Sun, Aug 24, 2025
| فارسی
Volume 27, Issue 1 (Spring 2021)
IJPCP 2021, 27(1): 104-119 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Malakouti S K, Keshavarz Akhlaghi A, Shirzad F, Rashedi V, Khlafbeigi M, Moradi Lakeh M et al . Urban Mental Health Initiative: Developing Interdisciplinary Collaboration, the Role of the Family Physician in Management of Severe Mentally Ill Patients. IJPCP 2021; 27 (1) :104-119
URL: http://ijpcp.iums.ac.ir/article-1-3130-en.html
URL: http://ijpcp.iums.ac.ir/article-1-3130-en.html
Seyed Kazem Malakouti1 

 , Amirabbas Keshavarz Akhlaghi2
, Amirabbas Keshavarz Akhlaghi2 

 , Fatemeh Shirzad3
, Fatemeh Shirzad3 

 , Vahid Rashedi4
, Vahid Rashedi4 

 , Mitra Khlafbeigi5
, Mitra Khlafbeigi5 

 , Maziar Moradi Lakeh6
, Maziar Moradi Lakeh6 

 , Ahmad Hajebi7
, Ahmad Hajebi7 




 , Amirabbas Keshavarz Akhlaghi2
, Amirabbas Keshavarz Akhlaghi2 

 , Fatemeh Shirzad3
, Fatemeh Shirzad3 

 , Vahid Rashedi4
, Vahid Rashedi4 

 , Mitra Khlafbeigi5
, Mitra Khlafbeigi5 

 , Maziar Moradi Lakeh6
, Maziar Moradi Lakeh6 

 , Ahmad Hajebi7
, Ahmad Hajebi7 


1- Mental Health Research Center, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
2- Mental Health Research Center, Iran University of Medical Sciences, Tehran, Iran.
3- Spiritual Health Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
5- Department of Occupational Therapy, School of Rehabilitation Sceinces, Iran University of Medical Sceinces, Tehran, Iran.
6- Family Health Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
7- Department of Psychiatry, Research Center for Addiction and Risky Behaviors (ReCARB), Iran University of Medical Sciences, Tehran, Iran. ,hajebi.a@iums.ac.ir
2- Mental Health Research Center, Iran University of Medical Sciences, Tehran, Iran.
3- Spiritual Health Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
5- Department of Occupational Therapy, School of Rehabilitation Sceinces, Iran University of Medical Sceinces, Tehran, Iran.
6- Family Health Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
7- Department of Psychiatry, Research Center for Addiction and Risky Behaviors (ReCARB), Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 6386 kb]
(1684 Downloads)
| Abstract (HTML) (3794 Views)
Full-Text: (2687 Views)
1. Introduction
Studies on the integratation of mental health into primary health care in Iran have been conducted since 1986, which was later implemented successfully within the Rural Family Physician Program in 1988. In urban areas, there is no structured mental health care system and the private sector provides health care services mostly focused on the biomedical model of care. Due to demographic changes in Iran’s population, urban sprawl, and the changes in the urban/rural proportion, the need for a coherent plan to provide mental health services in urban areas is felt more than ever. This study aims to investigate the feasibility of establishing the urban mental health care system for patients with severe psychiatric diseases based on collaboration between organizations in Iran.
2. Materials and Methods
The study reviews the integrated plan for urban mental health services in Iran. First, a systematic review was conducted to get acquainted with the models of providing urban mental health services worldwide, including the World Health Organization (WHO)’s model in the field of mental health care. Then, the situational analysis of the services provided in Iran was carried out using the WHO Assessment Instrument for Mental Health Systems (WHO-AIMS). Legal duties of beneficiary organizations, and the Inter-sectoral collaboration of the Ministry of Health and beneficiary organizations were reviewed along with seeking for the opinions of international and national experts using the Delphi method. The model estimates the need for mental health services in cities with 100,000 population.
3. Results
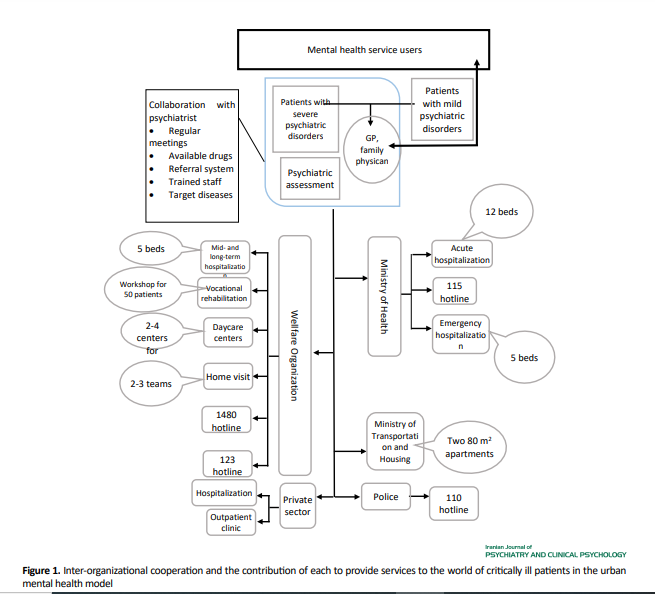
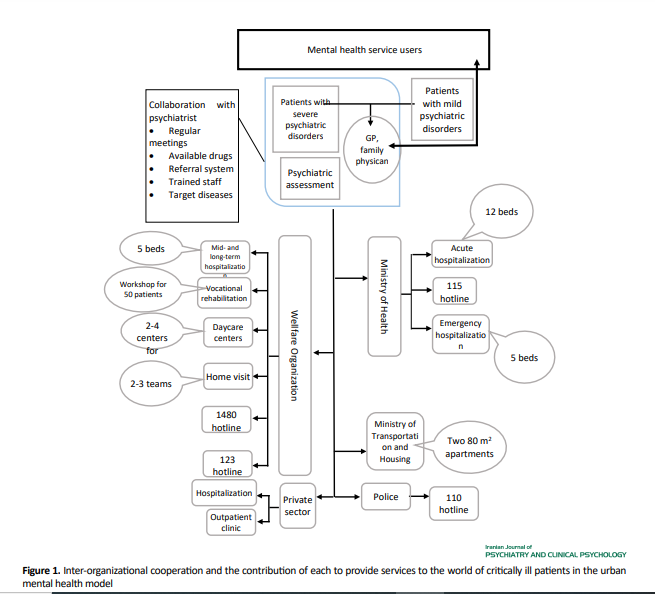
The prevalence of mental diseases in Iran was similar to the global rate. The most prevalent mental disease was major depressive disorder followed by substance abuse. The number of male and female patients with mental diseases was not equal. The proposed model was mainly for severe mental diseases such as severe depression, bipolar mood disorder, and the spectrum of psychotic disorders that account for the highest number of admissions to psychiatric hospitals. According to the results of the literature review and based on the opinions of experts, the urban mental health care system should provide the following services to psychiatric patients: (a) Integrated emergency psychiatric services in the form of crisis hotlines, mobile crisis intervention teams, and inpatient wards. Some of the crisis hotlines that are currently operational in Iran are the Police (Dial 110), Medical Emergency (Dial 115), and Social Emergency (Dial 123). There is no need to provide more similar services, especially new crisis hotlines and mobile crisis intervention teams; (b) Short- and long-term hospitalization services. Considering a point prevalence of 22% for psychiatric disorders in Iran according to the results of the systematic review and meta-analysis, a minimum estimate of 3% for the annual prevalence of severe psychiatric disorders was considered as the criterion for calculating the number of beds and providing other future services. Based on the made calculations, there was a need for 12 beds for acute psychiatric diseases and 5 beds for short- and long-term hospitalization for a population of 100,000 in case of providing community mental health services; (c) Home visit services. The psychiatric patients can be classified into two groups according to their disease severity: a group requiring more follow-up care and a group with the need for less follow-up care. For the first group, home visit services are currently provided by the welfare organization and community-based mental health care centers. For the second group, family education services, psychosocial rehabilitation, and emergency services can be provided by dialing 110 or 115; (d) Daycare and rehabilitation services. For a population of 100,000, about 100 people would be eligible for receiving daycare services, which requires the establishment of 2-4 daycare centers so that each center can provide services to 30-50 people; (e) Vocational rehabilitation services: According to various studies, an unemployment rate of 70% seems reasonable for psychiatric patients. Based on the calculation results, for 750 patients with severe mental diseases, there would be a need for providing vocational rehabilitation service to 52 people, which can be met through supportive/productive workshops and training of business owners, industries, and non-governmental organizations; (f) Accommodation services. In Iran, according to the cultural situation and extended families, the number of homeless psychiatric patients is 1%. In other words, for 750 severe psychiatric patients per 100,000 population, there would be about 8-10 homeless patients. On the other hand, for a typical family of four in Iran, there would be a need for an 80-m2 apartment; i.e. per 100,000 population, they can be accommodated in two 80-m2 apartments each with a capacity of 4 people.
4. Discussion and Conclusion
This study aimed to provide an optimal model of comprehensive urban mental health services and rehabilitation for patients with severe psychiatric diseases, based on collaboration between family physicians and the organizations that provide health care services. Since the current health system allocates a very small amount of budget to psychiatric hospitals which provide services to acute psychiatric patients for hospitalization, a coherent system can be useful for optimal management of at least one-fifth of the mental health needs of the community. There is a need for coordination between the organizations providing these services to plan carefully, eliminate similar services, and prevent the waste of human capital and resources.
Ethical Considerations
Compliance with ethical guidelines
All included studies would be cited in all reports and in all future publications.
Funding
This project was supported by the Ministry of Health, the Office of Mental Health and Addiction, and the Vice-Chancellor for Research and Technology of Shahrekord University of Medical Sciences.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We want to thanks the Mental Health Office Social and addiction Ministry of Health and Medical Education, and the Vice-Chancellor for Research and Technology of Shahrekord University of Medical Sciences.
Refrences:
Studies on the integratation of mental health into primary health care in Iran have been conducted since 1986, which was later implemented successfully within the Rural Family Physician Program in 1988. In urban areas, there is no structured mental health care system and the private sector provides health care services mostly focused on the biomedical model of care. Due to demographic changes in Iran’s population, urban sprawl, and the changes in the urban/rural proportion, the need for a coherent plan to provide mental health services in urban areas is felt more than ever. This study aims to investigate the feasibility of establishing the urban mental health care system for patients with severe psychiatric diseases based on collaboration between organizations in Iran.
2. Materials and Methods
The study reviews the integrated plan for urban mental health services in Iran. First, a systematic review was conducted to get acquainted with the models of providing urban mental health services worldwide, including the World Health Organization (WHO)’s model in the field of mental health care. Then, the situational analysis of the services provided in Iran was carried out using the WHO Assessment Instrument for Mental Health Systems (WHO-AIMS). Legal duties of beneficiary organizations, and the Inter-sectoral collaboration of the Ministry of Health and beneficiary organizations were reviewed along with seeking for the opinions of international and national experts using the Delphi method. The model estimates the need for mental health services in cities with 100,000 population.
3. Results
The prevalence of mental diseases in Iran was similar to the global rate. The most prevalent mental disease was major depressive disorder followed by substance abuse. The number of male and female patients with mental diseases was not equal. The proposed model was mainly for severe mental diseases such as severe depression, bipolar mood disorder, and the spectrum of psychotic disorders that account for the highest number of admissions to psychiatric hospitals. According to the results of the literature review and based on the opinions of experts, the urban mental health care system should provide the following services to psychiatric patients: (a) Integrated emergency psychiatric services in the form of crisis hotlines, mobile crisis intervention teams, and inpatient wards. Some of the crisis hotlines that are currently operational in Iran are the Police (Dial 110), Medical Emergency (Dial 115), and Social Emergency (Dial 123). There is no need to provide more similar services, especially new crisis hotlines and mobile crisis intervention teams; (b) Short- and long-term hospitalization services. Considering a point prevalence of 22% for psychiatric disorders in Iran according to the results of the systematic review and meta-analysis, a minimum estimate of 3% for the annual prevalence of severe psychiatric disorders was considered as the criterion for calculating the number of beds and providing other future services. Based on the made calculations, there was a need for 12 beds for acute psychiatric diseases and 5 beds for short- and long-term hospitalization for a population of 100,000 in case of providing community mental health services; (c) Home visit services. The psychiatric patients can be classified into two groups according to their disease severity: a group requiring more follow-up care and a group with the need for less follow-up care. For the first group, home visit services are currently provided by the welfare organization and community-based mental health care centers. For the second group, family education services, psychosocial rehabilitation, and emergency services can be provided by dialing 110 or 115; (d) Daycare and rehabilitation services. For a population of 100,000, about 100 people would be eligible for receiving daycare services, which requires the establishment of 2-4 daycare centers so that each center can provide services to 30-50 people; (e) Vocational rehabilitation services: According to various studies, an unemployment rate of 70% seems reasonable for psychiatric patients. Based on the calculation results, for 750 patients with severe mental diseases, there would be a need for providing vocational rehabilitation service to 52 people, which can be met through supportive/productive workshops and training of business owners, industries, and non-governmental organizations; (f) Accommodation services. In Iran, according to the cultural situation and extended families, the number of homeless psychiatric patients is 1%. In other words, for 750 severe psychiatric patients per 100,000 population, there would be about 8-10 homeless patients. On the other hand, for a typical family of four in Iran, there would be a need for an 80-m2 apartment; i.e. per 100,000 population, they can be accommodated in two 80-m2 apartments each with a capacity of 4 people.
4. Discussion and Conclusion
This study aimed to provide an optimal model of comprehensive urban mental health services and rehabilitation for patients with severe psychiatric diseases, based on collaboration between family physicians and the organizations that provide health care services. Since the current health system allocates a very small amount of budget to psychiatric hospitals which provide services to acute psychiatric patients for hospitalization, a coherent system can be useful for optimal management of at least one-fifth of the mental health needs of the community. There is a need for coordination between the organizations providing these services to plan carefully, eliminate similar services, and prevent the waste of human capital and resources.
Ethical Considerations
Compliance with ethical guidelines
All included studies would be cited in all reports and in all future publications.
Funding
This project was supported by the Ministry of Health, the Office of Mental Health and Addiction, and the Vice-Chancellor for Research and Technology of Shahrekord University of Medical Sciences.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We want to thanks the Mental Health Office Social and addiction Ministry of Health and Medical Education, and the Vice-Chancellor for Research and Technology of Shahrekord University of Medical Sciences.
Refrences:
- Mehrdad R. Health system in Iran. Japan Medical Association Journal. 2009; 52(1):69-73. https://www.researchgate.net/profile/Ramin-Mehrdad/publication/232426386_Health_System_in_Iran/links/0c9605281d9d29d0bc000000/Health-System-in-Iran.pdf#page=71
- Naeli J, Mogimi D. Primary care health promotion policy document. Tehran: Ministry of Health; 2007.
- Bagyani-Mogadam H, Ehraampoosh M. Principles of health services. Tehran: Cherag-E Danesh; 2003.
- Park K. Park’s textbook of preventive and social medicine. Jabalpur, Madhya Pradesh: Bhanot Publishers; 2017. https://books.google.com/books?id=SymHtAEACAAJ&dq=Park%E2%80%99s+textbook+of+preventive+and+social+medicine&hl=en&sa=X&ved=2ahUKEwiyq7Ojp8nxAhWox4UKHYyOA3gQ6AEwAHoECAsQAQ
- Funk M. Integrating mental health into primary care: A global perspective [Internet]. 2008 [Updated 2008]. Available from: https://www.who.int/mental_health/policy/services/integratingmhintoprimarycare/en/
- Asadi-Lari M, Sayyari A, Akbari M, Gray D. Public health improvement in Iran-lessons from the last 20 years. Public Health. 2004; 118(6):395-402. [DOI:10.1016/j.puhe.2004.05.011] [PMID]
- Bagheri-Yazdi S, Malek-Afzali H, Shahmohammadi D, Naghavi-Ravandi M, Hekmat S. Evaluation of functions of auxiliary health workers (Behvarzes) and health volunteers in mental health care delivery in the framework of PHC system in Brojen city, Chaharmahal and Bakhtiary province. Hakim Research Journal. 2001; 4(2):100-9.
- Shahmohammadi D, Bayanzadeh S A, Ehssanmanesh M. [Pathways to psychiatric care in Iran (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology (IJPCP). 1998; 3(4):4-14. http://ijpcp.iums.ac.ir/article-1-1706-en.html
- Caracci G. Urban mental health: An international survey. International Journal of Mental Health. 2006; 35(1):39-45. [DOI:10.2753/IMH0020-7411350103]
- Sharifi V, Abolhasani F, Farhoudian A, Amin-Esmaeili M. Community Mental Health Centers in Iran: Planning evidence-based services. Iranian Journal of Psychiatry & Clinical Psychology. 2013; 19(3):163-76. https://web.a.ebscohost.com/abstract?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=
- Rashedi V, Malakouti K, Rudnik A. Community mental health service for older adults in Iran. Journal of Kermanshah University of Medical Sciences. 2018; 22(2):e78947. [DOI:10.5812/jkums.78947]
- WHO and AIMS. A report of the assessment of the mental health system in Uttarkhand, India, using the World Health Organization - Assessment Instrument for Mental Health Systems (WHO-AIMS). Geneva: WHO 2006. https://apps.who.int/iris/bitstream/handle/10665/206158/B0768.pdf?sequence=1
- Sharifi V. [Urban mental health in Iran: challenges and future directions (Persian)]. Iranian Journal of Psychiatry and Behavioral Sciences. 2009; 3(1):9-14. https://www.sid.ir/en/journal/ViewPaper.aspx?ID=143475
- Noorbala AA, Bagheri Yazdi SA, Asadi Lari M, Vaez Mahdavi MR. [Mental health status of individuals fifteen years and older in Tehran-Iran (2009) (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2011; 16(4):479-83. http://ijpcp.iums.ac.ir/article-1-1212-en.html
- Noorbala AA, Yazdi SB, Yasamy M, Mohammad K. Mental health survey of the adult population in Iran. The British Journal of Psychiatry. 2004; 184(1):70-3. [DOI:10.1192/bjp.184.1.70] [PMID]
- Ministry of Health and Medical Education. A national report on registration of case with psychiatric disorder in integration of mental health in primary care program. Tehran: Ministry of Health and Medical Education; 2008. [Linke not Found]
- Amini H, Sharifi V, Nejatisafa A, Arbabi M, Tabatabaie M, Alimadadi Z, et al. [One year follow-up of patients with bipolar disorder admitted to Roozbeh Hospital (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2009; 15(2):168-74. http://ijpcp.iums.ac.ir/browse.php?a_id=699&slc_lang=fa&sid=1&ftxt=1
- Bolhari J, Zojaji A, Karimi-Kisomi I, Nazari-Jeirani M, Tabaee S. [Urban mental health service: Primary health care model with community participation. Iranian Journal of Psychiatry and Clinical Psychology. 2011; 17(2):110-5. http://irisweb.ir/files/site1/rds_journals/21/article-21-85192.pdf
- Hajebi A, Damari B, Moghaddam AV, Nasehi A, Nikfarjam A, Bolhari J. What to do to promote mental health of the society. Iranian Journal of Public Health. 2013; 42(Supple1):105-12. [PMCID] [PMID]
- Khayatzadeh A, Takian A. Family physician program in Iran: Considerations for adapting the policy in urban settings. Archives of Iranian Medicine. 2014; 17(11):776-778. [PMID]
- World Heald Organization. Improving health systems and services for mental health [Internet]. 2009 [Updated 2009]. Available from: http://apps.who.int/iris/bitstream/handle/10665/44219/9789241598774_eng.pdf;jsessionid=A91BCF97C36BA33024CAF66A5A1881BE?sequence=1
- World Health Organization. Integrating mental health into primary care: A global perspective [Internet]. 2008 [Updated 2008]. Available from: https://www.who.int/mental_health/policy/services/integratingmhintoprimarycare/en/
- World Health Organization. Investing in mental health. Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/42823
- State Welfare Organization of Iran. Social emergency program (Persian) [Internet]. 2020 [Updated 2020 September 27]. Available from: https://www.behzisti.ir/news/23534/
- Ministry of Cooperatives, Labour, and Social Welfare. Social emergency program (Persian) [Internet]. 2021 [Updated 2021 July 04]. Available from: https://asibha.mcls.gov.ir/fa/ghorop/marriageanddirorce/manabeejtemaei/barname
- State Welfare Organization of Iran. Executive instructions of the Crisis Intervention Center (individual, family and social) "Social Emergency Center" (Persian) [Internet]. 2008 [Updated 2008]. Available from: http://hormozganbeh.ir/attachments/article/2311/
- Gould MS, Kalafat J, HarrisMunfakh JL, Kleinman M. An evaluation of crisis hotline outcomes part 2: Suicidal callers. Suicide and Life‐Threatening Behavior. 2007; 37(3):338-52. [DOI:10.1521/suli.2007.37.3.338] [PMID]
- Kalafat J, Gould MS, Munfakh JLH, Kleinman M. An evaluation of crisis hotline outcomes. Part 1: Nonsuicidal crisis callers. Suicide and Life-Threatening Behavior. 2007; 37(3):322-37. [DOI:10.1521/suli.2007.37.3.322] [PMID]
- Gilat I, Shahar G. Emotional first aid for a suicide crisis: comparison between Telephonic hotline and internet. Psychiatry: Interpersonal and Biological Processes. 2007; 70(1):12-8. [DOI:10.1521/psyc.2007.70.1.12] [PMID]
- Bennett L, Riger S, Schewe P, Howard A, Wasco S. Effectiveness of hotline, advocacy, counseling, and shelter services for victims of domestic violence: A statewide evaluation. Journal of Interpersonal Violence. 2004; 19(7):815-29. [DOI:10.1177/0886260504265687] [PMID]
- Johnson S, Nolan F, Pilling S, Sandor A, Hoult J, McKenzie N, et al. Randomised controlled trial of acute mental health care by a crisis resolution team: the north Islington crisis study. The BMJ. 2005; 331(7517):599. [DOI:10.1136/bmj.38519.678148.8F] [PMID] [PMCID]
- Irving CB, Adams CE, Rice K. Crisis intervention for people with severe mental illnesses. Cochrane Database of Systematic Reviews. 2006; 4. [DOI:10.1002/14651858.CD001087.pub3]
- Jacobs R, Barrenho E. Impact of crisis resolution and home treatment teams on psychiatric admissions in England. The British Journal of Psychiatry. 2011; 199(1):71-6. [DOI:10.1192/bjp.bp.110.079830] [PMID]
- Needle J, Bindman JP, Thornicroft G. Crisis resolution and home treatment in mental health. Johnson S, editor. Cambridge: Cambridge University Press; 2008. [DOI:10.1017/S003329170999170X]
- McGlynn P, editor. Crisis resolution and home treatment: A practical guide. London: Sainsbury Centre for Mental Health; 2006.
- Farhoudian A, Sharifi V, Amini H, Basirnia A, Mesgarpour B, Mansouri N, et al. Prevalence of psychiatric disorders in Iran: A systematic review. Iranian Journal of Psychiatry. 2007; 2(4):137-50. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=165135
- Malakouti SK, Nojomi M, Panaghi L, Chimeh N, Mottaghipour Y, Joghatai MT, et al. Case-management for patients with schizophrenia in Iran: a comparative study of the clinical outcomes of mental health workers and consumers’ family members as case managers. Community Mental Health Journal. 2009; 45(6):447-52 [DOI:10.1007/s10597-009-9197-4] [PMID]
- Mansouri N, Malakouti SK, Chimeh N, Rezvanifar S, Mohseni M, Mansouri E. Chronic hospitalized and household maintained consumers; characteristics and differences among referees to the Iranian society supporting individuals with Schizophrenia. Iranian Journal of Psychiatry and Behavioral Sciences. 2014; 8(1):5-12. [PMCID] [PMID]
- Mansouri N, Chimeh N, Dehghani M, Malakouti SK, Taherkhani H, Abarashi Z. Risk factors associated with psychiatric hospitalization among Iranian schizophrenic patients. Iranian Journal of Psychiatry and Behavioral Sciences. 2013; 7(2):16-23. [PMCID] [PMID]
- Malakouti SK, Mirabzadeh A, Nojomi M, Tonkaboni AA, Nadarkhani F, Mirzaie M, et al. Clinical outcomes and cost effectiveness of two aftercare models provided by general physicians and nurses to patients with severe mental illness. Medical Journal of the Islamic Republic of Iran. 2015; 29:196. [PMCID] [PMID]
- Khaleghparast S, Ghanbari B, Kahani S, Malakouti K, SeyedAlinaghi S, Sudhinaraset M. The effectiveness of discharge planning on the knowledge, clinical symptoms and hospitalisation frequency of persons with schizophrenia: a longitudinal study in two hospitals in Tehran, Iran. Journal of Clinical Nursing. 2014; 23(15-16):2215-22. [DOI:10.1111/jocn.12499] [PMID]
- Moradi‐Lakeh M, Yaghoubi M, Hajebi A, Malakouti SK, Vasfi MG. Cost‐effectiveness of aftercare services for people with severe mental disorders: An analysis parallel to a randomised controlled clinical trial in Iran. Health & Social Care in the Community. 2017; 25(3):1151-9 [DOI:10.1111/hsc.12416] [PMID]
- Sharifi V, Amini H, Tehrani DM, Yasami M, Jalali RM, Sobh BP, et al. Roozbeh home care program for severe mental disorders: A preliminary report. Iranian Journal of Psychiatry. 2006; 1(1):31-4. https://ijps.tums.ac.ir/index.php/ijps/article/view/400/395
- Glick ID, Fleming L, DeChillo N, Meyerkopf N, Jackson C, Muscara D, et al. A controlled study of transitional day care for non-chronically-ill patients. The American Journal of Psychiatry. 1986; 143(12):1551-6. [DOI:10.1176/ajp.143.12.1551] [PMID]
- Linn MW, Caffey EM, Klett CJ, Hogarty GE, Lamb HR. Day treatment and psychotropic drugs in the aftercare of schizophrenic patients: A veterans administration cooperative study. Occupational Therapy in Mental Health. 1980; 1(1):77-106. [DOI:10.1300/J004v01n01_06]
- Wiersma D, Kluiter H, Nienhuis FJ, Rüphan M, Giel R. Costs and benefits of day treatment with community care for schizophrenic patients. Schizophrenia Bulletin. 1991; 17(3):411-9. [DOI:10.1093/schbul/17.3.411] [PMID]
- Creed F, Black D, Anthony P, Osborn M, Thomas P, Tomenson B. Randomised controlled trial of day patient versus inpatient psychiatric treatment. The BMJ. 1990; 300(6731):1033-7. [DOI:10.1136/bmj.300.6731.1033] [PMID] [PMCID]
- Štrkalj-Ivezić S, Vrdoljak M, Mužinić L, Agius M. The impact of a rehabilitation day centre program for persons suffering from schizophrenia on quality of life, social functioning and self-esteem. Psychiatria Danubina. 2013; 25(2):194-9. http://www.psychiatria-danubina.com/UserDocsImages/pdf/dnb_vol25%20Suppl%202_no/dnb_vol25_noSuppl%202_194.pdf
- Marshall M, Crowther R, Almaraz-Serrano A, Creed F, Sledge W, Kluiter H, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health technology assessment (Winchester, England). 2001; 5(21):1-75. [DOI:10.3310/hta5210] [PMID]
- Lloyd C. Vocational rehabilitation and mental health. Hoboken: John Wiley & Sons; 2010. [DOI:10.1002/9781444319736]
- Williams A, Fossey E, Harvey C. Sustaining employment in a social firm: use of the Work Environment Impact Scale v 2.0 to explore views of employees with psychiatric disabilities. British Journal of Occupational Therapy. 2010; 73(11):531-9. [DOI:10.4276/030802210X12892992239279]
- Warner R. The diffusion of two successful rehabilitation models. World Psychiatry. 2006; 5(3):160-1. [PMCID] [PMID]
- Kubiak S, Roddy J, Comartin E, Tillander E. Cost analysis of long-term outcomes of an urban mental health court. Evaluation and Program Planning. 2015; 52:96-106 [DOI:10.1016/j.evalprogplan.2015.04.002] [PMID]
- Wells R, Kite B, Breckenridge E, Sunbury T. Community mental health center integrated care outcomes. Psychiatric Quarterly. 2018; 89(4):969-82. [DOI:10.1007/s11126-018-9594-3] [PMID]
- McKay C, Johnsen M, Stein R. Employment outcomes in Massachusetts clubhouses. Psychiatric Rehabilitation Journal. 2005; 29(1):25-33. [DOI:10.2975/29.2005.25.33] [PMID]
- Auerbach ES. The individual placement and support model vs. the menu approach to supported employment: Where does Occupational Therapy fit in? Occupational Therapy in Mental Health. 2002; 17(2):1-19. [DOI:10.1300/J004v17n02_01]
- Moll S, Huff J, Detwiler L. Supported employment: Evidence for a best practice model in psychosocial rehabilitation. Canadian Journal of Occupational Therapy. 2003; 70(5):298-310. [DOI:10.1177/000841740307000506] [PMID]
- Crowther RE, Marshall M, Bond GR, Huxley P. Helping people with severe mental illness to obtain work: Systematic review. The BMJ. 2001; 322(7280):204-8. [DOI:10.1136/bmj.322.7280.204] [PMID] [PMCID]
- Lehman AF, Goldberg R, Dixon LB, McNary S, Postrado L, Hackman A, et al. Improving employment outcomes for persons with severe mental illnesses. Archives of General Psychiatry. 2002; 59(2):165-72. [DOI:10.1001/archpsyc.59.2.165] [PMID]
- Corrigan PW, Mueser KT, Bond GR, Drake RE, Solomon P. Principles and practice of psychiatric rehabilitation: An empirical approach. New York: Guilford Press; 2012.
- Rogers ES, Anthony W, Kash M, Olschewski A. Systematic review of supported housing literature 1993-2008. Center for Psychiatric Rehabilitation. Boston: Boston University; 2010.
- Tsemberis S. Housing first: The pathways model to end homelessness for people with mental illness and addiction manual. European Journal of Homelessness. 2011; 5(2):235-40. https://www.researchgate.net/publication/47669330_
- Chilvers R, Macdonald G, Hayes A. Supported housing for people with severe mental disorders. Cochrane Database of Systematic Reviews. 2006; (4):CD000453 [DOI:10.1002/14651858.CD000453.pub2] [PMID] [PMCID]
- Malakouti SK, Noori R, Naghavi M, Ahmad Abhari A, Nasr M, & Afagh S, Salehi P, et al. [The burden of caregivers of chronic mental patients and their needs to care and therapeutic services (Persian)]. Hakim. 2003; 6(2):1-10. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=62559
- Damari B, Alikhani S, Riazi-Isfahani S, Hajebi A. Transition of mental health to a more responsible service in Iran. Iranian Journal of Psychiatry. 2017; 12(1):36-41. [PMCID] [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2019/11/23 | Accepted: 2020/06/20 | Published: 2021/04/20
Received: 2019/11/23 | Accepted: 2020/06/20 | Published: 2021/04/20
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



