Wed, Jan 28, 2026
| فارسی
Volume 31, Issue 1 (Continuously Updated 2025)
IJPCP 2025, 31(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Keyvan Tabar S, Alimehdi M. Impact of Self-compassion Training on the Severity of Symptoms, Anxiety Sensitivity, and Distress Tolerance in Women with Dermatillomania and Trichotillomania. IJPCP 2025; 31 (1)
URL: http://ijpcp.iums.ac.ir/article-1-4368-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4368-en.html
1- Department of Clinical Psychology, Faculty of Welfare and Health Social Sciences, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran.
2- Department of Clinical Psychology, Faculty of Welfare and Health Social Sciences, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran. ,alimehdi.mansoor@gmail.com
2- Department of Clinical Psychology, Faculty of Welfare and Health Social Sciences, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran. ,
Full-Text [PDF 8679 kb]
(517 Downloads)
| Abstract (HTML) (764 Views)
Full-Text: (641 Views)
Introduction
Body-focused repetitive behaviors (BFRBs) include excessive actions such as pulling, picking, or scratching, encompassing dermatillomania (skin picking), trichotillomania (hair pulling), lip/cheek biting, and nail-biting. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), these behaviors are categorized under obsessive-compulsive disorder (OCD) and related disorders due to their repetitive nature, similar to compulsions observed in OCD. However, there are differences in their triggers and phenomenology, as BFRBs often occur during boredom or specific emotions, unlike OCD, which involves contamination fears. Dermatillomania involves excessive picking, causing open wounds that are prone to infection. It usually begins in adolescence and declines after age 20. Trichotillomania occurs in two styles: automatic (unconscious) and focused (intentional to reduce internal tension). Psychological factors such as anxiety sensitivity (AS) and distress tolerance (DT) significantly affect these disorders. AS refers to fear of anxiety-related sensations, and DT refers to the ability to endure negative emotional states. Low DT leads to maladaptive behaviors to temporarily escape discomfort.
Self-compassion therapy, a third-wave psychological intervention, emphasizes being kind and nonjudgmental toward oneself, recognizing shared human struggles. It has shown efficacy in treating depression, anxiety, and OCD by reducing distress and promoting psychological resilience. This study aims to examine the effectiveness of self-compassion therapy on the severity of symptoms, AS, and DT in women with dermatillomania and trichotillomania.
Methods
This is a quasi-experimental study with a pre-test/post-test/follow-up design. The study population consisted of female patients with dermatillomania and trichotillomania referred to psychology clinics in Tehran, Iran, in 2024. A total of 30 eligible patients were purposefully selected and randomly assigned to intervention (n=15) and control (n=15) groups. Inclusion criteria were the diagnosis of dermatillomania and trichotillomania based on the DSM-5 criteria, age 20-35 years, and having the disorder for at least six months. Data collection tools included Floyd et al.’s [23] anxiety sensitivity index (ASI), Simons and Gaher’s DT scale (DTS), the Massachusetts general hospital hairpulling scale (MGH-HPS), and Keuthen et al.’s [28] skin picking scale (SPS). The intervention group underwent eight 45-min sessions of self-compassion training based on Gilbert’s protocol, while the control group received no intervention. The data were analyzed using the repeated measures ANOVA.
Results
The mean scores of the variables for the two groups are presented in Table 1.
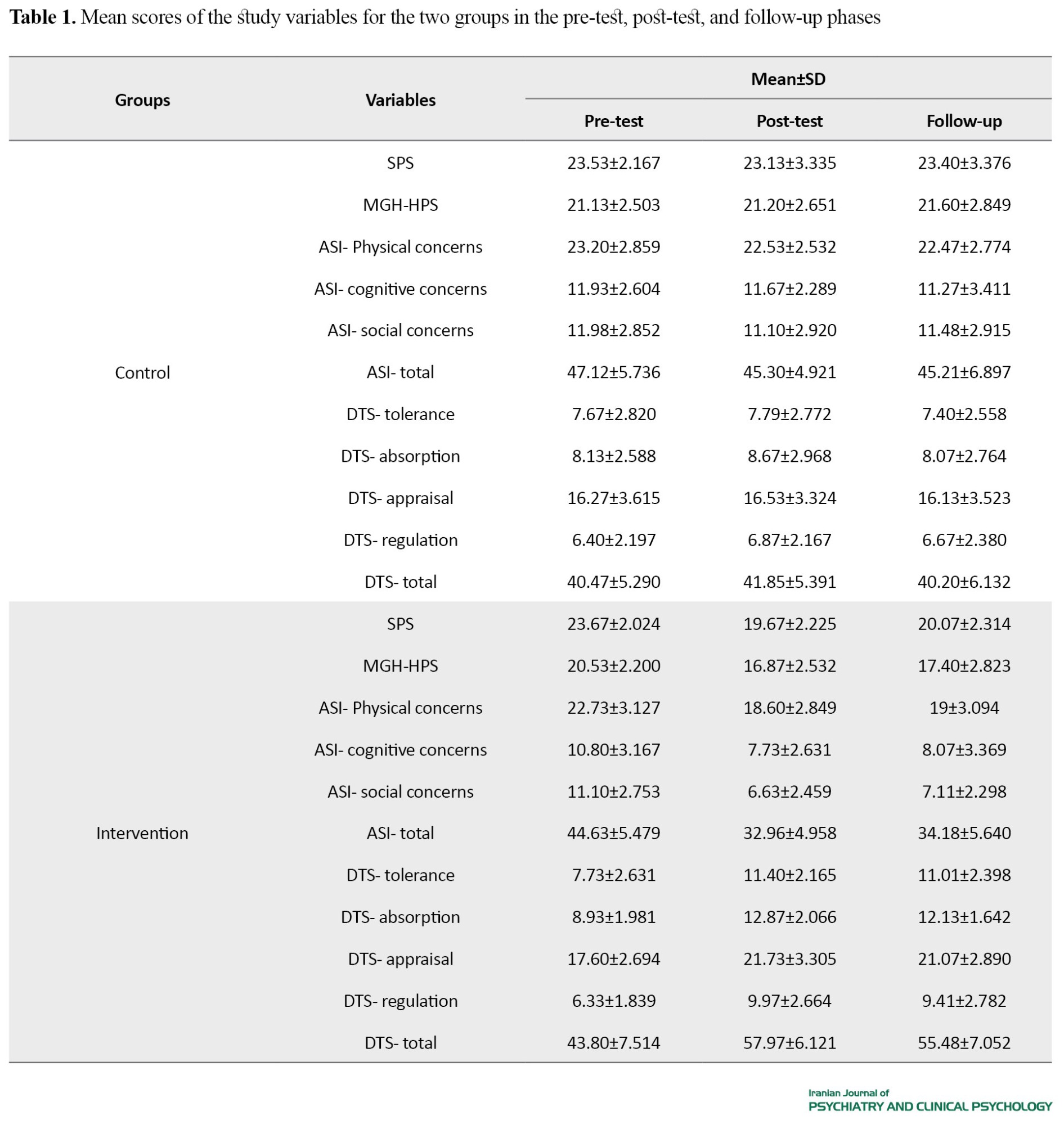
The results of repeated measures ANOVA for comparing two groups in SPS and MGH-HPS scores in the three phases of pre-test, post-test, and follow-up are reported in Table 2.
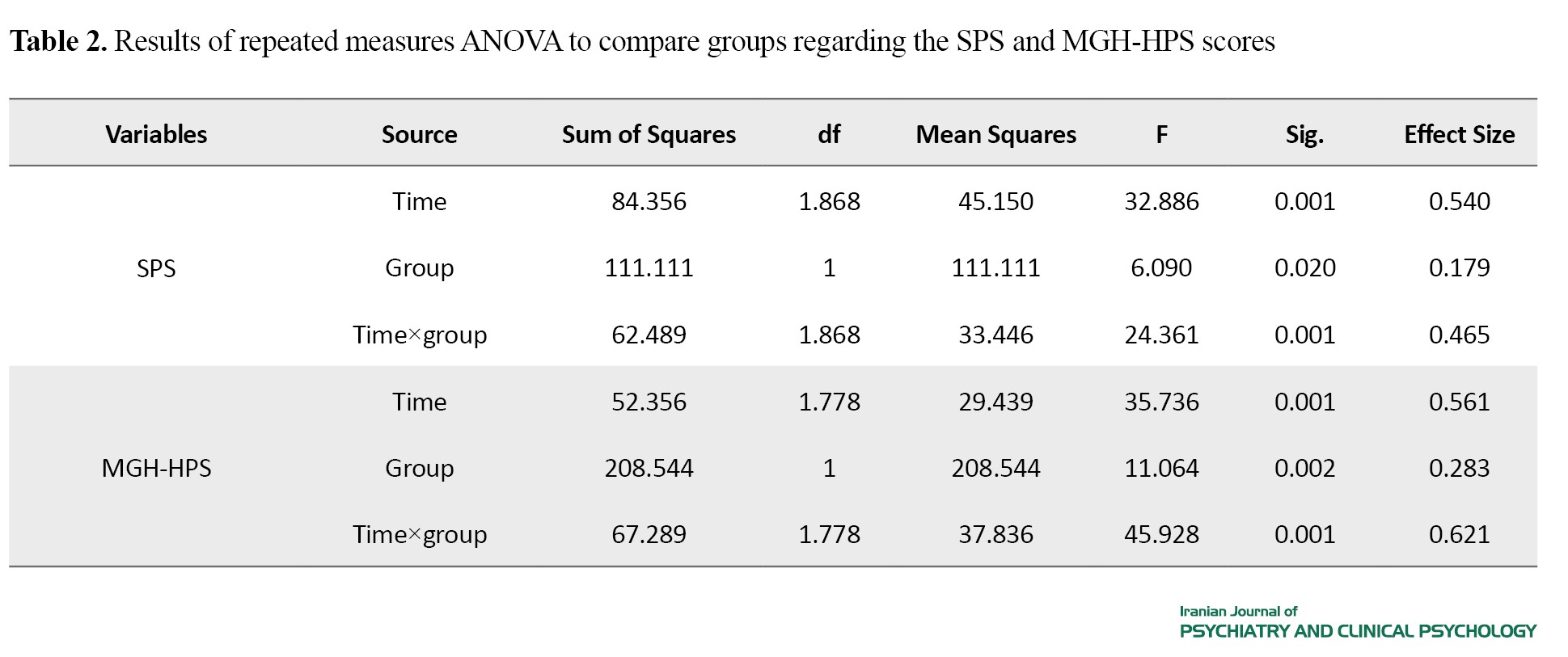
Based on the findings, the difference between the two groups in the scores of SPS (P=0.020) and MGH-HPS (P=0.002) was significant in three phases. Approximately 17.9% and 28.3% of the differences in the SPS and MGH-HPS scores were related to the group factor, respectively. In addition, the main effect and the interaction effect of time and group were significant on all study variables (P<0.05). In other words, the difference in the SPS and MGH-HPS scores between the two groups over time was significant. Based on the findings, the differences between the two groups in the scores of ASI and DTS domains were also significant in three phases (P<0.05). The main effect and the interaction effect of time and group were also significant on all ASI and DTS domains (P<0.01).
Conclusions
The self-compassion training is effective in reducing symptoms and AS, and improving DT in women with dermatillomania and trichotillomania. The self-compassion programs should be used through organized workshops to improve DT and reduce AS in these women. Further research should be conducted using qualitative methods and exploring other psychological factors affecting the severity of dermatillomania and trichotillomania symptoms in women.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Islamic Azad University, Tehran Medical Sciences Branch (IR.IAU.TMU.REC.1403.108) and was registered by the Iranian Registry of Clinical Trials (ID: IRCT20241019063416N). Informed consent was obtained from all participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, methodology, investigation, review & editing, resources: Sahar Keyvan Tabar and Mansoor Alimehdi; Writing original draft: Sahar Keyvan Tabar; Supervision, and project administration: Mansoor Alimehdi.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
The authors would like to thank the Parseh Clinic in Tehran and all participants for their cooperation in this study.
Body-focused repetitive behaviors (BFRBs) include excessive actions such as pulling, picking, or scratching, encompassing dermatillomania (skin picking), trichotillomania (hair pulling), lip/cheek biting, and nail-biting. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), these behaviors are categorized under obsessive-compulsive disorder (OCD) and related disorders due to their repetitive nature, similar to compulsions observed in OCD. However, there are differences in their triggers and phenomenology, as BFRBs often occur during boredom or specific emotions, unlike OCD, which involves contamination fears. Dermatillomania involves excessive picking, causing open wounds that are prone to infection. It usually begins in adolescence and declines after age 20. Trichotillomania occurs in two styles: automatic (unconscious) and focused (intentional to reduce internal tension). Psychological factors such as anxiety sensitivity (AS) and distress tolerance (DT) significantly affect these disorders. AS refers to fear of anxiety-related sensations, and DT refers to the ability to endure negative emotional states. Low DT leads to maladaptive behaviors to temporarily escape discomfort.
Self-compassion therapy, a third-wave psychological intervention, emphasizes being kind and nonjudgmental toward oneself, recognizing shared human struggles. It has shown efficacy in treating depression, anxiety, and OCD by reducing distress and promoting psychological resilience. This study aims to examine the effectiveness of self-compassion therapy on the severity of symptoms, AS, and DT in women with dermatillomania and trichotillomania.
Methods
This is a quasi-experimental study with a pre-test/post-test/follow-up design. The study population consisted of female patients with dermatillomania and trichotillomania referred to psychology clinics in Tehran, Iran, in 2024. A total of 30 eligible patients were purposefully selected and randomly assigned to intervention (n=15) and control (n=15) groups. Inclusion criteria were the diagnosis of dermatillomania and trichotillomania based on the DSM-5 criteria, age 20-35 years, and having the disorder for at least six months. Data collection tools included Floyd et al.’s [23] anxiety sensitivity index (ASI), Simons and Gaher’s DT scale (DTS), the Massachusetts general hospital hairpulling scale (MGH-HPS), and Keuthen et al.’s [28] skin picking scale (SPS). The intervention group underwent eight 45-min sessions of self-compassion training based on Gilbert’s protocol, while the control group received no intervention. The data were analyzed using the repeated measures ANOVA.
Results
The mean scores of the variables for the two groups are presented in Table 1.
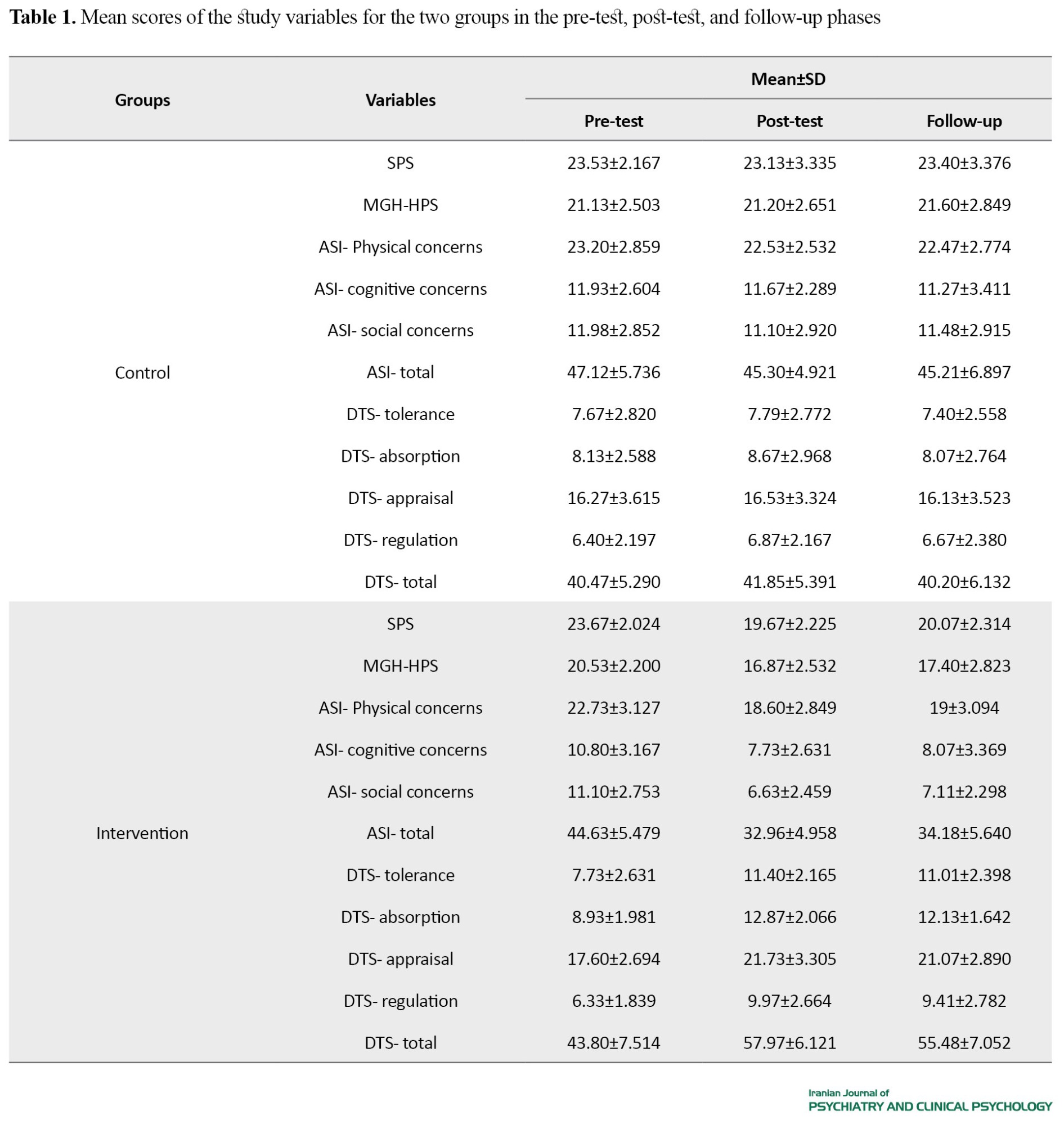
The results of repeated measures ANOVA for comparing two groups in SPS and MGH-HPS scores in the three phases of pre-test, post-test, and follow-up are reported in Table 2.
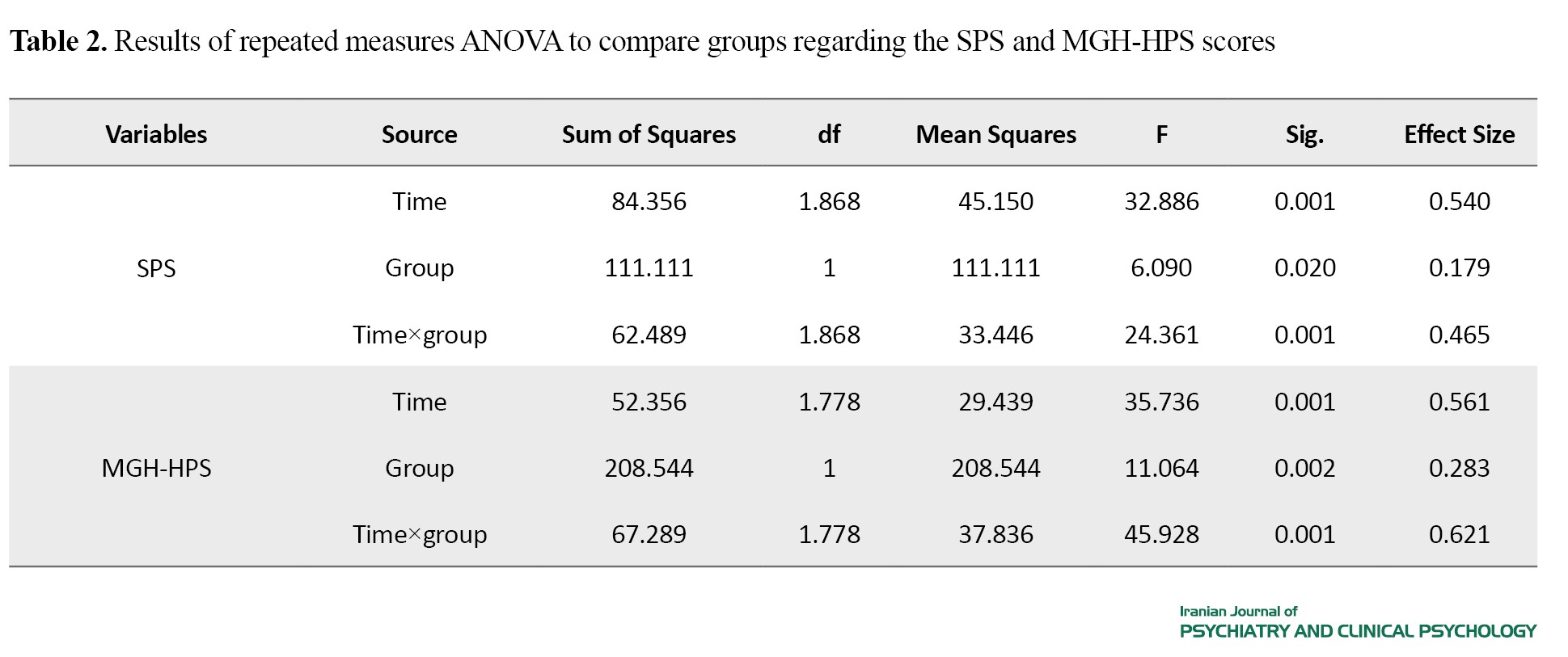
Based on the findings, the difference between the two groups in the scores of SPS (P=0.020) and MGH-HPS (P=0.002) was significant in three phases. Approximately 17.9% and 28.3% of the differences in the SPS and MGH-HPS scores were related to the group factor, respectively. In addition, the main effect and the interaction effect of time and group were significant on all study variables (P<0.05). In other words, the difference in the SPS and MGH-HPS scores between the two groups over time was significant. Based on the findings, the differences between the two groups in the scores of ASI and DTS domains were also significant in three phases (P<0.05). The main effect and the interaction effect of time and group were also significant on all ASI and DTS domains (P<0.01).
Conclusions
The self-compassion training is effective in reducing symptoms and AS, and improving DT in women with dermatillomania and trichotillomania. The self-compassion programs should be used through organized workshops to improve DT and reduce AS in these women. Further research should be conducted using qualitative methods and exploring other psychological factors affecting the severity of dermatillomania and trichotillomania symptoms in women.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Islamic Azad University, Tehran Medical Sciences Branch (IR.IAU.TMU.REC.1403.108) and was registered by the Iranian Registry of Clinical Trials (ID: IRCT20241019063416N). Informed consent was obtained from all participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, methodology, investigation, review & editing, resources: Sahar Keyvan Tabar and Mansoor Alimehdi; Writing original draft: Sahar Keyvan Tabar; Supervision, and project administration: Mansoor Alimehdi.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
The authors would like to thank the Parseh Clinic in Tehran and all participants for their cooperation in this study.
References
- Moritz S, Scheunemann J, Jelinek L, Penney D, Schmotz S, Hoyer L, et al. Prevalence of body-focused repetitive behaviors in a diverse population sample- rates across age, gender, race and education. Psychological Medicine. 2024; 54(8):1552-8. [DOI:10.1017/S0033291723003392] [PMID]
- Faroughi P, Khanjani Z, Hashemi T, Mahmoud-Aliloo M. [Effectiveness of acceptance enhanced behavior therapy on body focused repetitive behavior disorders (Trichotillomania, Skin Picking, Nail Biting): A multiple baseline design with three month follow-up (Persian)]. Journal of Research in Psychological Health. 2017; 11(3):13-27. [DOI:10.29252/rph.11.3.13]
- Duke DC, Keeley ML, Geffken GR, Storch EA. Trichotillomania: A current review. Clinical Psychology Review. 2010; 30(2):181-93. [DOI:10.1016/j.cpr.2009.10.008] [PMID]
- Khan S, Hughes S, Hill O. N-acetyl cysteine supplementation to alleviate skin picking disorder: A case report. Cureus. 2024; 16(2):e53440. [DOI:10.7759/cureus.53440]
- Grant JE, Chamberlain SR. Characteristics of 262 adults with skin picking disorder. Comprehensive Psychiatry. 2022; 117:152338. [DOI:10.1016/j.comppsych.2022.152338] [PMID]
- Hamid N, Bordbar M, Marashy SA. The effectiveness of habit reversal training with cognitive behavior therapy on quality of life and symptoms of trichotillomania patients. Medical Journal of Tabriz University of Medical Sciences. 2022; 44(2):116-26. [DOI:10.34172/mj.2022.021]
- Flessner CA, Conelea CA, Woods DW, Franklin ME, Keuthen NJ, Cashin SE. Styles of pulling in trichotillomania: Exploring differences in symptom severity, phenomenology, and functional impact. Behaviour Research and Therapy. 2008; 46(3):345-57. [DOI:10.1016/j.brat.2007.12.009] [PMID]
- du Toit PL, van Kradenburg J, Niehaus D, Stein DJ. Comparison of obsessive-compulsive disorder patients with and without comorbid putative obsessive-compulsive spectrum disorders using a structured clinical interview. Comprehensive Psychiatry. 2001; 42(4):291-300. [DOI:10.1053/comp.2001.24586] [PMID]
- Georgiadis C, Schreck M, Gervasio M, Kemp J, Freeman J, Garcia A, et al. Disgust propensity and sensitivity in childhood anxiety and obsessive-compulsive disorder: Two constructs differentially related to obsessional content. Journal of Anxiety Disorders. 2020; 76:102294. [DOI:10.1016/j.janxdis.2020.102294] [PMID]
- McKay D, Yang H, Elhai J, Asmundson GJG. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: The moderating role of disgust propensity and sensitivity.Journal of Anxiety Disorders. 2020; 73:102233. [DOI:10.1016/j.janxdis.2020.102233] [PMID]
- Grant JE, Collins M, Chamberlain SR, Chesivoir E. Disorders of impulsivity in trichotillomania and skin picking disorder. Journal of Psychiatric Research. 2024; 170:42-6. [DOI:10.1016/j.jpsychires.2023.12.011] [PMID]
- Akbari M, Seydavi M, Firoozabadi MA, Babaeifard M. Distress tolerance and lifetime frequency of non-suicidal self-injury (NSSI): A systematic review and meta-analysis. Clinical Psychology & Psychotherapy. 2024; 31(1):e2957. [DOI:10.1002/cpp.2957] [PMID]
- Hsu T, Thomas EBK, Welch EK, O'Hara MW, McCabe JE. Examining the structure of distress tolerance: Are behavioral and self-report indicators assessing the same construct? Journal of Contextual Behavioral Science. 2023; 27:143-51. [DOI:10.1016/j.jcbs.2023.02.001] [PMID]
- Xie Q, Guan Y, Hofmann SG, Jiang T, Liu X. The potential mediating role of anxiety sensitivity in the impact of mindfulness training on anxiety and depression severity and impairment: A randomized controlled trial. Scandinavian Journal of Psychology. 2023; 64(1):21-9.[DOI:10.1111/sjop.12860] [PMID]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005; 29(2):83-102. [DOI:10.1007/s11031-005-7955-3]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: The association with distress tolerance and anxiety sensitivity. Behavior Therapy. 2010; 41(4):567-74. [DOI:10.1016/j.beth.2010.04.002] [PMID]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro T. Distress Tolerance: Theory, measurement, and relations to psychopathology. Current Directions in Psychological Science. 2010; 19(6):406-10. [DOI:10.1177/0963721410388642] [PMID]
- Neff KD. Self-compassion: Theory, method, research, and intervention. Annual Review of Psychology. 2023; 74:193-218. [DOI:10.1146/annurev-psych-032420-031047] [PMID]
- Miyagawa Y, Neff KD. How self-compassion operates within individuals: An examination of latent profiles of state self-compassion in the US and Japan. Mindfulness. 2023; 14(6):1371-82. [DOI:10.1007/s12671-023-02143-2]
- Reilly EB, Stuyvenberg CL. A meta-analysis of loving-kindness meditations on self-compassion. Mindfulness. 2023; 14(10):2299-310. [DOI:10.1007/s12671-022-01972-x]
- Alimehdi M, khosravi N. [The effectiveness of self-compassion training on anxiety sensitivity, uncertainty intolerance and psychological distress in people with social anxiety (Persian)]. Clinical Psychology Achievements. 2022; 8(1):1-14. [DOI:10.22055/jacp.2023.43478.1289]
- Peterson RA, Plehn K. Measuring anxiety sensitivity. In: Taylor S, editor. Anxiety Sensitivity. New York: Routledge; 2014. [DOI:10.4324/9781410603326]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity index (ASI). In: Roemer L, Antony MM, Orsillo MS, editors.Practitioner's guide to empirically based measures of anxiety. Dordrecht: Kluwer Academic/Plenum Publishers; 2001. [Link]
- Beirami M, Akbari E, Qasempour A, Azimi Z. [An investigation of anxiety sensitivity, meta-worry and components of emotion regulation in students with and without social Anxiety (Persian)]. Clinical Psychology Studies. 2012; 3(8):40-69. [Link]
- Mashhadi A, Gasempoor A, Akbari E, ElBeigi R, Hasanzadeh S. [The role of anxiety sensitivity and emotion regulation in prediction of students social anxiety disorder (Persian)]. Knowledge Research Applied Psychology. 2013; 14(2):89-99. [Link]
- Alavi SS. Psychometric properties of Young internet addiction test. International Journal of Behavioral Sciences. 2010; 4(3):183-9.[Link]
- Alavi SS, Alaghemandan H, Maracy MR, Jannatifard F, Eslami M, Ferdosi M. Impact of addiction to internet on a number of psychiatric symptoms in students of Isfahan Universities, Iran, 2010. Int J Prev Med. 2012; 3(2):122-7. [PMID]
- Keuthen NJ, O'Sullivan RL, Ricciardi JN, Shera D, Savage CR, Borgmann AS, et al. The Massachusetts General Hospital (MGH) Hairpulling Scale: I. development and factor analyses. Psychotherapy and Psychosomatics. 1995; 64(3-4):141-5. [DOI:10.1159/000289003] [PMID]
- Selles RR, McGuire JF, Small BJ, Storch EA. A systematic review and meta-analysis of psychiatric treatments for excoriation (skin-picking) disorder. General Hospital Psychiatry. 2016; 41:29-37. [DOI:10.1016/j.genhosppsych.2016.04.001] [PMID]
- Rahman SM, Jafferany M, Barkauskaite R. Habit-reversal training: a psychotherapeutic approach in treating body-focused repetitive behaviour disorders. Clinical and Experimental Dermatology. 2023; 48(12):1310-6. [DOI:10.1093/ced/llad247]
- O'Sullivan RL, Keuthen NJ, Hayday CF, Ricciardi JN, Buttolph ML, Jenike MA, et al. The Massachusetts General Hospital (MGH) Hairpulling Scale: 2. reliability and validity. Psychotherapy and Psychosomatics. 1995; 64(3-4):146-8. [DOI:10.1159/000289004] [PMID]
- Keuthen NJ, Wilhelm S, Deckersbach T, Engelhard IM, Forker AE, Baer L, et al. The Skin Picking Scale: Scale construction and psychometric analyses.Journal of Psychosomatic Research. 2001; 50(6):337-41. [DOI:10.1016/S0022-3999(01)00215-X] [PMID]
- Rautio D, Andrén P, Bjureberg L, Silverberg-Mörse M, Mataix-Cols D, Fernández de la Cruz L. Body-focused repetitive behavior disorders in children and adolescents: Clinical characteristics and treatment outcomes in a naturalistic setting. Behavior Therapy. 2024; 55(2):376-90. [PMID]
- Grant JE, Chamberlain SR. Clinical correlates of symptom severity in skin picking disorder. Comprehensive Psychiatry. 2017; 78:25-30. [DOI:10.1016/j.comppsych.2017.07.001] [PMID]
- Gilbert P. A New Approach to Life's Challenges. London: Constable & Robinson; 2010. [Link]
- Mirmoeini P, Bayazi M, Khalatbari J. Comparing the effectiveness of acceptance and commitment therapy and compassion-focused therapy on worry severity and loneliness among patients with multiple sclerosis. Internal Medicine Today. 2021; 27(4):534-49. [DOI:10.32598/hms.27.4.3426.1]
- Millard LA, Wan MW, Smith DM, Wittkowski A. The effectiveness of compassion focused therapy with clinical populations: A systematic review and meta-analysis. Journal of Affective Disorders. 2023; 326:168-92. [DOI:10.1016/j.jad.2023.01.010] [PMID]
- Beaumont E, Hollins Martin CJ. A narrative review exploring the effectiveness of Compassion-Focused Therapy. Counselling Psychology Review. 2015; 30(1):21-32. [DOI:10.53841/bpscpr.2015.30.1.21]
- Wilson AC, Mackintosh K, Power K, Chan SW. Effectiveness of self-compassion related therapies: A systematic review and meta-analysis. Mindfulness. 2019; 10:979-95. [DOI:10.1007/s12671-018-1037-6]
- Li Y, Ju R, Hofmann SG, Chiu W, Guan Y, Leng Y, et al. Distress tolerance as a mechanism of mindfulness for depression and anxiety: Cross-sectional and diary evidence. International Journal of Clinical and Health Psychology. 2023; 23(4):100392. [DOI:10.1016/j.ijchp.2023.100392] [PMID]
- Germer CK, Neff KD. Self-compassion in clinical practice. Journal of Clinical Psychology. 2013; 69(8):856-67. [PMID]
- Aboutalebi H, Yazdchi N, Smkhani Akbarinejhad H. [Effectiveness of compassion-focused therapy on death anxiety and quality of life among women with multiple sclerosis (Persian)]. Medical Sciences. 2022; 32(1):92-101. [DOI:10.52547/iau.32.1.92]
- Khedri M, Shiralinia K, Aslani K. [Effectiveness of Mindful Self-Compassion training on reducing rumination and perceived stress in adolescent girls (Persian)]. Applied Psychology. 2022; 16(2):223-01. [DOI:10.52547/apsy.2021.219957.1000]
- Taher Pour M, Sohrabi A, Zemestani M. Effectiveness of compassion- focused therapy on depression, anxiety, stress, and weight self-efficacy in patients with eating disorder. Journal of Sabzevar University of Medical Sciences. 2019; 26(4):505-13. [Link]
- Baumgardner M, Benoit Allen K. Integrating cognitive-behavioral therapy with compassion-focused therapy for the treatment of social anxiety disorder: An evidence-based case study. Clinical Case Studies. 2024; 23(2):127-45. [DOI:10.1177/15346501231197403]
- Mirzakhani M, Gharraee B, Zahedi Tajrishi K, Khanjani S, Noorbala AA, Safaei Nodehi SR. [Effect of compassion-focused therapy on depression, anxiety, stress, and quality of life in patients with cancer: A clinical trial (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2023; 29(2):142-55. [DOI:10.32598/ijpcp.29.2.4462.1]
- Miller JT, Verhaeghen P. Mind full of kindness: Self-awareness, self-regulation, and self-transcendence as vehicles for compassion. BMC Psychology. 2022; 10(1):188. [DOI:10.1186/s40359-022-00888-4] [PMID]
- Ramsey A, Govind T, Lam JA, Palmer BW, Jeste DV, Lee EE. Self-compassion, but not compassion toward others, is associated with better physical health: A cross-sectional study. Schizophrenia Research. 2023; 255:17-23. [DOI:10.1016/j.schres.2023.03.017] [PMID]
- Mousavi SM, Khajevand Khoshli A, Asadi J, Abdollahzadeh H. [Comparison of the effectiveness of compassion-focused therapy and acceptance and commitment therapy on distress tolerance in women with systemic lupus erythematosus (Persian)]. Journal of Psychological Science. 2021; 20(99):453-60. [Link]
- Niasti N, Shiroudi Sh, Khalatbari J, Tizdast T. [Determining the effectiveness of compassion-focused treatment package, emotion-focused therapy and acceptance and commitment therapy on distress tolerance among adolescents with aggressive behaviors: A pilot study (Persian)]. Community Health. 2021; 8(3):496-508.[Link]
- Karami P, Ghanifar MH, Ahi G. Comparing the effectiveness of cognitive behavioral therapy and compassion-focused therapy in improving distress tolerance and self-compassion in women with experiences of marital infidelity. Journal of Assessment and Research in Applied Counseling. 2024; 6(2):27-35. [DOI:10.61838/kman.jarac.6.2.4]
- Esmaeili L, Amiri S, Reza Abedi M, Molavi H. [The effect of acceptance and commitment therapy focused on self-compassion on social anxiety of adolescent girls (Persian)]. Clinical Psychology Studies. 2018; 9(30):117-37. [DOI:10.22054/jcps.2018.8605]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/11/20 | Accepted: 2025/05/17 | Published: 2025/08/1
Received: 2024/11/20 | Accepted: 2025/05/17 | Published: 2025/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |