Tue, Jul 1, 2025
| فارسی
Volume 23, Issue 2 (Summer 2017)
IJPCP 2017, 23(2): 136-147 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pirnia B, Rasoulzadeh Tabatabaei S K, Pirkhaefi A, Soleimani A. Comparison of the Effectiveness of Two Cognitive-Behavioral and Mother-Child Interactive Therapies on Anxiety of Children With Under-Methadone Treatment Mother. IJPCP 2017; 23 (2) :136-147
URL: http://ijpcp.iums.ac.ir/article-1-2466-en.html
URL: http://ijpcp.iums.ac.ir/article-1-2466-en.html
1- Department of Psychology, Faculty of Humanities, University of Science and Culture , E-mail: b.pirnia@usc.ac.ir
2- 1.Department of Psychology, School of Humanities, Tarbiat Modares University2.Department of Psychology, Faculty of Education and Psychology, Ferdowsi University of Mashhad
3- Department of Psychology, Faculty of Psychology and Medical science, Garmsar Branch, Islamic Azad University
4- Department of Psychology, Faculty of Humanities, University of Science and Culture
2- 1.Department of Psychology, School of Humanities, Tarbiat Modares University2.Department of Psychology, Faculty of Education and Psychology, Ferdowsi University of Mashhad
3- Department of Psychology, Faculty of Psychology and Medical science, Garmsar Branch, Islamic Azad University
4- Department of Psychology, Faculty of Humanities, University of Science and Culture
Keywords: Cognitive-Behavioral Therapy (CBT), Parent-Child Interaction Therapy (PCIT), Methadone Maintenance Treatment (MMT)
Full-Text [PDF 2384 kb]
(4160 Downloads)
| Abstract (HTML) (9352 Views)
Full-Text: (5955 Views)
Extended Abstract
1. Introduction
In recent years, experts as well as parents are paying more attention to childhood disorders. Over time, early childhood impairment is accompanied with more resistant courses towards treatment and weaker treatment results [1, 2]. Anxiety disorders are the most common psychiatric disorders in childhood due to the fact that common infrastructure mechanisms has a high degree of coordination with other mental disorders and are usually accompanied by inclusive problems in life [3, 4]. Since the effectiveness of drug therapy for anxiety disorders is not clear [35], the current therapeutic approaches in the field of addiction treatment are not clinically tested, and many parents avoid drug therapy because of its side effects, we intended to compare two cognitive-behavioral (child friendly) and parent-child interactive therapies.
2. Method
This study has a semi-experimental design with pre-test, post-test and six months follow-up. It was conducted among families with under-methadone-treatment mothers who were referred to two methadone treatment clinics in Tehran. A total of 75 mothers and children (N=75) were purposefully chosen and randomly assigned to the following three groups (n=25): Child Cognitive-Behavioral Therapy, Interactive mother-child treatment, and the control group. Protocol of the treatments mentioned was presented in eight sessions a week for two treatment groups, and the control group was on the waiting list. Child anxiety levels in three stages of pre-test, post-test and follow-up were evaluated using Spencer Anxiety Scale (response rate=94%), and the resulting data were analyzed using SPSS19 software and with the help of Chi Square, Independent t and Analysis of Variance with repeated measurements.
3. Results
Demographic characteristics of participants
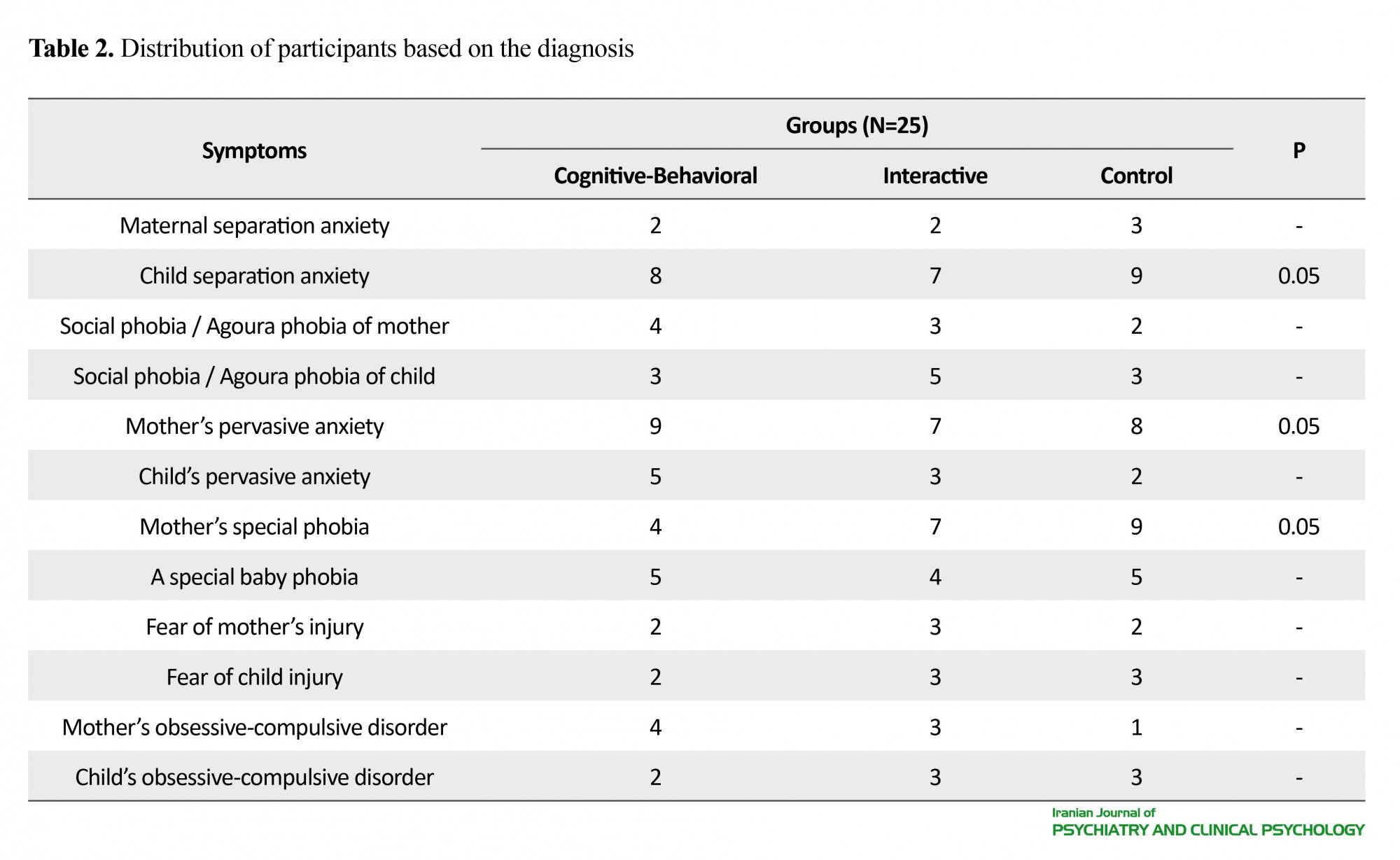
Table 1 shows demographic characteristics of 75 participants of the research. Statistical analysis by Chi-square test suggests that subject distribution in age and monthly income indices show significant differences (P<0.05). In the table, the diagnoses taken based on DSM-IV criteria are provided. As can be seen, there is a significant difference between the diagnoses taken of mothers and children in three disorders of separation anxiety, inclusive anxiety, and certain phobia (P<0.05). There is no significant difference between the three research groups in terms of diagnostic distribution (P<0.05) (Table 2). In order to evaluate the difference in scores of subjects before the intervention, these scores were evaluated in the pre-test stage by independent t-test. The results showed that there is no significant difference between research groups on anxiety index (P<0.05). Comparison of pre-test and the post-test scores shows that differences in anxiety scores in two treatment groups in the post-test stage are significant. Mean and standard deviation of anxiety scores in behavioral-cognitive group in the pre-test stage was 94.72±3.24 compared to 89.71±2.14 in the post-test stage. In the interactive group, these scores in the pre-test stage were 95.21±2.97 compared to 91.09±3.81 in the post-test stage. According to the above findings, the effectiveness of cognitive-behavioral and interactive therapies on the anxiety variable in the post-test stage is significant (P<0.01). Also, the comparison between the effectiveness of two cognitive-behavioral and interactive therapies showed that there was not a significant difference between the two treatments in anxiety reduction (P>0.65).
The results of ANOVA test with repeated measures showed that the difference in the scores in the follow-up stage is not significant. Therefore, the effectiveness of both cognitive-behavioral and interactive therapies on anxiety index is significant only in the post-test stage, compared to the control group (P<0.001).
4. Discussion
This study has been conducted with the aim to compare the effectiveness of two cognitive behavioral and interactive parent-child therapeutic approaches on anxiety index in 5-7-year-old Tehrani children with Methadone-consuming mothers. The results of the study showed that both therapeutic approaches had a significant effect in reducing the symptoms of anxiety, compared to control group. Neil and Christine [16] examined 27 studies carried out in 2009 in the framework of a systematic study with the aim of evaluating the effectiveness of cognitive-behavioral therapy in the form of preventive and early interventions conducted about mental health problems in children and reported the effectiveness of this treatment on anxiety syndrome as desirable. Also, Urao et al. [18] showed the effectiveness of cognitive-behavioral therapy based on Anxiety Prevention Program in a sample of Japanese children. Puliafico et al. [42] used an interactive approach to treat anxiety disorders in children, and the results suggested the effectiveness of the treatment. Of course, there are results regarding the effectiveness of this treatment in treating depression disorder. For example, Luby et al. [31]used an interactive approach in the treatment of depression in a sample of 54 children aged 3-6 years who lacked metacognitive abilities to use cognitive-behavioral therapy, which had been reported as successful. Also, Lenze et al. [32] used interactive therapy successfully with the goal of reducing the symptoms of depression in preschoolers. Kortlander et al. [45] compared mothers of anxious children with control group mothers based on their expectations of their child in responding to anxiety situations. Mothers of anxious children showed higher expectations, lower compatibility skills, and less self-confidence in management of their homework. In this regard, Shamir et al. [46] reported that anxiety syndrome in a sample of 104 preschoolers that were selected based on the high and low index of behavioral inhibition is related to trait anxiety of the mother and insecure attachment style. The results of this study showed that both cognitive-behavioral and interactive therapy had a significant effect on child anxiety index. However, there was no significant difference between the effectiveness of these two treatments. The findings can be valuable in the field of prevention and treatment of anxiety disorders.
Acknowledgments
Bijan Drug Abuse Treatment Center has financially supported the present paper.
Conflict of Interest
The authors declared no conflicts of interest.
1. Introduction
In recent years, experts as well as parents are paying more attention to childhood disorders. Over time, early childhood impairment is accompanied with more resistant courses towards treatment and weaker treatment results [1, 2]. Anxiety disorders are the most common psychiatric disorders in childhood due to the fact that common infrastructure mechanisms has a high degree of coordination with other mental disorders and are usually accompanied by inclusive problems in life [3, 4]. Since the effectiveness of drug therapy for anxiety disorders is not clear [35], the current therapeutic approaches in the field of addiction treatment are not clinically tested, and many parents avoid drug therapy because of its side effects, we intended to compare two cognitive-behavioral (child friendly) and parent-child interactive therapies.
2. Method
This study has a semi-experimental design with pre-test, post-test and six months follow-up. It was conducted among families with under-methadone-treatment mothers who were referred to two methadone treatment clinics in Tehran. A total of 75 mothers and children (N=75) were purposefully chosen and randomly assigned to the following three groups (n=25): Child Cognitive-Behavioral Therapy, Interactive mother-child treatment, and the control group. Protocol of the treatments mentioned was presented in eight sessions a week for two treatment groups, and the control group was on the waiting list. Child anxiety levels in three stages of pre-test, post-test and follow-up were evaluated using Spencer Anxiety Scale (response rate=94%), and the resulting data were analyzed using SPSS19 software and with the help of Chi Square, Independent t and Analysis of Variance with repeated measurements.
3. Results
Demographic characteristics of participants
Table 1 shows demographic characteristics of 75 participants of the research. Statistical analysis by Chi-square test suggests that subject distribution in age and monthly income indices show significant differences (P<0.05). In the table, the diagnoses taken based on DSM-IV criteria are provided. As can be seen, there is a significant difference between the diagnoses taken of mothers and children in three disorders of separation anxiety, inclusive anxiety, and certain phobia (P<0.05). There is no significant difference between the three research groups in terms of diagnostic distribution (P<0.05) (Table 2). In order to evaluate the difference in scores of subjects before the intervention, these scores were evaluated in the pre-test stage by independent t-test. The results showed that there is no significant difference between research groups on anxiety index (P<0.05). Comparison of pre-test and the post-test scores shows that differences in anxiety scores in two treatment groups in the post-test stage are significant. Mean and standard deviation of anxiety scores in behavioral-cognitive group in the pre-test stage was 94.72±3.24 compared to 89.71±2.14 in the post-test stage. In the interactive group, these scores in the pre-test stage were 95.21±2.97 compared to 91.09±3.81 in the post-test stage. According to the above findings, the effectiveness of cognitive-behavioral and interactive therapies on the anxiety variable in the post-test stage is significant (P<0.01). Also, the comparison between the effectiveness of two cognitive-behavioral and interactive therapies showed that there was not a significant difference between the two treatments in anxiety reduction (P>0.65).
The results of ANOVA test with repeated measures showed that the difference in the scores in the follow-up stage is not significant. Therefore, the effectiveness of both cognitive-behavioral and interactive therapies on anxiety index is significant only in the post-test stage, compared to the control group (P<0.001).
4. Discussion
This study has been conducted with the aim to compare the effectiveness of two cognitive behavioral and interactive parent-child therapeutic approaches on anxiety index in 5-7-year-old Tehrani children with Methadone-consuming mothers. The results of the study showed that both therapeutic approaches had a significant effect in reducing the symptoms of anxiety, compared to control group. Neil and Christine [16] examined 27 studies carried out in 2009 in the framework of a systematic study with the aim of evaluating the effectiveness of cognitive-behavioral therapy in the form of preventive and early interventions conducted about mental health problems in children and reported the effectiveness of this treatment on anxiety syndrome as desirable. Also, Urao et al. [18] showed the effectiveness of cognitive-behavioral therapy based on Anxiety Prevention Program in a sample of Japanese children. Puliafico et al. [42] used an interactive approach to treat anxiety disorders in children, and the results suggested the effectiveness of the treatment. Of course, there are results regarding the effectiveness of this treatment in treating depression disorder. For example, Luby et al. [31]used an interactive approach in the treatment of depression in a sample of 54 children aged 3-6 years who lacked metacognitive abilities to use cognitive-behavioral therapy, which had been reported as successful. Also, Lenze et al. [32] used interactive therapy successfully with the goal of reducing the symptoms of depression in preschoolers. Kortlander et al. [45] compared mothers of anxious children with control group mothers based on their expectations of their child in responding to anxiety situations. Mothers of anxious children showed higher expectations, lower compatibility skills, and less self-confidence in management of their homework. In this regard, Shamir et al. [46] reported that anxiety syndrome in a sample of 104 preschoolers that were selected based on the high and low index of behavioral inhibition is related to trait anxiety of the mother and insecure attachment style. The results of this study showed that both cognitive-behavioral and interactive therapy had a significant effect on child anxiety index. However, there was no significant difference between the effectiveness of these two treatments. The findings can be valuable in the field of prevention and treatment of anxiety disorders.
Acknowledgments
Bijan Drug Abuse Treatment Center has financially supported the present paper.
Conflict of Interest
The authors declared no conflicts of interest.
References
- Ramsawh HJ, Weisberg RB, Dyck I, Stout R, Keller MB. Age of onset, clinical characteristics, and 15-year course of anxiety disorders in a prospective, longitudinal, observational study. Journal of Affective Disorders. 2011; 132(1-2):260–4. doi: 10.1016/j.jad.2011.01.006
- Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression. Archives of General Psychiatry. 2009; 66(8):897. doi: 10.1001/archgenpsychiatry.2009.97
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009; 32(3):483–524. doi: 10.1016/j.psc.2009.06.002
- Rapee RM, Schniering CA, Hudson JL. Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology. 2009; 5(1):311–41. doi: 10.1146/annurev.clinpsy.032408.153628
- Wichstrøm L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E, Sveen TH. Prevalence of psychiatric disorders in preschoolers. Journal of Child Psychology and Psychiatry. 2011; 53(6):695–705. doi: 10.1111/j.1469-7610.2011.02514.x
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012; 21(3):169–84. doi: 10.1002/mpr.1359
- Dougherty LR, Tolep MR, Bufferd SJ, Olino TM, Dyson M, Traditi J, et al. Preschool anxiety disorders: Comprehensive assessment of clinical, demographic, temperamental, familial, and life stress correlates. Journal of Clinical Child & Adolescent Psychology. 2013; 42(5):577–89. doi: 10.1080/15374416.2012.759225
- Birmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, et al. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children – A preliminary psychometric study. Journal of Psychiatric Research. 2009; 43(7):680–6. doi: 10.1016/j.jpsychires.2008.10.003
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child & Adolescent Psychology. 2009; 38(3):315–28. doi: 10.1080/15374410902851382
- Lavigne JV, Gibbons RD, Christoffel KK, Arend R, Rosenbaum D, Binns H, et al. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child & Adolescent Psychiatry. 1996; 35(2):204–14. doi: 10.1097/00004583-199602000-00014
- Hopkins J, Lavigne JV, Gouze KR, LeBailly SA, Bryant FB. Multi-domain models of risk factors for depression and anxiety symptoms in preschoolers: Evidence for common and specific factors. Journal of Abnormal Child Psychology. 2013; 41(5):705–22. doi: 10.1007/s10802-013-9723-2
- Katz SJ, Conway CC, Hammen CL, Brennan PA, Najman JM. Childhood social withdrawal, interpersonal impairment, and young adult depression: A mediational model. Journal of Abnormal Child Psychology. 2011; 39(8):1227–38. doi: 10.1007/s10802-011-9537-z
- Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology. 1996; 64(2):333–42. doi: 10.1037/0022-006x.64.2.333
- Barrett PM. Evaluation of cognitive-behavioral group treatments for childhood anxiety disorders. Journal of Clinical Child Psychology. 1998; 27(4):459–68. doi: 10.1207/s15374424jccp2704_10
- Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. British Journal of Clinical Psychology. 2001; 40(4):399–410. doi: 10.1348/014466501163887
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clinical Psychology Review. 2009; 29(3):208–15. doi: 10.1016/j.cpr.2009.01.002
- Teubert D, Pinquart M. A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. Journal of Anxiety Disorders. 2011; 25(8):1046–59. doi: 10.1016/j.janxdis.2011.07.001
- Urao Y, Yoshinaga N, Asano K, Ishikawa R, Tano A, Sato Y, et al. Effectiveness of a cognitive behavioural therapy-based anxiety prevention programme for children: a preliminary quasi-experimental study in Japan. Child and Adolescent Psychiatry and Mental Health. 2016; 10:4. doi: 10.1186/s13034-016-0091-x
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999; 106(3):458–90. doi: 10.1037/0033-295x.106.3.458
- Wood JJ, McLeod BD, Sigman M, Hwang W-C, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry. 2003; 44(1):134–51. doi: 10.1111/1469-7610.00106
- McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007; 27(2):155–72. doi: 10.1016/j.cpr.2006.09.002
- Van der Bruggen CO, Stams GJJM, Bögels SM. Research Review: The relation between child and parent anxiety and parental control: A meta-analytic review. Journal of Child Psychology and Psychiatry. 2008; 49(12):1257–69. doi: 10.1111/j.1469-7610.2008.01898.x
- Stallard P. A clinician's guide to think good-feel good: Using CBT with children and young people. New Jersey: John Wiley & Sons; 2005.
- Abrahamse ME, Junger M, Chavannes EL, Coelman FJG, Boer F, Lindauer RJL. Parent–child interaction therapy for preschool children with disruptive behaviour problems in the Netherlands. Child and Adolescent Psychiatry and Mental Health. 2012; 6(1):24. doi: 10.1186/1753-2000-6-24
- Hood KK, Eyberg SM. Outcomes of parent-child interaction therapy: Mothers' reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003; 32(3):419-29. doi: 10.1207/s15374424jccp3203_10
- Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology. 2003; 71(2):251–60. doi: 10.1037/0022-006x.71.2.251
- Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent–child interaction therapy: One- and two-year follow-up of standard and abbreviated treatments for oppositional preschoolers. Journal of Abnormal Child Psychology. 2004; 32(3):263–71. doi: 10.1023/b:jacp.0000026140.60558.05
- Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J. Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology. 1998; 27(1):34–45. doi: 10.1207/s15374424jccp2701_4
- Pincus DB, Eyberg SM, Choate ML. Adapting parent-child interaction therapy for young children with separation anxiety disorder. Education and Treatment of Children. 2005; 28(2):163-81.
- Choate ML, Pincus DB, Eyberg SM, Barlow DH. Parent-child interaction therapy for treatment of separation anxiety disorder in young children: A pilot study. Cognitive and Behavioral Practice. 2005; 12(1):126–35. doi: 10.1016/s1077-7229(05)80047-1
- Luby J, Lenze S, Tillman R. A novel early intervention for preschool depression: Findings from a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry. 2011; 53(3):313–22. doi: 10.1111/j.1469-7610.2011.02483.x
- Lenze SN, Pautsch J, Luby J. Parent-child interaction therapy emotion development: A novel treatment for depression in preschool children. Depression and Anxiety. 2010; 28(2):153–9. doi: 10.1002/da.20770
- Barnard M, McKeganey N. The impact of parental problem drug use on children: What is the problem and what can be done to help. Addiction. 2004; 99(5):552–9. doi: 10.1111/j.1360-0443.2003.00664.x
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict. Journal of Child Psychology and Psychiatry. 2007; 48(12):1174–83. doi: 10.1111/j.1469-7610.2007.01812.x
- Wagner KD. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder two randomized controlled trials. JAMA. 2003; 290(8):1033. doi: 10.1001/jama.290.8.1033
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. New York: New York State Psychiatric Institute; 2002.
- Sharifi V, Assadi SM, Mohammadi MR, Amini H, Kaviani H, Semnani Y, et al. [A Persian translation of the structured clinical interview for diagnostic and statistical manual of mental disorders (Persian)]. Comprehensive Psychiatry. 2009; 50(1):86–91. doi: 10.1016/j.comppsych.2008.04.004
- Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children’s anxiety: Psychometric properties and comparison with child-report in a clinic and normal sample. Behaviour Research and Therapy. 2004; 42(7):813–39. doi: 10.1016/s0005-7967(03)00200-6
- Ishikawa S, Sato H, Sasagawa S. Anxiety disorder symptoms in Japanese children and adolescents. Journal of Anxiety Disorders. 2009; 23(1):104–11. doi: 10.1016/j.janxdis.2008.04.003
- Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston: Cengage learning; 2002.
- Smith KE, Hudson JL. Metacognitive beliefs and processes in clinical anxiety in children. Journal of Clinical Child & Adolescent Psychology. 2013; 42(5):590–602. doi: 10.1080/15374416.2012.755925
- Puliafico AC, Comer JS, Pincus DB. Adapting parent-child interaction therapy to treat anxiety disorders in young children. Child and Adolescent Psychiatric Clinics of North America. 2012; 21(3):607–19. doi: 10.1016/j.chc.2012.05.005
- Spence SH, Shortt AL. Research review: Can we justify the widespread dissemination of universal, school-based interventions for the prevention of depression among children and adolescents. Journal of Child Psychology and Psychiatry. 2007; 48(6):526–42. doi: 10.1111/j.1469-7610.2007.01738.x
- Stallard P, Sayal K, Phillips R, Taylor JA, Spears M, Anderson R, et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: Pragmatic cluster randomised controlled trial. BMJ. 2012; 345:6058. doi: 10.1136/bmj.e6058
- Kortlander E, Kendall PC, Panichelli-Mindel SM. Maternal expectations and attributions about coping in anxious children. Journal of Anxiety Disorders. 1997; 11(3):297–315. doi: 10.1016/s0887-6185(97)00012-1
- Shamir-Essakow G, Ungerer JA, Rapee RM. Attachment, behavioral inhibition, and anxiety in preschool children. Journal of Abnormal Child Psychology. 2005; 33(2):131–43. doi: 10.1007/s10802-005-1822-2
- Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clinical Psychology Review. 2006; 26(7):834–56. doi: 10.1016/j.cpr.2005.08.001
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2016/02/26 | Accepted: 2016/12/3 | Published: 2017/07/1
Received: 2016/02/26 | Accepted: 2016/12/3 | Published: 2017/07/1
References
1. Ramsawh HJ, Weisberg RB, Dyck I, Stout R, Keller MB. Age of onset, clinical characteristics, and 15-year course of anxiety disorders in a prospective, longitudinal, observational study. Journal of Affective Disorders. 2011; 132(1-2):260–4. doi: 10.1016/j.jad.2011.01.006 [DOI:10.1016/j.jad.2011.01.006]
2. Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression. Archives of General Psychiatry. 2009; 66(8):897. doi: 10.1001/archgenpsychiatry.2009.97 [DOI:10.1001/archgenpsychiatry.2009.97]
3. Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009; 32(3):483–524. doi: 10.1016/j.psc.2009.06.002 [DOI:10.1016/j.psc.2009.06.002]
4. Rapee RM, Schniering CA, Hudson JL. Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology. 2009; 5(1):311–41. doi: 10.1146/annurev.clinpsy.032408.153628 [DOI:10.1146/annurev.clinpsy.032408.153628]
5. Wichstrøm L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E, Sveen TH. Prevalence of psychiatric disorders in preschoolers. Journal of Child Psychology and Psychiatry. 2011; 53(6):695–705. doi: 10.1111/j.1469-7610.2011.02514.x [DOI:10.1111/j.1469-7610.2011.02514.x]
6. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012; 21(3):169–84. doi: 10.1002/mpr.1359 [DOI:10.1002/mpr.1359]
7. Dougherty LR, Tolep MR, Bufferd SJ, Olino TM, Dyson M, Traditi J, et al. Preschool anxiety disorders: Comprehensive assessment of clinical, demographic, temperamental, familial, and life stress correlates. Journal of Clinical Child & Adolescent Psychology. 2013; 42(5):577–89. doi: 10.1080/15374416.2012.759225 [DOI:10.1080/15374416.2012.759225]
8. Birmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, et al. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children – A preliminary psychometric study. Journal of Psychiatric Research. 2009; 43(7):680–6. doi: 10.1016/j.jpsychires.2008.10.003 [DOI:10.1016/j.jpsychires.2008.10.003]
9. Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child & Adolescent Psychology. 2009; 38(3):315–28. doi: 10.1080/15374410902851382 [DOI:10.1080/15374410902851382]
10. Lavigne JV, Gibbons RD, Christoffel KK, Arend R, Rosenbaum D, Binns H, et al. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child & Adolescent Psychiatry. 1996; 35(2):204–14. doi: 10.1097/00004583-199602000-00014 [DOI:10.1097/00004583-199602000-00014]
11. Hopkins J, Lavigne JV, Gouze KR, LeBailly SA, Bryant FB. Multi-domain models of risk factors for depression and anxiety symptoms in preschoolers: Evidence for common and specific factors. Journal of Abnormal Child Psychology. 2013; 41(5):705–22. doi: 10.1007/s10802-013-9723-2 [DOI:10.1007/s10802-013-9723-2]
12. Katz SJ, Conway CC, Hammen CL, Brennan PA, Najman JM. Childhood social withdrawal, interpersonal impairment, and young adult depression: A mediational model. Journal of Abnormal Child Psychology. 2011; 39(8):1227–38. doi: 10.1007/s10802-011-9537-z [DOI:10.1007/s10802-011-9537-z]
13. Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology. 1996; 64(2):333–42. doi: 10.1037/0022-006x.64.2.333 [DOI:10.1037/0022-006X.64.2.333]
14. Barrett PM. Evaluation of cognitive-behavioral group treatments for childhood anxiety disorders. Journal of Clinical Child Psychology. 1998; 27(4):459–68. doi: 10.1207/s15374424jccp2704_10 [DOI:10.1207/s15374424jccp2704_10]
15. Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. British Journal of Clinical Psychology. 2001; 40(4):399–410. doi: 10.1348/014466501163887 [DOI:10.1348/014466501163887]
16. Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clinical Psychology Review. 2009; 29(3):208–15. doi: 10.1016/j.cpr.2009.01.002 [DOI:10.1016/j.cpr.2009.01.002]
17. Teubert D, Pinquart M. A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. Journal of Anxiety Disorders. 2011; 25(8):1046–59. doi: 10.1016/j.janxdis.2011.07.001 [DOI:10.1016/j.janxdis.2011.07.001]
18. Urao Y, Yoshinaga N, Asano K, Ishikawa R, Tano A, Sato Y, et al. Effectiveness of a cognitive behavioural therapy-based anxiety prevention programme for children: a preliminary quasi-experimental study in Japan. Child and Adolescent Psychiatry and Mental Health. 2016; 10:4. doi: 10.1186/s13034-016-0091-x [DOI:10.1186/s13034-016-0091-x]
19. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999; 106(3):458–90. doi: 10.1037/0033-295x.106.3.458 [DOI:10.1037/0033-295X.106.3.458]
20. Wood JJ, McLeod BD, Sigman M, Hwang W-C, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry. 2003; 44(1):134–51. doi: 10.1111/1469-7610.00106 [DOI:10.1111/1469-7610.00106]
21. McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007; 27(2):155–72. doi: 10.1016/j.cpr.2006.09.002 [DOI:10.1016/j.cpr.2006.09.002]
22. Van der Bruggen CO, Stams GJJM, Bögels SM. Research Review: The relation between child and parent anxiety and parental control: A meta-analytic review. Journal of Child Psychology and Psychiatry. 2008; 49(12):1257–69. doi: 10.1111/j.1469-7610.2008.01898.x [DOI:10.1111/j.1469-7610.2008.01898.x]
23. Stallard P. A clinician's guide to think good-feel good: Using CBT with children and young people. New Jersey: John Wiley & Sons; 2005.
24. Abrahamse ME, Junger M, Chavannes EL, Coelman FJG, Boer F, Lindauer RJL. Parent–child interaction therapy for preschool children with disruptive behaviour problems in the Netherlands. Child and Adolescent Psychiatry and Mental Health. 2012; 6(1):24. doi: 10.1186/1753-2000-6-24 [DOI:10.1186/1753-2000-6-24]
25. Hood KK, Eyberg SM. Outcomes of parent-child interaction therapy: Mothers' reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003; 32(3):419-29. doi: 10.1207/s15374424jccp3203_10 [DOI:10.1207/S15374424JCCP3203_10]
26. Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology. 2003; 71(2):251–60. doi: 10.1037/0022-006x.71.2.251 [DOI:10.1037/0022-006X.71.2.251]
27. Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent–child interaction therapy: One- and two-year follow-up of standard and abbreviated treatments for oppositional preschoolers. Journal of Abnormal Child Psychology. 2004; 32(3):263–71. doi: 10.1023/b:jacp.0000026140.60558.05 [DOI:10.1023/B:JACP.0000026140.60558.05]
28. Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J. Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology. 1998; 27(1):34–45. doi: 10.1207/s15374424jccp2701_4 [DOI:10.1207/s15374424jccp2701_4]
29. Pincus DB, Eyberg SM, Choate ML. Adapting parent-child interaction therapy for young children with separation anxiety disorder. Education and Treatment of Children. 2005; 28(2):163-81.
30. Choate ML, Pincus DB, Eyberg SM, Barlow DH. Parent-child interaction therapy for treatment of separation anxiety disorder in young children: A pilot study. Cognitive and Behavioral Practice. 2005; 12(1):126–35. doi: 10.1016/s1077-7229(05)80047-1 [DOI:10.1016/S1077-7229(05)80047-1]
31. Luby J, Lenze S, Tillman R. A novel early intervention for preschool depression: Findings from a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry. 2011; 53(3):313–22. doi: 10.1111/j.1469-7610.2011.02483.x [DOI:10.1111/j.1469-7610.2011.02483.x]
32. Lenze SN, Pautsch J, Luby J. Parent-child interaction therapy emotion development: A novel treatment for depression in preschool children. Depression and Anxiety. 2010; 28(2):153–9. doi: 10.1002/da.20770 [DOI:10.1002/da.20770]
33. Barnard M, McKeganey N. The impact of parental problem drug use on children: What is the problem and what can be done to help. Addiction. 2004; 99(5):552–9. doi: 10.1111/j.1360-0443.2003.00664.x [DOI:10.1111/j.1360-0443.2003.00664.x]
34. Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict. Journal of Child Psychology and Psychiatry. 2007; 48(12):1174–83. doi: 10.1111/j.1469-7610.2007.01812.x [DOI:10.1111/j.1469-7610.2007.01812.x]
35. Wagner KD. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder two randomized controlled trials. JAMA. 2003; 290(8):1033. doi: 10.1001/jama.290.8.1033 [DOI:10.1001/jama.290.8.1033]
36. First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. New York: New York State Psychiatric Institute; 2002. [PMCID]
37. Sharifi V, Assadi SM, Mohammadi MR, Amini H, Kaviani H, Semnani Y, et al. [A Persian translation of the structured clinical interview for diagnostic and statistical manual of mental disorders (Persian)]. Comprehensive Psychiatry. 2009; 50(1):86–91. doi: 10.1016/j.comppsych.2008.04.004 [DOI:10.1016/j.comppsych.2008.04.004]
38. Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children's anxiety: Psychometric properties and comparison with child-report in a clinic and normal sample. Behaviour Research and Therapy. 2004; 42(7):813–39. doi: 10.1016/s0005-7967(03)00200-6 [DOI:10.1016/S0005-7967(03)00200-6]
39. Ishikawa S, Sato H, Sasagawa S. Anxiety disorder symptoms in Japanese children and adolescents. Journal of Anxiety Disorders. 2009; 23(1):104–11. doi: 10.1016/j.janxdis.2008.04.003 [DOI:10.1016/j.janxdis.2008.04.003]
40. Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston: Cengage learning; 2002.
41. Smith KE, Hudson JL. Metacognitive beliefs and processes in clinical anxiety in children. Journal of Clinical Child & Adolescent Psychology. 2013; 42(5):590–602. doi: 10.1080/15374416.2012.755925 [DOI:10.1080/15374416.2012.755925]
42. Puliafico AC, Comer JS, Pincus DB. Adapting parent-child interaction therapy to treat anxiety disorders in young children. Child and Adolescent Psychiatric Clinics of North America. 2012; 21(3):607–19. doi: 10.1016/j.chc.2012.05.005 [DOI:10.1016/j.chc.2012.05.005]
43. Spence SH, Shortt AL. Research review: Can we justify the widespread dissemination of universal, school-based interventions for the prevention of depression among children and adolescents. Journal of Child Psychology and Psychiatry. 2007; 48(6):526–42. doi: 10.1111/j.1469-7610.2007.01738.x [DOI:10.1111/j.1469-7610.2007.01738.x]
44. Stallard P, Sayal K, Phillips R, Taylor JA, Spears M, Anderson R, et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: Pragmatic cluster randomised controlled trial. BMJ. 2012; 345:6058. doi: 10.1136/bmj.e6058 [DOI:10.1136/bmj.e6058]
45. Kortlander E, Kendall PC, Panichelli-Mindel SM. Maternal expectations and attributions about coping in anxious children. Journal of Anxiety Disorders. 1997; 11(3):297–315. doi: 10.1016/s0887-6185(97)00012-1 [DOI:10.1016/S0887-6185(97)00012-1]
46. Shamir-Essakow G, Ungerer JA, Rapee RM. Attachment, behavioral inhibition, and anxiety in preschool children. Journal of Abnormal Child Psychology. 2005; 33(2):131–43. doi: 10.1007/s10802-005-1822-2 [DOI:10.1007/s10802-005-1822-2]
47. Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clinical Psychology Review. 2006; 26(7):834–56. doi: 10.1016/j.cpr.2005.08.001 [DOI:10.1016/j.cpr.2005.08.001]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |