Tue, Dec 9, 2025
| فارسی
Volume 30, Issue 1 (Continuously Updated 2024)
IJPCP 2024, 30(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Farokhnezhad Afshar P, Saei R, Mehri A. Comparing the Stroop Test Scores Between Older Adults With and Without Sleep Problems in Maragheh, Iran. IJPCP 2024; 30 (1) : 2822.5
URL: http://ijpcp.iums.ac.ir/article-1-4151-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4151-en.html
1- Geriatric Mental Health Research Center, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
2- Department of Geriatric Health, Geriatric Mental Health Research Center, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran. ,saei6917@gmail.com
3- Department of Speech Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Geriatric Health, Geriatric Mental Health Research Center, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran. ,
3- Department of Speech Therapy, School of Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran.
Keywords: Aged, Sleep quality, Executive functions, Attention, Inhibitory control, Cognitive flexibility
Full-Text [PDF 3506 kb]
(958 Downloads)
| Abstract (HTML) (2512 Views)
Full-Text: (666 Views)
Introduction
The aging population in the world is increasing due to medical advances and reduced mortality. It is expected that the number of older people will increase from 840 million in 2013 to 2 billion by 2050 [1]. Ageing can negative affect cognitive processes and executive functions. Impairment of executive functions has a negative effect on older people’s lives [4]. The prevalence of cognitive impairments is 1.5-41% in older adults [5]. Many factors can affect executive functions, one of which is sleep quality. Sleep is needed for restoring energy and repair, recovery, and protecting the brain [8]. It is not well understood what executive functions are affected by sleep and more research is needed. Considering the negative effect of aging on the sleep process and given the importance of sleep for cognitive processes and executive functions, this study aims to compare the Stroop test score of older adults with and without sleep problems.
Methods
This is a descriptive cross-sectional study. The study population consists of older adults referred to the adult day care center in Maragheh City, East Azerbaijan province, Iran. Inclusion criteria were age over 60 years, at least a reading and writing literacy, and no mental health problems according to medical records. The exclusion criteria were the depressive symptoms and neurological disorders based on medical records. Participants were divided into two groups of without sleep problems (n=42) and with sleep problems (n=58) based on the Pittsburgh sleep quality index (PSQI) score (a PSQI score 6≤). Due to the long duration of the tests and time constraints, 16 seniors from the group without sleep problems left the study and the sample size was 42 people.
The data were collected using a demographic information form, Stroop test, and PSQI. Stroop test can measure inhibitory control, selective attention, and cognition flexibility. This test has a computerized version including four types of color (red, blue, yellow, and green) and words. The first list includes words with the same meaning and color. The second list includes the words with different meaning and color. The third list includes the words with incongruent meanings and colors. This test has three parameters including the percentage of correct answers, the percentage of incorrect answers, and response time. The PSQI measures sleep quality and has 18 items with a total score ranged from 0 to 21; a score 6≤ indicates sleep quality problems [17].
After collecting data, they were analyzed in SPSS software, version 24. Independent t-test and analysis of variance were used to compare two study groups and the male and female groups. Pearson’s correlation test was used to examine the correlation between the Stroop test score and age and body mass index (BMI). Chi-square test was used to compare the two groups in terms of demographic variables. The significance level was set 0.05.
Results
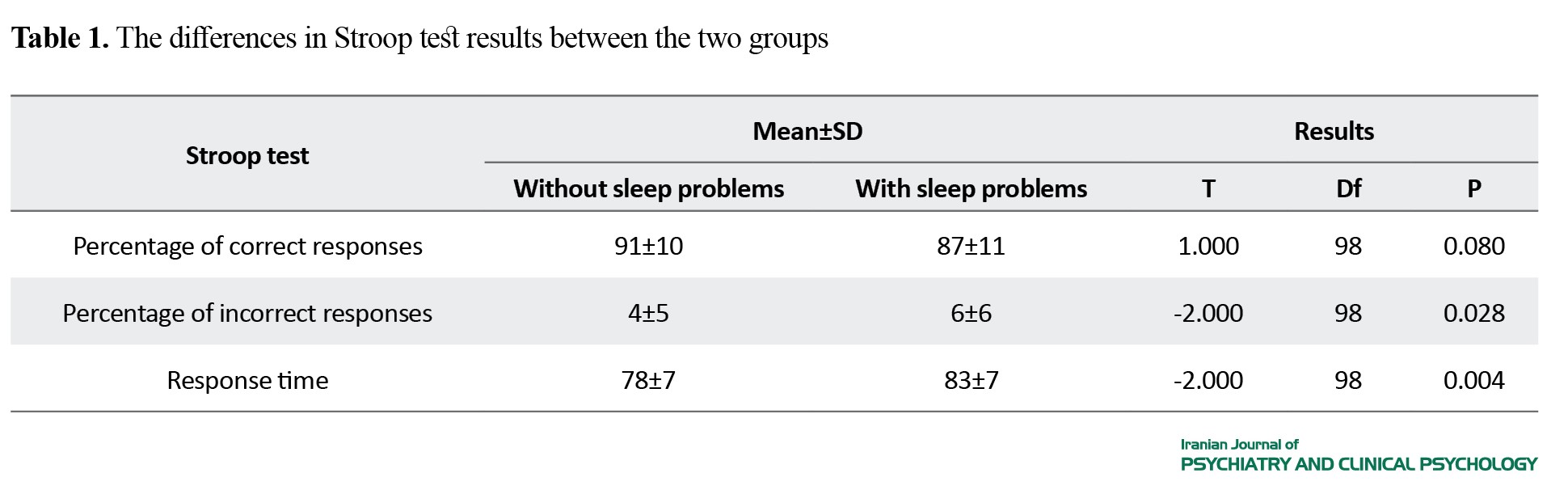
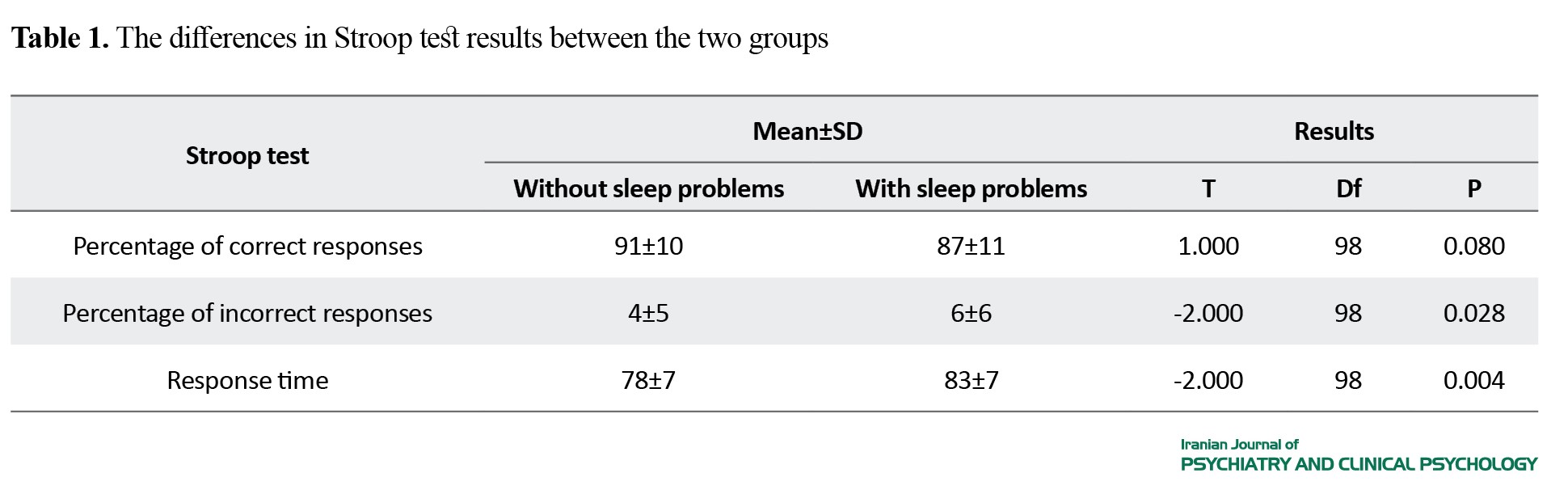
Participants included 100 older adults, 75 women and 25 men. The mean age of older adults without sleep problems was 67 years, while it was 66 years for older adults with sleep problems. In the Stroop test, the results showed that the mean difference was significant in the percentage of incorrect answers (P=0.028) and response time (P=0.004) between the two groups. The difference in the percentage of correct answers was not significant (P=0.080) (Table 1).
There was a significant relationship between age and Stroop test score (P<0.001), but there was no significant relationship between BMI and Stroop test.
Conclusion
The present study showed that the percentage of incorrect responses and response time in Stroop test were significantly different between older adults with and without sleep problems. There are impaired inhibitory control and selective attention in older adults with sleep problems. Therefore, sleep quality may be one of the factors affecting executive functions in older adults. There was no significant difference between the two groups in the percentage of correct answers in the Stroop test.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.767). The study objectives were explained to the participants and their informed consent was obtained.
Funding
This study was funded by the Geriatric Mental Health Research Center of Iran University of Medical Sciences.
Authors contributions
Writing: Roghayeh Saei, Pouya Farokhnezhad Afshar; Editing & review: Pouya Farokhnezhad Afshar and Azar Mehri; Read and approved the final draft: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the seniors participated in this research for their cooperation.
References
The aging population in the world is increasing due to medical advances and reduced mortality. It is expected that the number of older people will increase from 840 million in 2013 to 2 billion by 2050 [1]. Ageing can negative affect cognitive processes and executive functions. Impairment of executive functions has a negative effect on older people’s lives [4]. The prevalence of cognitive impairments is 1.5-41% in older adults [5]. Many factors can affect executive functions, one of which is sleep quality. Sleep is needed for restoring energy and repair, recovery, and protecting the brain [8]. It is not well understood what executive functions are affected by sleep and more research is needed. Considering the negative effect of aging on the sleep process and given the importance of sleep for cognitive processes and executive functions, this study aims to compare the Stroop test score of older adults with and without sleep problems.
Methods
This is a descriptive cross-sectional study. The study population consists of older adults referred to the adult day care center in Maragheh City, East Azerbaijan province, Iran. Inclusion criteria were age over 60 years, at least a reading and writing literacy, and no mental health problems according to medical records. The exclusion criteria were the depressive symptoms and neurological disorders based on medical records. Participants were divided into two groups of without sleep problems (n=42) and with sleep problems (n=58) based on the Pittsburgh sleep quality index (PSQI) score (a PSQI score 6≤). Due to the long duration of the tests and time constraints, 16 seniors from the group without sleep problems left the study and the sample size was 42 people.
The data were collected using a demographic information form, Stroop test, and PSQI. Stroop test can measure inhibitory control, selective attention, and cognition flexibility. This test has a computerized version including four types of color (red, blue, yellow, and green) and words. The first list includes words with the same meaning and color. The second list includes the words with different meaning and color. The third list includes the words with incongruent meanings and colors. This test has three parameters including the percentage of correct answers, the percentage of incorrect answers, and response time. The PSQI measures sleep quality and has 18 items with a total score ranged from 0 to 21; a score 6≤ indicates sleep quality problems [17].
After collecting data, they were analyzed in SPSS software, version 24. Independent t-test and analysis of variance were used to compare two study groups and the male and female groups. Pearson’s correlation test was used to examine the correlation between the Stroop test score and age and body mass index (BMI). Chi-square test was used to compare the two groups in terms of demographic variables. The significance level was set 0.05.
Results
Participants included 100 older adults, 75 women and 25 men. The mean age of older adults without sleep problems was 67 years, while it was 66 years for older adults with sleep problems. In the Stroop test, the results showed that the mean difference was significant in the percentage of incorrect answers (P=0.028) and response time (P=0.004) between the two groups. The difference in the percentage of correct answers was not significant (P=0.080) (Table 1).
There was a significant relationship between age and Stroop test score (P<0.001), but there was no significant relationship between BMI and Stroop test.
Conclusion
The present study showed that the percentage of incorrect responses and response time in Stroop test were significantly different between older adults with and without sleep problems. There are impaired inhibitory control and selective attention in older adults with sleep problems. Therefore, sleep quality may be one of the factors affecting executive functions in older adults. There was no significant difference between the two groups in the percentage of correct answers in the Stroop test.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.767). The study objectives were explained to the participants and their informed consent was obtained.
Funding
This study was funded by the Geriatric Mental Health Research Center of Iran University of Medical Sciences.
Authors contributions
Writing: Roghayeh Saei, Pouya Farokhnezhad Afshar; Editing & review: Pouya Farokhnezhad Afshar and Azar Mehri; Read and approved the final draft: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the seniors participated in this research for their cooperation.
References
- Han J, Zhang X, Meng Y. The impact of old-age pensions on the happiness level of elderly people-evidence from China. Ageing & Society. 2022; 42(5):1079-99. [DOI:10.1017/S0144686X20001452]
- Mehri N, Messkoub M, Kunkel S. Trends, determinants and the implications of population aging in Iran. Ageing International. 2020;45(4):327-43. [DOI:10.1007/s12126-020-09364-z]
- Aghamohamadi S, Hajinabi K, Jahangiri K, Asl IM, Dehnavieh R. Population and mortality profile in the Islamic Republic of Iran, 2006-2035. Eastern Mediterranean Health Journal. 2018; 24(5):469-76. [DOI:10.26719/2018.24.5.469] [PMID]
- Mayer RE, Parong J, Bainbridge K. Young adults learning executive function skills by playing focused video games. Cognitive Development. 2019; 49:43-50. [DOI:10.1016/j.cogdev.2018.11.002]
- Pais R, Ruano L, O PC, Barros H. Global cognitive impairment prevalence and incidence in community dwelling older adults-A systematic review. Geriatrics (Basel). 2020; 5(4):84. [DOI:10.3390/geriatrics5040084] [PMID]
- Kheirkhah F, Hosseini SR, Fallah R, Bijani A. [Prevalence of cognitive disorders in elderly people of Amirkola (2011-2012) (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2014; 19(4):247-54. [Link]
- Tajrishi K, Besharat MA, Pourbohlool S, Larijani R. Psychometric properties of a Farsi version of the Basic Needs Satisfaction in General Scale in a sample of Iranian population. Procedia - Social and Behavioral Sciences. 2011; 30:221-5. [DOI:10.1016/j.sbspro.2011.10.044]
- Ghaemi F, Rostami R, Mirkamali SM, Salehi K. [Systematic and analytical review of theories, components and models of executive functions of the brain (Persian)]. Rooyesh-e-Ravanshenasi Journal(RRJ). 2021; 10(6):211-26. [Link]
- Killgore WDS, Vanuk JR, Shane BR, Weber M, Bajaj S. A randomized, double-blind, placebo-controlled trial of blue wavelength light exposure on sleep and recovery of brain structure, function, and cognition following mild traumatic brain injury. Neurobiology of Disease. 2020; 134:104679. [DOI:10.1016/j.nbd.2019.104679][PMID]
- Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. International Journal of Nursing Practice. 2013; 19(2):116-23. [DOI:10.1111/ijn.12047] [PMID]
- Papi S, Karimi Z, Ghaed Amini Harooni G, Nazarpour A, Shahry P. [Determining the prevalence of sleep disorder and its predictors among elderly residents of nursing homes of Ahvaz City in 2017 (Persian)]. Salmand: Iranian Journal of Ageing. 2019; 13(5):576-87. [DOI:10.32598/SIJA.13.Special-Issue.576]
- Azadian B, Yousefi Rezaii T, Meshgini S. [Exploiting sparse representation for sleep stage classification using electroencephalogram signal (Persian)]. Advanced Signal Processing. 2019; 3(1):1-11. [Link]
- Saadati H, Sheibani V, Refahi S, Mashhadi Z. [A review of the effects of sleep deprivation on learning and memory: The role of sex hormones (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2018; 17(4):359-76. [Link]
- Izadi Avanji FS, Adib Hajbaghery M, Afazel MR. [Quality of sleep and it’s related factors in the hospitalized elderly patients of Kashan hospitals in 2007 (Persian)]. Feyz Medical Sciences Journal. 2009; 12(4):52-60. [Link]
- Jabarzadeh Chaharbarod M, Bayrami M, Nakhostin Goldoost A, Hashemi T. [The effectiveness of cognitive empowerment on executive functions and cognitive and emotional inhibition of students with learning disabilities (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2022; 65(1). [DOI:10.22038/mjms.2022.22710]
- Faria LO, Frois T, Fortes LS, Bertola L, Albuquerque MR. Evaluating the Stroop Test with older adults: Construct validity, short term test-retest reliability, and sensitivity to mental fatigue. Perceptual and Motor Skills. 2024; 131(4):1120-44.[DOI:10.1177/00315125241253425]
- Sadri Damirchi E, Behbuei S, Mojarrad A. [Role of performance in the stroop test in anticipation of anxiety and aggression in the elderly in Ardabil (Persian)]. Salmand: Iranian Journal of Ageing. 2018; 13(1):38-49. [DOI:10.21859/sija.13.1.38]
- Zare S. [Evaluation of sleep quality in bus drivers in Tehran (Persian)]. Traffic Management Studies. 2010; 5:1-10. [Link]
- Sepehrmanesh Z, Moraveji A, kalantar Mehrjarid F. The relationship between mental health and sleep quality in students of Kashan University of Medical Sciences in the academic year of 1994-93. Occupational Medicine Quarterly Journal. 2023; 14(4):36-45. [DOI:10.18502/tkj.v14i4.12312]
- Rahmani K, Ebrahimi M, Abdi N. [Assessment of general health and sleep quality of nurses in educational hospitals of Kurdistan University of Medical Sciences, 2018 (Persian)]. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2020; 6(2):31-42. [Link]
- Khodadadi M, Feyzi Daryati MR, Movahedi Y, Ahmadi I. [Assessment of attention bias in the cognitive processing of neutral and emotional words using semantic strop test (Persian)]. Shenakht Journal of Psychology and Psychiatry. 2014; 1(1):23-30.[Link]
- Jasemi Zargan E, Sotoudeh Asl N, Moazedian A, Jahan F. [The effectiveness of metacognitive therapy and transcranial direct current stimulation on executive functions of stroop and tower of London in veterans with post-traumatic stress disorder (Persian)]. Neuropsychology. 2021; 7(25):29-42. [DOI:10.30473/clpsy.2020.55099.1569]
- Honn KA, Hinson JM, Whitney P, Van Dongen HPA. Cognitive flexibility: A distinct element of performance impairment due to sleep deprivation. Accident Analysis & Prevention. 2019; 126:191-7. [DOI:10.1016/j.aap.2018.02.013] [PMID]
- Liao H, Liao S, Gao YJ, Mu JP, Wang X, Chen DS. Correlation between sleep time, sleep quality, and emotional and cognitive function in the elderly. BioMed Research International. 2022; 2022; 2022:9709536. [DOI:10.1155/2022/9709536] [PMID]
- Unsal P, Sengul Aycicek G, Deniz O, Esme M, Dikmeer A, Balcı C, et al. Insomnia and falls in older adults: Are they linked to executive dysfunction? Psychogeriatrics. 2021; 21(3):359-67. [DOI:10.1111/psyg.12677] [PMID]
- Rodrigues T, Shigaeff N. Sleep disorders and attention: A systematic review. Arquivos de Neuro-Psiquiatria. 2022; 80(5):530-8. [DOI:10.1590/0004-282x-anp-2021-0182] [PMID]
- Eugene AR, Masiak J. The neuroprotective aspects of sleep. MEDtube Science. 2015; 3(1):35-40. [PMID]
- Mirzakhani M, Gharraee B, Zahedi Tajrishi K, Khanjani S, Noorbala AA, Safaei Nodehi SR. [Effect of compassion-focused therapy on depression, anxiety, stress, and quality of life in patients with cancer: A clinical trial (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2023; 29(2):142-55. [Link]
- Ferguson SA, Appleton SL, Reynolds AC, Gill TK, Taylor AW, McEvoy RD, et al. Making errors at work due to sleepiness or sleep problems is not confined to non-standard work hours: results of the 2016 Sleep Health Foundation national survey. Chronobiology International. 2019; 36(6):758-69. [DOI:10.1080/07420528.2019.1578969] [PMID]
- Takeuchi H, Taki Y, Sassa Y, Hashizume H, Sekiguchi A, Fukushima A, et al. Brain structures associated with executive functions during everyday events in a non-clinical sample. Brain Structure & Function. 2013; 218(4):1017-32. [DOI:10.1007/s00429-012-0444-z] [PMID]
- Verweij IM, Romeijn N, Smit DJ, Piantoni G, Van Someren EJ, van der Werf YD. Sleep deprivation leads to a loss of functional connectivity in frontal brain regions. BMC Neuroscience. 2014; 15:88. [DOI:10.1186/1471-2202-15-88] [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/04/9 | Accepted: 2024/08/12 | Published: 2024/07/31
Received: 2024/04/9 | Accepted: 2024/08/12 | Published: 2024/07/31
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






