Wed, Jul 16, 2025
| فارسی
Volume 29, Issue 4 (Winter 2024)
IJPCP 2024, 29(4): 494-513 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Falahat K, Baradaran Eftekhari M, Mirabzadeh A. Social Determinants of Health for Positive Mental Health of Iranian Adults. IJPCP 2024; 29 (4) :494-513
URL: http://ijpcp.iums.ac.ir/article-1-4041-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4041-en.html
1- Deputy of Research and Technology, Ministry of Health and Medical Education, Tehran, Iran.
2- Deputy of Research and Technology, Ministry of Health and Medical Education, Tehran, Iran. ,mbeftekhari200@gmail.com
3- Department of Social Welfare, School of Social Welfare, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Deputy of Research and Technology, Ministry of Health and Medical Education, Tehran, Iran. ,
3- Department of Social Welfare, School of Social Welfare, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Full-Text [PDF 7070 kb]
(535 Downloads)
| Abstract (HTML) (1620 Views)
Full-Text: (519 Views)
Introduction
According to the World Health Organization (WHO), mental health is more than the absence of mental disorders. It also denotes positive mental health. Based on this view, people with mental disorders may experience different degrees of positive mental health. Various studies have shown that promoting positive mental health can reduce the prevalence, incidence and burden of mental disorders. The social determinants of health (SDH) play important roles in different aspects of health such as mental health or positive mental health. According to the WHO, the SDH include structural and intermediary factors. Education, employment, gender are examples of structural determinants and psychosocial, behavioral and biological factors are among intermediary determinants. Identifying the SDH of positive mental health is necessary to implement interventions for promoting mental health in society. Therefore, the present study aims to identify the SDH of positive mental health in Iranian adults.
Methods
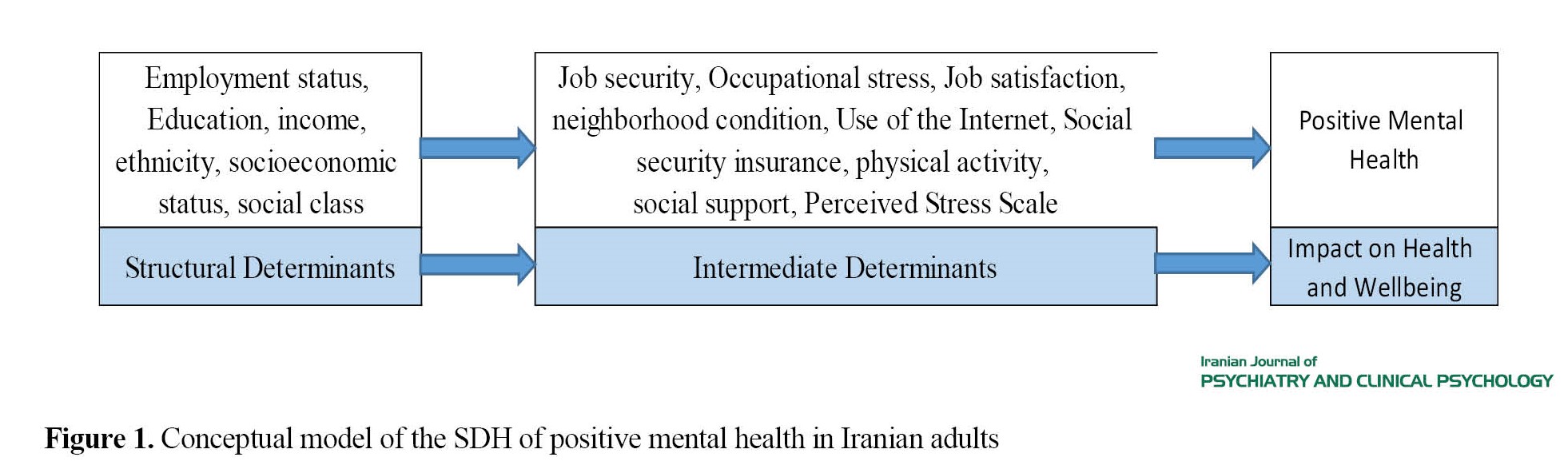
This is a quantitative and correlational study that was conducted on adults aged 30-60 in Tehran, Iran. The sampling method was a multi-stage sampling method including stratified random sampling, cluster sampling, and simple random sampling techniques. The sample size was estimated to be 547 using G*Power software, considering the effect size of 0.12, α=0.05, and P=0.80. To design the conceptual model of the SDH of positive mental health, we first reviewed the literature. Then, by holding a meeting with experts in mental health and SDH as well as people, a list of the SDH of positive mental health was extracted and the conceptual model of the study was plotted (Figure 1). Based on this conceptual model, the structural equation modeling (SEM) was conducted. The data collection tools included the mental health continuum–short form (MHC–SF), the socioeconomic status questionnaire, multidimensional scale of perceived social support, perceived stress scale-10 items, International physical activity questionnaire- short form, Neissi’s job security questionnaire, Ten Horn’s job security questionnaire, visual analogue scale for occupational stress assessment, the neighborhood status checklist, Internet use checklist, and social security insurance checklist. These questionnaires included 117 items that were completed by a self-report method. The collected data were analyzed using SPSS software, vesion 21 and LISREL vesion 8.8. The significant level was set at 0.05.
Results
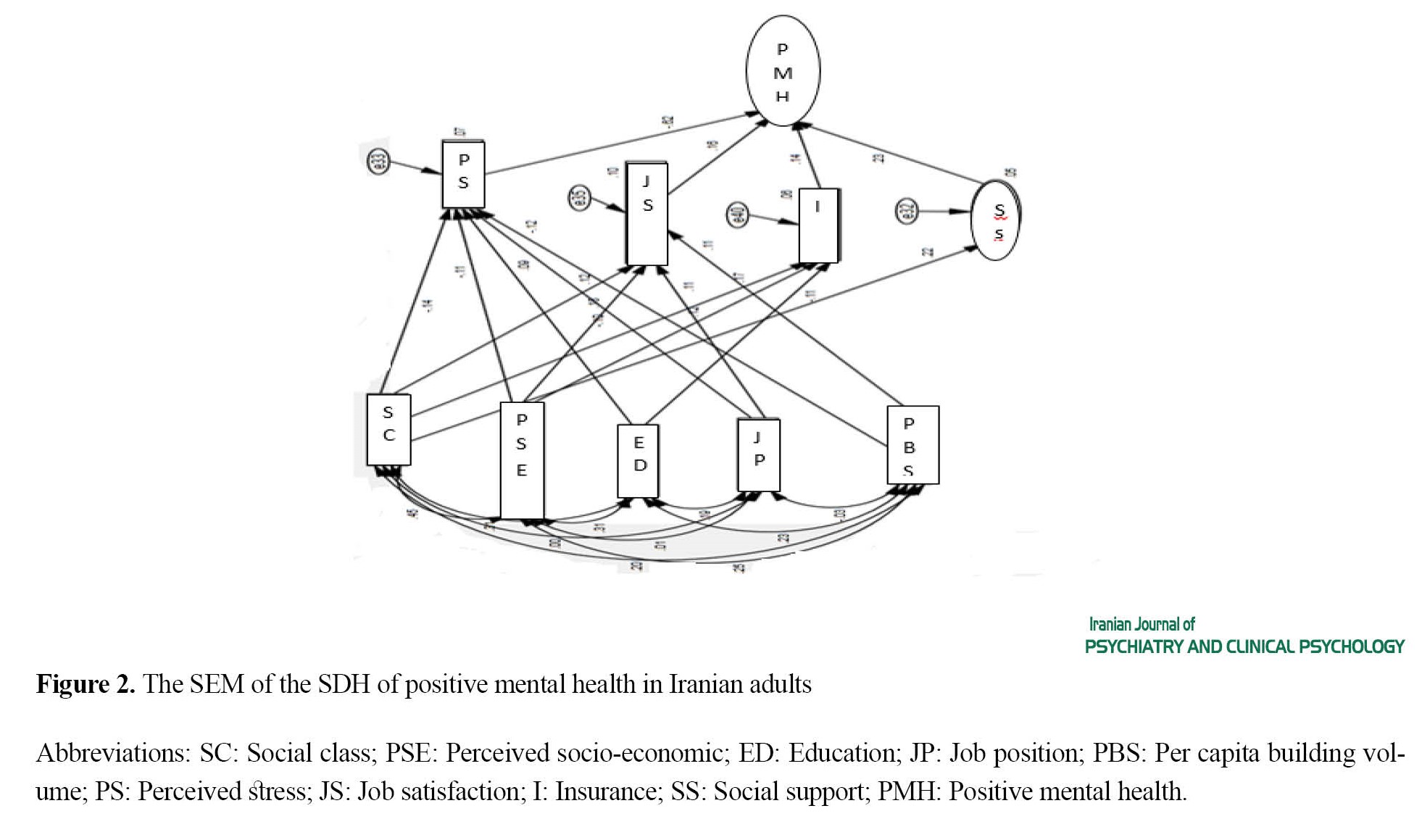
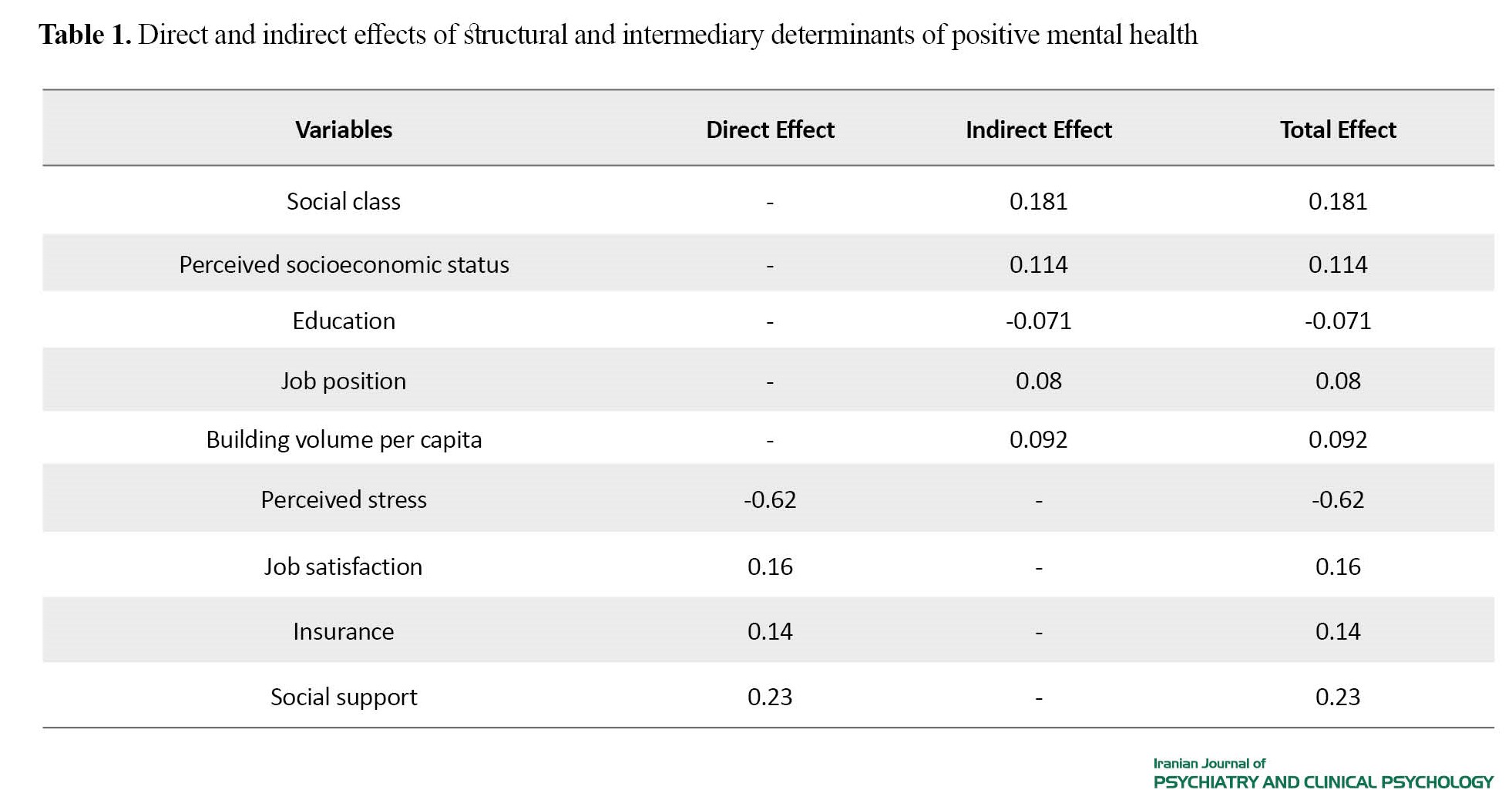
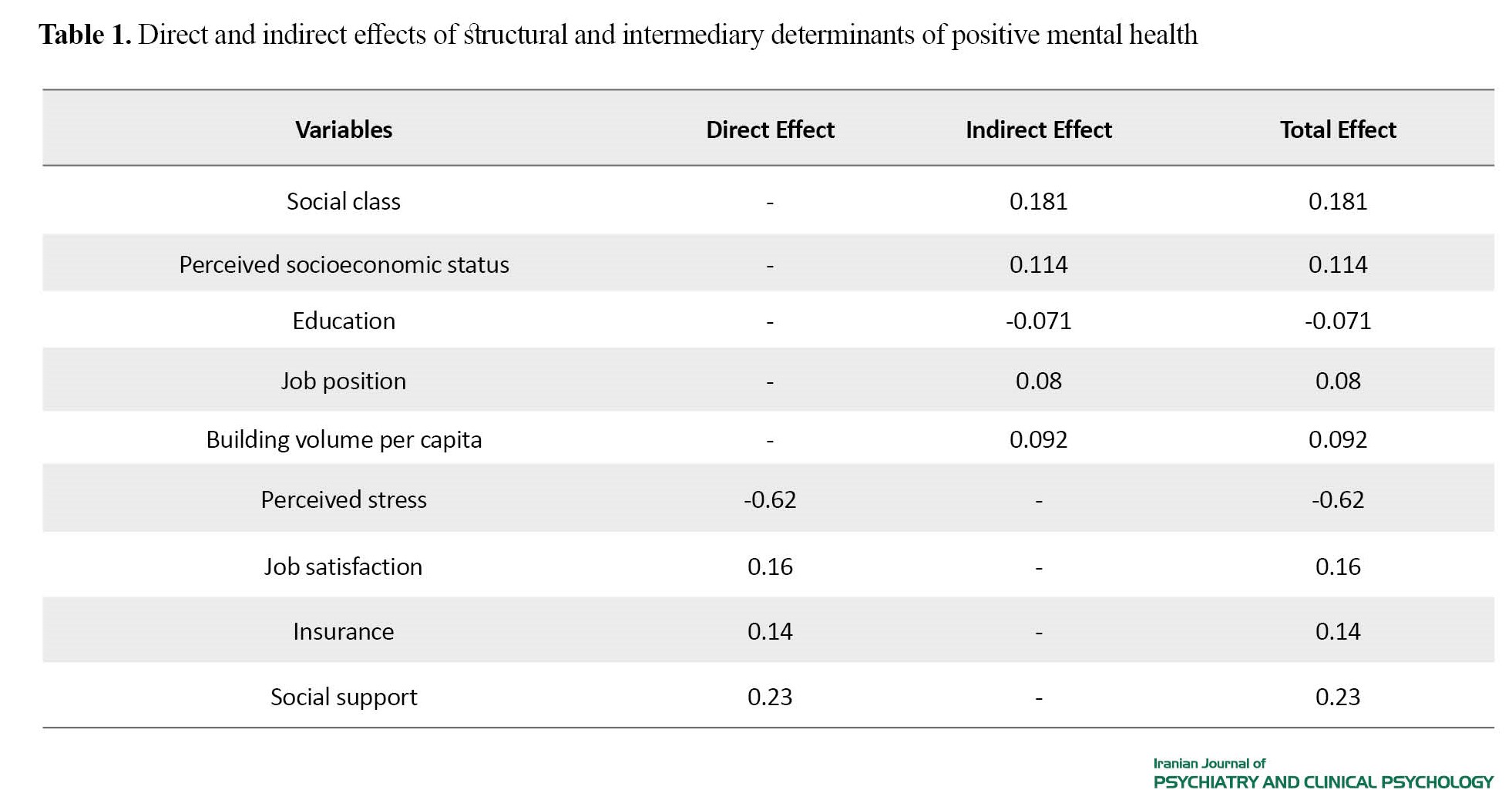
The data of 607 questionnaires were analyzed in this study. Participants were 308 women (50.7%) and 299 men (49.3%) with mean age of 44.04±9.4 years. The mean total score of MHC–SF (positive mental health) was 45.96±8.65. Regarding its domains of emotional, social, and psychological well-being, the scores were 9.8±2.54, 14.22±3.41, and 21.93±4.4, respectively. For conducting SEM, the variables with a significance level (P≥0.2 were entered into the model. The social class (B=0.181), perceived socio-economic status (B=0.114), job position (B=0.08), building volume per capita (B=0.092) and education (B=-0.071) had indirect effect on positive mental health. Perceived stress (B=-0.62), job satisfaction (B=0.16), social support (B=0.23) and insurance (B=0.14) had direct effect on positive mental health. In general, all variables positively explained about 53% of mental health changes (Table 1 and Figure 2).
Conclusion
The structural model of the SDH indicated that perceived stress was the most important intermediary determinant of positive mental health in Iranian adults, which transfers the effect of structural determinants on the positive mental health. Perceived stress had the most direct and negative impact on positive mental health, while social support, job satisfaction and insurance had the most positive and direct effects on positive mental health. Therefore, planning for the implementation of interventions to optimally manage stress of Iranian adults and teaching them how to use adaptive mechanisms to deal with it along with increasing social support for them, strengthening their family foundation, and improving their working conditions and insurance coverage can be effective in improving the positive mental health of Iranian adults.
Ethical Considera tions
Compliance with ethical guidelines
All ethical considerations were considered in this study. The study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1396.204).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization: Monir Baradaran Eftekhari and Arash Mirabzadeh; Methodology: Monir Baradaran Eftekhari and Katayoun Falahat; Data gathering: Katayoun Falahat; Writing: Monir Baradaran Eftekhari.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all participants for their cooperation in this study.
According to the World Health Organization (WHO), mental health is more than the absence of mental disorders. It also denotes positive mental health. Based on this view, people with mental disorders may experience different degrees of positive mental health. Various studies have shown that promoting positive mental health can reduce the prevalence, incidence and burden of mental disorders. The social determinants of health (SDH) play important roles in different aspects of health such as mental health or positive mental health. According to the WHO, the SDH include structural and intermediary factors. Education, employment, gender are examples of structural determinants and psychosocial, behavioral and biological factors are among intermediary determinants. Identifying the SDH of positive mental health is necessary to implement interventions for promoting mental health in society. Therefore, the present study aims to identify the SDH of positive mental health in Iranian adults.
Methods
This is a quantitative and correlational study that was conducted on adults aged 30-60 in Tehran, Iran. The sampling method was a multi-stage sampling method including stratified random sampling, cluster sampling, and simple random sampling techniques. The sample size was estimated to be 547 using G*Power software, considering the effect size of 0.12, α=0.05, and P=0.80. To design the conceptual model of the SDH of positive mental health, we first reviewed the literature. Then, by holding a meeting with experts in mental health and SDH as well as people, a list of the SDH of positive mental health was extracted and the conceptual model of the study was plotted (Figure 1). Based on this conceptual model, the structural equation modeling (SEM) was conducted. The data collection tools included the mental health continuum–short form (MHC–SF), the socioeconomic status questionnaire, multidimensional scale of perceived social support, perceived stress scale-10 items, International physical activity questionnaire- short form, Neissi’s job security questionnaire, Ten Horn’s job security questionnaire, visual analogue scale for occupational stress assessment, the neighborhood status checklist, Internet use checklist, and social security insurance checklist. These questionnaires included 117 items that were completed by a self-report method. The collected data were analyzed using SPSS software, vesion 21 and LISREL vesion 8.8. The significant level was set at 0.05.
Results
The data of 607 questionnaires were analyzed in this study. Participants were 308 women (50.7%) and 299 men (49.3%) with mean age of 44.04±9.4 years. The mean total score of MHC–SF (positive mental health) was 45.96±8.65. Regarding its domains of emotional, social, and psychological well-being, the scores were 9.8±2.54, 14.22±3.41, and 21.93±4.4, respectively. For conducting SEM, the variables with a significance level (P≥0.2 were entered into the model. The social class (B=0.181), perceived socio-economic status (B=0.114), job position (B=0.08), building volume per capita (B=0.092) and education (B=-0.071) had indirect effect on positive mental health. Perceived stress (B=-0.62), job satisfaction (B=0.16), social support (B=0.23) and insurance (B=0.14) had direct effect on positive mental health. In general, all variables positively explained about 53% of mental health changes (Table 1 and Figure 2).
Conclusion
The structural model of the SDH indicated that perceived stress was the most important intermediary determinant of positive mental health in Iranian adults, which transfers the effect of structural determinants on the positive mental health. Perceived stress had the most direct and negative impact on positive mental health, while social support, job satisfaction and insurance had the most positive and direct effects on positive mental health. Therefore, planning for the implementation of interventions to optimally manage stress of Iranian adults and teaching them how to use adaptive mechanisms to deal with it along with increasing social support for them, strengthening their family foundation, and improving their working conditions and insurance coverage can be effective in improving the positive mental health of Iranian adults.
Ethical Considera tions
Compliance with ethical guidelines
All ethical considerations were considered in this study. The study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1396.204).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization: Monir Baradaran Eftekhari and Arash Mirabzadeh; Methodology: Monir Baradaran Eftekhari and Katayoun Falahat; Data gathering: Katayoun Falahat; Writing: Monir Baradaran Eftekhari.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all participants for their cooperation in this study.
- Friedli L. Mental health, resilience and inequalities. Copenhagen: WHO Regional Office for Europe; 2009. [DOI:10.1016/S0924-9338(12)74077-4]
- Kraiss J, Redelinghuys K, Weiss LA. The effects of psychological interventions on well-being measured with the mental health continuum: A meta-analysis. Journal of Happiness Studies. 2022; 23:3655-89. [DOI:10.1007/s10902-022-00545-y]
- Gilmour H. Positive mental health and mental illness. Health Reports. 2014; 25(9):3-9. [PMID]
- Nosratabadi M, Joshanloo M, Mohammadi F, Shahmohammadi K. [Are Iranian students flourishing? (Persian)]. Developmental Psychology. 2010; 7(25):83-94. [Link]
- Fuller-Thomson E, Lung Y, West KJ, Keyes CLM, Baiden P. Suboptimal baseline mental health associated with 4-month premature all-cause mortality: Findings from 18 years of follow-up of the Canadian national population health survey. Journal of Psychosomatic Research. 2020; 136:110176 [DOI:10.1016/j.jpsychores.2020.110176] [PMID]
- Keyes CLM, Yao J, Hybels CF, Milstein G, Proeschold-Bell RJ. Are changes in positive mental health associated with increased likelihood of depression over a two year period? A test of the mental health promotion and protection hypotheses. Journal of Affective Disorders. 2020; 270:136-42. [DOI:10.1016/j.jad.2020.03.056] [PMID]
- Solar O, Irwin A. A conceptual framework for action on the social determinants of health. WHO Document Production Services; 2010. [Link]
- Owusu-Addo E, Renzaho AMN, Smith BJ. Cash transfers and the social determinants of health: A conceptual framework. Health Promotion International. 2019; 34(6):e106-18. [DOI:10.1093/heapro/day079] [PMID]
- Kading ML, Hautala DS, Palombi LC, Aronson BD, Smith RC, Walls ML. Flourishing: American Indian positive mental health. Society and Mental Health. 2015; 5(3):203-17. [DOI:10.1177/2156869315570480] [PMID]
- Mokhayeri Y, Mahmoudi M, Haghdoost AA, Amini H, Asadi-Lari M, Holakouie Naieni K. How within-city socioeconomic disparities affect life expectancy? Results of urban heart in Tehran, Iran. Medical Journal of the Islamic Republic of Iran. 2014; 28:80. [PMID]
- Munro, B.H., Statistical methods for health care research. Volume 1. Philadelphia: Lippincott Williams & Wilkins; 2005. [Link]
- Falahat K, Mirabzadeh A, Eftekhari MB, Sajjadi H, Vameghi M, Harouni GG, et al. Social determinants of positive mental health in Iranian Society: A qualitative approach. International Journal of Preventive Medicine. 2019; 10:170. [DOI:10.4103/ijpvm.IJPVM_94_18] [PMID]
- Guetterman TC. Basics of statistics for primary care research: Family Medicine and community Health. 2019; 7(2):e000067. [PMID]
- Joshanloo M, Wissing MP, Khumalo IP, Lamers SM. Measurement invariance of the Mental Health Continuum-Short Form (MHC-SF) across three cultural groups. Personality and Individual Differences. 2013; 55(7):755-9. [DOI:10.1016/j.paid.2013.06.002]
- Cohen S, Alper CM, Doyle WJ, Adler N, Treanor JJ, Turner RB. Objective and subjective socioeconomic status and susceptibility to the common cold. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2008; 27(2):268-74. [DOI:10.1037/0278-6133.27.2.268] [PMID]
- Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment. 1990; 55(3-4):610-7. [DOI:10.1080/00223891.1990.9674095] [PMID]
- Bagherian-Sararoudi R, Hajian A, Ehsan HB, Sarafraz MR, Zimet GD. Psychometric properties of the Persian version of the Multidimensional Scale of Perceived Social Support in Iran. International Journal of Preventive Medicine. 2013; 4(11):1277-81. [PMID]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983; 24(4):385-96. [DOI:10.2307/2136404] [PMID]
- Cohen S, Kamarck T, Mermelstein R. Measuring stress: A guide for health Perceived Stress Scale. 1994. [Link]
- Bastianon CD, Klein EM, Tibubos AN, Brähler E, Beutel ME, Petrowski K. Perceived Stress Scale (PSS-10) psychometric properties in migrants and native Germans. BMC Psychiatry. 2020; 20(1):450. [DOI:10.1186/s12888-020-02851-2] [PMID]
- Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2011; 8:115. [DOI:10.1186/1479-5868-8-115] [PMID]
- Hazavehei SMM, Asadi Z, Hassanzadeh A, Shekarchizadeh P. [Comparing the effect of two methods of presenting physical education 2 course on the attitudes and practices of female students towards regular physical activity in Isfahan University of Medical Sciences (Persian)]. Iranian Journal of Medical Education. 2008; 8(1):121-31. [Link]
- Ariamanesh M, Sadoughi M. [Investigating the intellectual capital and job security of employees and their role in reducing organizational evasion (Persian)]. Journal of Management and Sustainable Development Studies. 2023; 3(2):101-23. [DOI:10.30495/MSDS.2023.1983686.1135]
- Zinovieva IL, Ten Horn LA, Roe RA.Work motivation under forced transition. (WORC Paper 93.01.001/6. Paper presented at: 6th European Congress on Work and Organizational Psychology. 14-17 April 1993; Alicante, Spain. [Link]
- Lesage FX, Berjot S. Validity of occupational stress assessment using a visual analogue scale. Occupational Medicine (Oxford, England). 2011; 61(6):434-6. [DOI:10.1093/occmed/kqr037] [PMID]
- Dutheil F, Pereira B, Moustafa F, Naughton G, Lesage FX, Lambert C. At-risk and intervention thresholds of occupational stress using a visual analogue scale. Plos One. 2017; 12(6):e0178948. [PMID]
- Bruce N, Pope D, Stanistreet D. Quantitative methods for health research: A practical interactive guide to epidemiology and statistics. New Jersey: John Wiley & Sons; 2018. [DOI:10.1002/9781118665374]
- Rubin M, Stuart R. Kill or cure? Different types of social class identification amplify and buffer the relation between social class and mental health. The Journal of Social Psychology. 2018; 158(2):236-51. [DOI:10.1080/00224545.2017.1327405] [PMID]
- Harandi TF, Taghinasab MM, Nayeri TD. The correlation of social support with mental health: A meta-analysis. Electronic Physician. 2017; 9(9):5212-22. [DOI:10.19082/5212] [PMID]
- Descary G, Dupéré V, T Hebert S, Schoon I. Is academic agency relevant for the school-to-work transition of lower attainers? Evidence from Canada and England. Journal of Youth and Adolescence. 2023; 52(12):2509-25. [DOI:10.1007/s10964-023-01843-1] [PMID]
- Muntaner C. Global precarious employment and health inequalities: Working conditions, social class, or precariat? Cad Saúde Pública. 2016; 32(6):e00162215. [DOI:10.1590/0102-311X00162215]
- Donkin A, Goldblatt P, Allen J, Nathanson V, Marmot M. Global action on the social determinants of health. BMJ Global Health. 2017; 3(Suppl 1):e000603. [DOI:10.1136/bmjgh-2017-000603] [PMID]
- Woodward EN, Walsh JL, Senn TE, Carey MP. Positive social interaction offsets impact of low socioeconomic status on stress. Journal of the National Medical Association. 2018; 110(4):371-7. [DOI:10.1016/j.jnma.2017.07.006] [PMID]
- Judge TA, Weiss HM, Kammeyer-Mueller JD, Hulin CL. Job attitudes, job satisfaction, and job affect: A century of continuity and of change. Journal of Applied Psychology. 2017; 102(3):356-74. [DOI:10.1037/apl0000181] [PMID]
- Ngirande H. Occupational stress, uncertainty and organizational commitment in higher education: Job satisfaction as a moderator. SA Journal of Human Resource Management. 2024; 19:a1376. [DOI:10.4102/sajhrm.v19i0.1376]
- De Moortel D, Palència L, Artazcoz L, Borrell C, Vanroelen C. Neo-Marxian social class inequalities in the mental well-being of employed men and women: The role of European welfare regimes. Social Science & Medicine. 2015; 128:188-200. [DOI:10.1016/j.socscimed.2015.01.027] [PMID]
- Banerjee N, Chatterjee I. Academic stress, suicidal ideation & mental well-being among 1st semester & 3rd semester medical, engineering & general stream students. Researchers World - International Refereed Social Sciences Journal. 2016; 7(3):73-80. [DOI:10.18843/rwjasc/v7i3/09]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2023/10/16 | Accepted: 2023/12/6 | Published: 2023/12/31
Received: 2023/10/16 | Accepted: 2023/12/6 | Published: 2023/12/31
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |