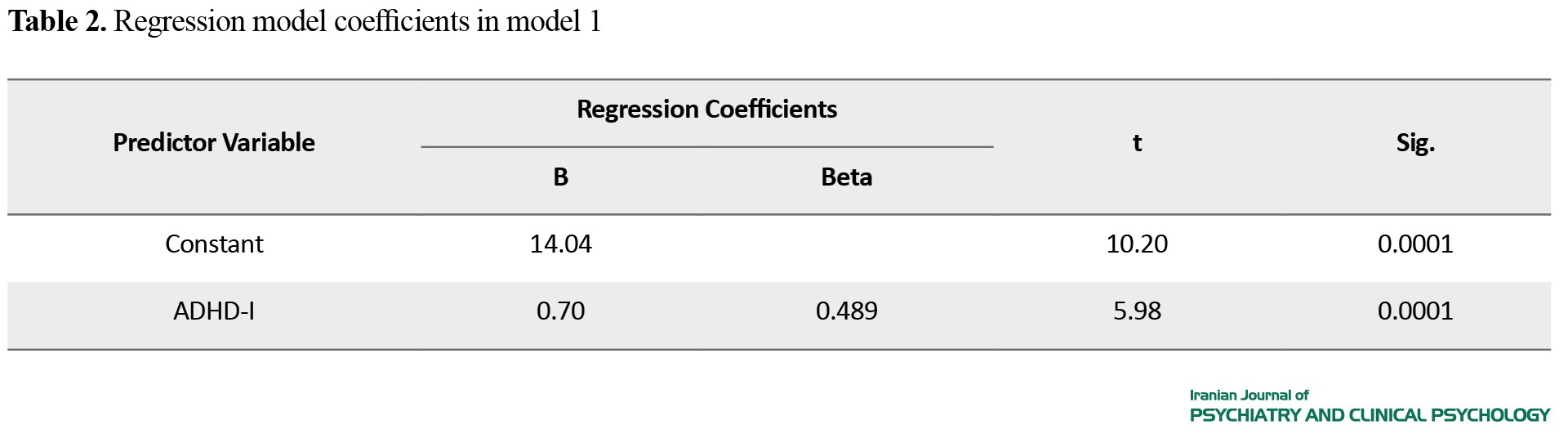
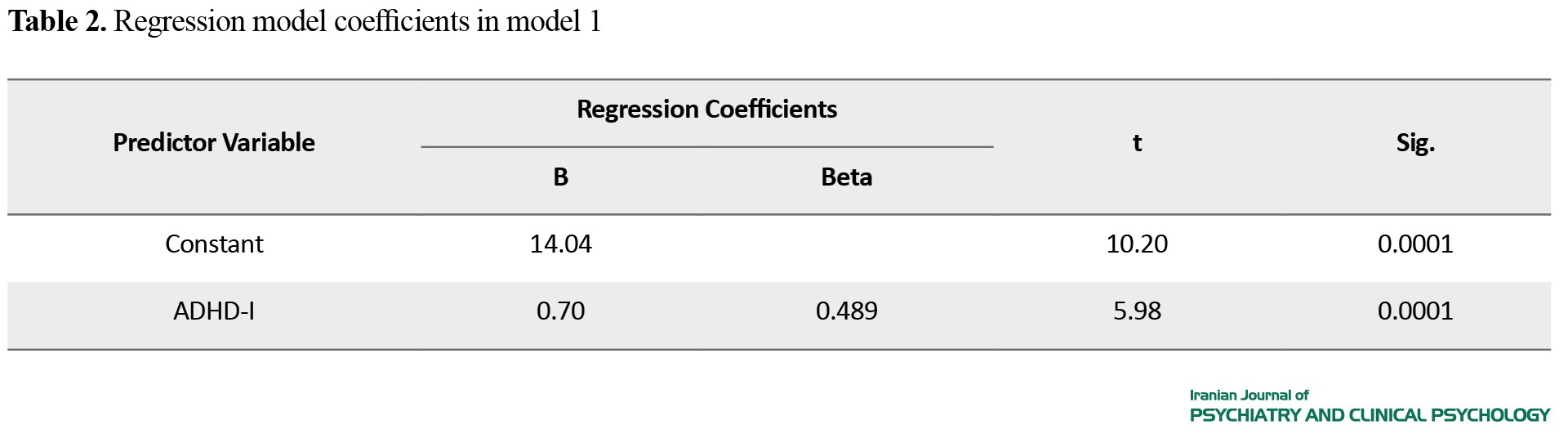
The SCT had no significant relationship with the variables of sleep problems, hyperactivity, and response inhibition. Consequently, sleep problems, hyperactivity, and response inhibition were excluded from the regression model. The regression analysis results indicated that only inattention had a significant predictive power and was significantly correlated with SCT (P<0.05, r=0.489). In this model, the coefficient of determination was 0.23, indicating that inattention accounts for 0.23 of the variance in the SCT variable (Table 2).
Conclusion
The SCT is not correlated with sleep problems in children with high-functioning ASD. However, this finding remains controversial and requires further investigation. The second finding of the study is that SCT has a positive and significant correlation with the inattentive symptom of ADHD in these children, but not with the hyperactive symptom of ADHD. The inattentive symptom is a significant predictor of SCT in children with ASD. Given the overlap of symptoms between SCT and inattention and the high co-occurrence of ADHD in children with ASD, it is reasonable to expect a significant relationship between SCT and inattention in children with ASD. The third finding is that SCT has a positive and significant correlation with decision-making and organizing skills of children with ASD, but has no significant relationship with the response inhibition skill. Given the characteristics of children with SCT symptoms, such as daydreaming, being easily confused, slow thinking and responding, and a lack of constant vigilance, it is expected that these children experience difficulties with executive functions, including working memory, planning, and organization. The findings of this study offer comprehensive insights into the variables associated with SCT in children with ASD. This information can enhance the knowledge of parents, professionals, and therapists who work with and provide services for this group of children.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committees of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1402.196). Written informed consent was obtained from all parents before the study. Their information was kept confidential.
Funding
This article was extracted from the master's thesis of Kosar Razavi at the Department of Psychology and Education of Exceptional Children, University of Social Welfare and Rehabilitation Sciences. This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, review & editing: Marjan Poshtmashhadi, Masoume Pourmohamadreza-Tajrishi, and Kosar Razavi; Methodology and validation: All authors; data analysis: Marjan Poshtmashhadi, Kosar Razavi, and Razie Bidhendi Yarandi; investigation, writing initial draft: Kosar Razavi; Supervision: Marjan Poshtmashhadi, Masoume Pourmohamadreza-Tajrishi, and Razie Bidhendi Yarandi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Exceptional Education Organization in Tehran and all children and parents for their cooperation in this research.
References
Sluggish cognitive tempo (SCT), recently known as cognitive disengagement syndrome (CDS), is a relatively new clinical construct that refers to a set of cognitive and behavioral symptoms including lethargy, daydreaming, drowsiness, being easily confused, and slow thinking and responding. Most initial studies on SCT had focused on the empirical distinction between SCT and the inattentive type of attention deficit/hyperactivity disorder (ADHD). Following the emergence of additional evidence highlighting the differences between SCT and ADHD, researchers increasingly investigated the causes, correlates, and consequences of SCT. Their findings indicated that SCT is significantly linked to ADHD, sleep problems, executive functioning problems (particularly in metacognitive areas such as planning and organization), and symptoms of autism spectrum disorder (ASD). Most SCT studies have been conducted on ADHD samples and the general population, while SCT is prevalent among children with ASD. Few studies have explored the relationship between SCT and other symptoms in ASD children. In Iran, there has been no research on SCT in children with ASD. Therefore, this study aims to investigate the ADHD symptoms, sleep problems, and executive functions as predictors of SCT in Iranian children with high-functioning ASD.
Method
This is a descriptive-correlational study. The participants were the parents of 122 children aged 6-12 with high-functioning ASD selected from specialized autism schools in Tehran, Iran. Data was collected using the convenience sampling method from January to February 2024. The parents who scored 55-70 in the Gilliam Autism rating scale-third edition and had a score above the cut-off point on the SCT scale were selected. They completed the online forms of the Swanson, Nolan, and Pelham rating scale (SNAP-IV), the children’s sleep habits questionnaire (CSHQ), and the coolidge personality and neuropsychological inventory for children (CPNI).
The SPSS software, version 27 was used for data analysis. The Shapiro-Wilk test was first employed to assess the normality of data distribution. Pearson’s correlation test was then used to calculate the correlation between the variables. Finally, multiple regression analysis was used to find the predictors. The significance level was set at 0.05.
Results
The final analysis was conducted on the parents of 116 children. Since the skewness and kurtosis values for all variables fall within the range of -2 to 2, the distributions were considered normal. Furthermore, the Shapiro-Wilk test results showed all variables had a normal distribution (P>0.05).
The results in Table 1 indicated that SCT, as the criterion variable, had a positive and significant association with three variables: Inattention, decision-making/planning, and organizing.
The SCT had no significant relationship with the variables of sleep problems, hyperactivity, and response inhibition. Consequently, sleep problems, hyperactivity, and response inhibition were excluded from the regression model. The regression analysis results indicated that only inattention had a significant predictive power and was significantly correlated with SCT (P<0.05, r=0.489). In this model, the coefficient of determination was 0.23, indicating that inattention accounts for 0.23 of the variance in the SCT variable (Table 2).
Conclusion
The SCT is not correlated with sleep problems in children with high-functioning ASD. However, this finding remains controversial and requires further investigation. The second finding of the study is that SCT has a positive and significant correlation with the inattentive symptom of ADHD in these children, but not with the hyperactive symptom of ADHD. The inattentive symptom is a significant predictor of SCT in children with ASD. Given the overlap of symptoms between SCT and inattention and the high co-occurrence of ADHD in children with ASD, it is reasonable to expect a significant relationship between SCT and inattention in children with ASD. The third finding is that SCT has a positive and significant correlation with decision-making and organizing skills of children with ASD, but has no significant relationship with the response inhibition skill. Given the characteristics of children with SCT symptoms, such as daydreaming, being easily confused, slow thinking and responding, and a lack of constant vigilance, it is expected that these children experience difficulties with executive functions, including working memory, planning, and organization. The findings of this study offer comprehensive insights into the variables associated with SCT in children with ASD. This information can enhance the knowledge of parents, professionals, and therapists who work with and provide services for this group of children.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committees of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1402.196). Written informed consent was obtained from all parents before the study. Their information was kept confidential.
Funding
This article was extracted from the master's thesis of Kosar Razavi at the Department of Psychology and Education of Exceptional Children, University of Social Welfare and Rehabilitation Sciences. This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, review & editing: Marjan Poshtmashhadi, Masoume Pourmohamadreza-Tajrishi, and Kosar Razavi; Methodology and validation: All authors; data analysis: Marjan Poshtmashhadi, Kosar Razavi, and Razie Bidhendi Yarandi; investigation, writing initial draft: Kosar Razavi; Supervision: Marjan Poshtmashhadi, Masoume Pourmohamadreza-Tajrishi, and Razie Bidhendi Yarandi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Exceptional Education Organization in Tehran and all children and parents for their cooperation in this research.
References
- Mayes SD, Becker SP, Waschbusch DA. Cognitive Disengagement Syndrome and Autism Traits are empirically distinct from each other and from other psychopathology dimensions. Research on Child and Adolescent Psychopathology. 2025; 53(2):151-61. [DOI:10.1007/s10802-024-01281-y] [PMID]
- Becker SP, Willcutt EG, Leopold DR, Fredrick JW, Smith ZR, Jacobson LA, et al. Report of a work group on sluggish cognitive tempo: Key research directions and a consensus change in terminology to cognitive disengagement syndrome. Journal of the American Academy of Child & Adolescent Psychiatry. 2023; 62(6):629-45. [DOI:10.1016/j.jaac.2022.07.821] [PMID]
- Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, et al. The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child & Adolescent Psychiatry. 2016; 55(3):163-78. [DOI:10.1016/j.jaac.2015.12.006] [PMID]
- Araujo Jiménez EA, Jané Ballabriga MC, Bonillo Martin A, Arrufat FJ, Serra Giacobo R. Executive functioning in children and adolescents with symptoms of sluggish cognitive tempo and ADHD. Journal of Attention Disorders. 2015; 19(6):507-14. [DOI:10.1177/1087054713495442] [PMID]
- Barkley RA. Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child & Adolescent Psychology. 2013; 42(2):161-73. [DOI:10.1080/15374416.2012.734259] [PMID]
- Dvorsky MR, Becker SP, Tamm L, Willoughby MT. Testing the longitudinal structure and change in sluggish cognitive tempo and inattentive behaviors from early through middle childhood. Assessment. 2021; 28(2):380-94. [DOI:10.1177/1073191119872247] [PMID]
- Mayes SD, Calhoun SL, Waschbusch DA. Relationship between sluggish cognitive tempo and sleep, psychological, somatic, and cognitive problems and impairment in children with autism and children with ADHD. Clinical Child Psychology and Psychiatry. 2021; 26(2):518-30. [DOI:10.1177/1359104520978459] [PMID]
- Mohammadi E, Shadbafi M. [Comparison of sensitivity to reward and punishment, response inhibition and sus-tained attention between school boys with attention deficit/hyperactivity disorder and sluggish cognitive tempo (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2021; 27(2):180-93. [DOI:10.32598/ijpcp.27.2.3294.1]
- Mueller AK, Tucha L, Koerts J, Groen Y, Lange KW, Tucha O. Sluggish cognitive tempo and its neurocognitive, social and emotive correlates: A systematic review of the current literature. Journal of Molecular Psychiatry. 2014; 2(1):5. [DOI:10.1186/2049-9256-2-5] [PMID]
- Reinvall O, Kujala T, Voutilainen A, Moisio AL, Lahti-Nuuttila P, Laasonen M. Sluggish cognitive tempo in children and adolescents with higher functioning autism spectrum disorders: Social impairments and internalizing symptoms. Scandinavian Journal of Psychology. 2017; 58(5):389-99. [DOI:10.1111/sjop.12379] [PMID]
- Rondon AT, Hilton DC, Jarrett MA, Ollendick TH. Sleep, internalizing problems, and social withdrawal: Unique associations in clinic-referred youth with elevated sluggish cognitive tempo symptoms. Journal of Attention Disorders. 2020; 24(4):524-34. [DOI:10.1177/1087054718756197] [PMID]
- Sáez B, Servera M, Becker SP, Burns GL. Optimal items for assessing sluggish cognitive tempo in children across mother, father, and teacher ratings. Journal of Clinical Child & Adolescent Psychology. 2019; 48(6):825-39. [DOI:10.1080/15374416.2017.1416619] [PMID]
- Skirbekk B, Hansen BH, Oerbeck B, Kristensen H. The relationship between sluggish cognitive tempo, subtypes of attention-deficit/hyperactivity disorder, and anxiety disorders. Journal of Abnormal Child Psychology. 2011; 39(4):513-25. [DOI:10.1007/s10802-011-9488-4] [PMID]
- Wåhlstedt C, Bohlin G. DSM-IV-defined inattention and sluggish cognitive tempo: independent and interactive relations to neuropsychological factors and comorbidity. Child Neuropsychology. 2010; 16(4):350-65. [DOI:10.1080/09297041003671176] [PMID]
- Willcutt EG, Chhabildas N, Kinnear M, DeFries JC, Olson RK, Leopold DR, et al. The internal and external validity of sluggish cognitive tempo and its relation with DSM-IV ADHD. Journal of Abnormal Child Psychology. 2014; 42(1):21-35. [DOI:10.1007/s10802-013-9800-6] [PMID]
- Becker SP, Garner AA, Byars KC. Sluggish cognitive tempo in children referred to a pediatric Sleep Disorders Center: Examining possible overlap with sleep problems and associations with impairment. Journal of Psychiatric Research. 2016; 77:116-24. [DOI:10.1016/j.jpsychires.2016.03.005] [PMID]
- Burns GL, Becker SP. Sluggish Cognitive Tempo and ADHD Symptoms in a Nationally Representative Sample of U.S. Children: Differentiation using categorical and dimensional approaches. Journal of Clinical Child and Adolescent Psychology. 2021; 50(2):267-80. [DOI:10.1080/15374416.2019.1678165] [PMID]
- Fredrick JW, Yeaman KM, Yu X, Langberg JM, Becker SP. A multi-method examination of sluggish cognitive tempo in relation to adolescent sleep, daytime sleepiness, and circadian preference. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2022; 63(12):1658-67. [DOI:10.1111/jcpp.13568] [PMID]
- Koriakin TA, Mahone EM, Jacobson LA. Sleep difficulties are associated with parent report of sluggish cognitive tempo.Journal of Developmental and Behavioral Pediatrics. 2015; 36(9):717-23.[DOI:10.1097/DBP.0000000000000224] [PMID]
- Mayes SD, Waschbusch DA, Fernandez-Mendoza J, Calhoun SL. Relationship between sluggish cognitive tempo and sleep, psychological, somatic, and cognitive problems in elementary school children. Journal of Pediatric Neuropsychology. 2021; 7(4):182-91. [Link]
- O'Hare K, White N, Harding R, Galland B, Sellbom M, Shine B, et al. Sluggish cognitive tempo and daytime sleepiness mediate relationships between sleep and academic performance. Journal of Developmental and Behavioral Pediatrics . 2021; 42(8):637-47. [DOI:10.1097/DBP.0000000000000948] [PMID]
- Smith ZR, Eadeh HM, Breaux RP, Langberg JM. Sleepy, sluggish, worried, or down? The distinction between self-reported sluggish cognitive tempo, daytime sleepiness, and internalizing symptoms in youth with attention-deficit/hyperactivity disorder. Psychological Assessment. 2019; 31(3):365-75. [DOI:10.1037/pas0000671] [PMID]
- Collado-Valero J, Navarro-Soria I, Delgado-Domenech B, Real-Fernández M, Costa-López B, Mazón-Esquiva I, et al. ADHD and sluggish cognitive tempo: comparing executive functioning response patterns. Sustainability. 2021; 13(19):10506. [DOI:10.3390/su131910506]
- Duncan A, Tamm L, Birnschein AM, Becker SP. Clinical correlates of sluggish cognitive tempo in adolescents with autism spectrum disorder. Autism. 2019; 23(6):1354-62. [DOI:10.1177/1362361318811329] [PMID]
- McFayden T, Jarrett MA, White SW, Scarpa A, Dahiya A, Ollendick TH. Sluggish cognitive tempo in Autism Spectrum Disorder, ADHD, and their comorbidity: Implications for impairment. Journal of Clinical Child and Adolescent Psychology. 2022; 51(2):195-202. [DOI:10.1080/15374416.2020.1716365] [PMID]
- Gadow KD, DeVincent CJ, Pomeroy J. ADHD symptom subtypes in children with pervasive developmental disorder. Journal of Autism and Developmental Disorders. 2006; 36(2):271-83.[DOI:10.1007/s10803-005-0060-3] [PMID]
- Lee DO, Ousley OY. Attention-deficit hyperactivity disorder symptoms in a clinic sample of children and adolescents with pervasive developmental disorders. Journal of Child & Adolescent Psychopharmacology. 2006; 16(6):737-46. [DOI:10.1089/cap.2006.16.737] [PMID]
- Mattila ML, Hurtig T, Haapsamo H, Jussila K, Kuusikko-Gauffin S, Kielinen M, et al. Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: A community- and clinic-based study. Journal of Autism and Developmental Disorders. 2010; 40(9):1080-93. [DOI:10.1007/s10803-010-0958-2] [PMID]
- Bahçivan Saydam R, Ayvaşik HB, Alyanak B. Executive functioning in subtypes of attention deficit hyperactivity disorder. Noro Psikiyatri Arsivi. 2015; 52(4):386-92. [DOI:10.5152/npa.2015.8712] [PMID]
- Tyagi V, Juneja M, Jain R. Sleep problems and their correlates in children with Autism Spectrum Disorder: An Indian Study. Journal of Autism and Developmental Disorders. 2019; 49(3):1169-81. [DOI:10.1007/s10803-018-3820-6] [PMID]
- Tzischinsky O, Meiri G, Manelis L, Bar-Sinai A, Flusser H, Michaelovski A, et al. Sleep disturbances are associated with specific sensory sensitivities in children with autism. Molecular Autism. 2018; 9:22. [DOI:10.1186/s13229-018-0206-8] [PMID]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth - Text Revision (DSM-5-TR). Virginia: American Psychiatric Association; 2022. [DOI:10.1176/appi.books.9780890425787]
- Demetriou EA, DeMayo MM, Guastella AJ. Executive function in Autism spectrum disorder: History, Theoretical Models, Empirical Findings, and Potential as an Endophenotype. Frontiers in Psychiatry. 2019; 10:753. [DOI:10.3389/fpsyt.2019.00753] [PMID]
- Friedman L, Sterling A. A review of language, executive function, and intervention in Autism Spectrum Disorder. Seminars in Speech and Language. 2019; 40(4):291-304. [DOI:10.1055/s-0039-1692964] [PMID]
- Gilliam JE. GARS-3: Gilliam Autism Rating Scale-Third Edition. Austin: Pro-Ed Publishers Austin; 2014. [Link]
- Duffy L, Baluch B, Welland S, Raman E. Effects of physical activity on debilitating behaviours in 13- to 20-year-old males with severe autism spectrum disorder. Journal of Exercise Rehabilitation. 2017; 13(3):340-7. [DOI:10.12965/jer.1734960.480] [PMID]
- Karren BC. A test review: Gilliam, JE (2014). Gilliam Autism rating scale-third edition (GARS-3). Los Angeles, CA: SAGE Publications Sage CA; 2017. [DOI:10.1177/0734282916635465]
- Gorji R, Hassanzadeh S, Ghasemzadeh S, Qolamali Lavasani M. [Sensitivity and specificity gilliam autism rating scale (GARS) in diagnosis autism spectrum disorders: Systematic review (Persian)]. The Neuroscience Journal of Shefaye Khatam. 2020; 8(4):80-9. [DOI:10.29252/shefa.8.4.80]
- Penny AM, Waschbusch DA, Klein RM, Corkum P, Eskes G. Developing a measure of sluggish cognitive tempo for children: Content validity, factor structure, and reliability. Psychological Assessment. 2009; 21(3):380-9. [DOI:10.1037/a0016600] [PMID]
- Abdolmohamadi K , Ghadiri Sourman Abadi F, Alimohamadi A, Zareean M. [Psychometric Properties of Sluggish Cognitive Tempo Scale (SCTS) Parent Form among Iranian Children (Persian)]. Quarterly of Educational Measurement. 202; 13(47):95-111.
- Owens J, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep: Journal of Sleep Research & Sleep Medicine. 2000; 23(8):1-9. [DOI:10.1093/sleep/23.8.1d]
- Shoghy M, Khanjari S, Farmany F, Hosseini F. [Sleep habits of school age children (Persian)]. Iran Journal of Nursing. 2005; 18(41-42):131-8. [Link]
- Coolidge FL, Thede LL, Stewart SE, Segal DL. The Coolidge Personality and Neuropsychological Inventory for Children (CPNI). Preliminary psychometric characteristics. Behavior Modification. 2002; 26(4):550-66. [DOI:10.1177/0145445502026004007] [PMID]
- Alizadeh H, Zahedipour M. [Executive functions in children with and without developmental coordination disorder (Persian)]. Advances in Cognitive Science. 2005; 6(3-4):49-56. [Link]
- Nobel E, Brunnekreef JA, Schachar RJ, van den Hoofdakker BJ, Hoekstra PJ. Parent-clinician agreement in rating the presence and severity of attention-deficit/hyperactivity disorder symptoms. Attention Deficit and Hyperactivity Disorders. 2019; 11(1):21-9. [DOI:10.1007/s12402-018-0267-8] [PMID]
- Sadrossadat L, Hooshyari Z, Sadrossadat SJ, Mohammadi MR, Rouzbahani A, Shirmardi A. Determination of Psychometrics Indices of SNAP-IV Rating Scale in Teachers Execution. Journal of Isfahan Medical School. 2010; 28(110). [Link]
- Burns GL, Becker SP, Servera M, Bernad MD, García-Banda G. Sluggish cognitive tempo and attention-deficit/hyperactivity disorder (ADHD) inattention in the home and school contexts: Parent and teacher invariance and cross-setting validity. Psychological Assessment. 2017; 29(2):209-20. [DOI:10.1037/pas0000325] [PMID]
- Meyers LS, Gamst G, Guarino AJ. Applied multivariate research: Design and interpretation. California: Sage Publications; 2016. [DOI:10.4135/9781071802687]
- Watabe Y, Owens JS, Evans SW, Brandt NE. The relationship between sluggish cognitive tempo and impairment in children with and without ADHD. Journal of Abnormal Child Psychology. 2014; 42(1):105-15. [DOI:10.1007/s10802-013-9767-3] [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/09/15 | Accepted: 2025/05/26 | Published: 2025/08/1
Received: 2024/09/15 | Accepted: 2025/05/26 | Published: 2025/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |