Sun, Feb 15, 2026
| فارسی
Volume 30, Issue 1 (Continuously Updated 2024)
IJPCP 2024, 30(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sharifi P, Roaya M A, Dehghan M. The Moderating Role of Illness Identity in the Relationship between Pain Self-Efficacy and Quality of Life in Patients with Multiple Sclerosis. IJPCP 2024; 30 (1) : 4475.1
URL: http://ijpcp.iums.ac.ir/article-1-4238-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4238-en.html
1- Department of Psychology, Faculty of Letters and Humanities, Urmia University, Urmia, Iran.
2- Department of Health Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
3- Department of Health Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran. ,dehghan.mo@iums.ac.ir
2- Department of Health Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
3- Department of Health Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 5441 kb]
(607 Downloads)
| Abstract (HTML) (1805 Views)
Full-Text: (628 Views)
Introduction
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system that leads to demyelination and neurodegeneration [3]. Due to its ambiguous, chronic, and life-altering nature, especially in the early stages, MS induces significant levels of distress in affected individuals [3]. This condition can reduce the quality of life (QoL) of patients [5]. The World Health Organization defines QoL as an individual’s perception of their position in life within the cultural and value systems in which they live, and in relation to their goals, expectations, standards, and concerns [6]. Living with a person suffering from MS can disrupt the QoL [7], and studying its antecedent factors is of great importance. Based on the social cognitive approach, the potential antecedents of QoL in individuals with MS may include their perceptions and beliefs about their disease, which can be the constructs such as pain self-efficacy (PSE) and illness identity. The PSE refers to an individual’s belief in their capacity to manage pain symptoms, minimize its impact on daily life, and maintain functionality despite pain [9, 10]. Pain is a common symptom of MS [11], and is experienced by more than 75% of MS people [12]. Examining the effects of PSE in people with MS is important. Illness identity is important in facing chronic illnesses. There are four illness identity types: Rejection, engulfment, acceptance, and enrichment. Their relationship with psychological and physical functioning in chronic physical conditions has been examined in previous studies [22]. Illness identity is a relatively new concept in health psychology and has been studied so far in cases such as people with cardiac disease [23, 24], multisystem connective tissue disorders [23], and epilepsy [25].
The literature review indicates that the experience of MS affects individuals’ beliefs and perceptions about themselves. Understanding the extent to which PSE and each of the four illness identity types explain QoL among people with MS can help health psychologists in designing interventions aimed at improving QoL. However, there is a research gap in this area. Therefore, this study aimed to examine the relationship of PSE and illness identity with QoL among individuals with MS and to assess the moderating role of illness identity in the relationship between PSE and QoL.
Methods
This is a correlational study with a cross-sectional design. The study population included all individuals with MS referred to Sina and Asia hospitals in Tehran, Iran, from November 16, 2023 to June 20, 2024. Using G*Power software (effect size=0.15, α=0.05, test power=0.95), the sample size was estimated at 138, but finally 166 participants were included in the study. Inclusion criteria were the MS diagnosis and age 18-60 years. Exclusion criteria were a prior psychiatric diagnosis before MS and diagnosis of comorbid chronic diseases (based on the patient’s medical records).
For data collection, a demographic form (surveying age, gender, educational level, marital status, duration of illness, and type of MS), the Persian version of the World Health Organization Quality of Life Questionnaire- Brief version [26], the Persian version of the Pain Self-Efficacy Questionnaire [27], and the Persian version of the Illness Identity Questionnaire (IIQ) [22] were employed.
Six participants were excluded during data collection due to outlier data, resulting in a final sample size of 160. Pearson’s correlation test and hierarchical regression analysis (with and without adjusting for age) were utilized for data analysis. Additionally, independent t-test was used to compare the mean QoL based on gender, and a one-way ANOVA was conducted to compare the mean QoL based on other demographic variables.
Results
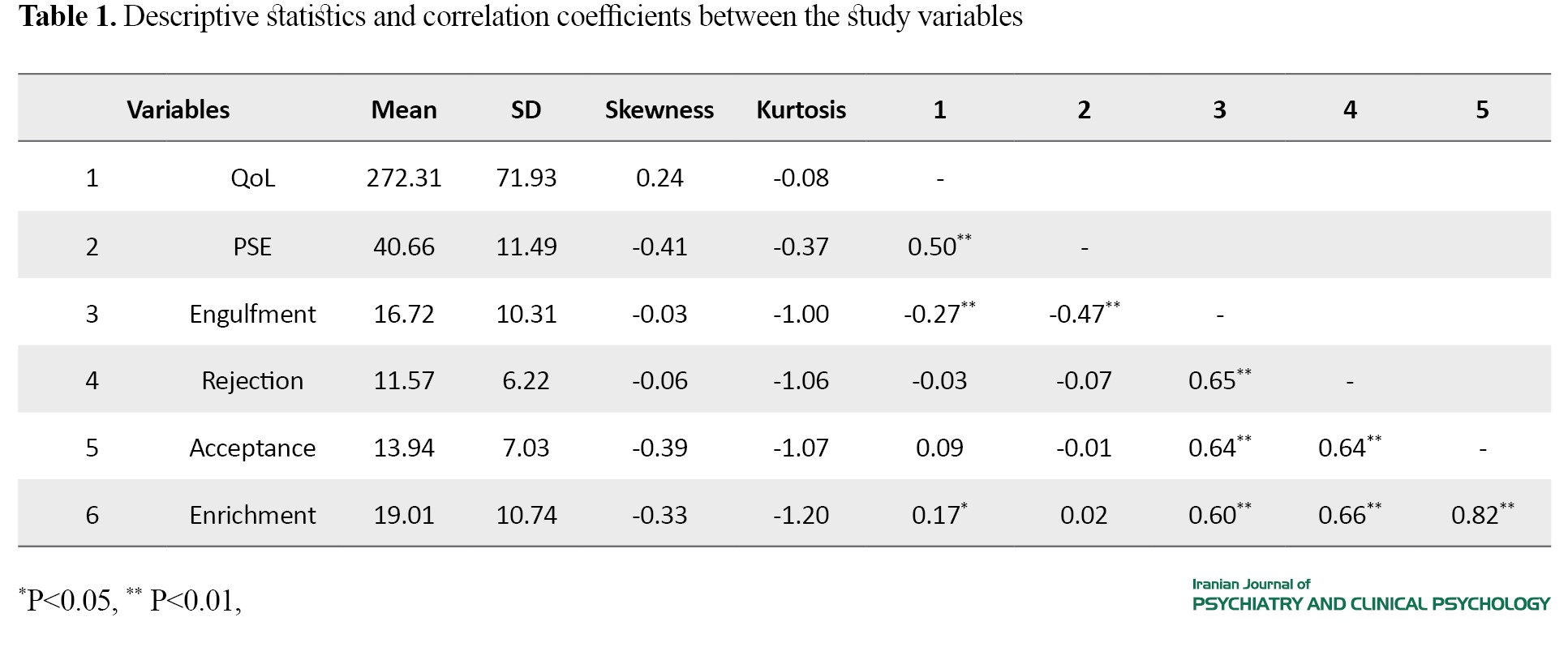
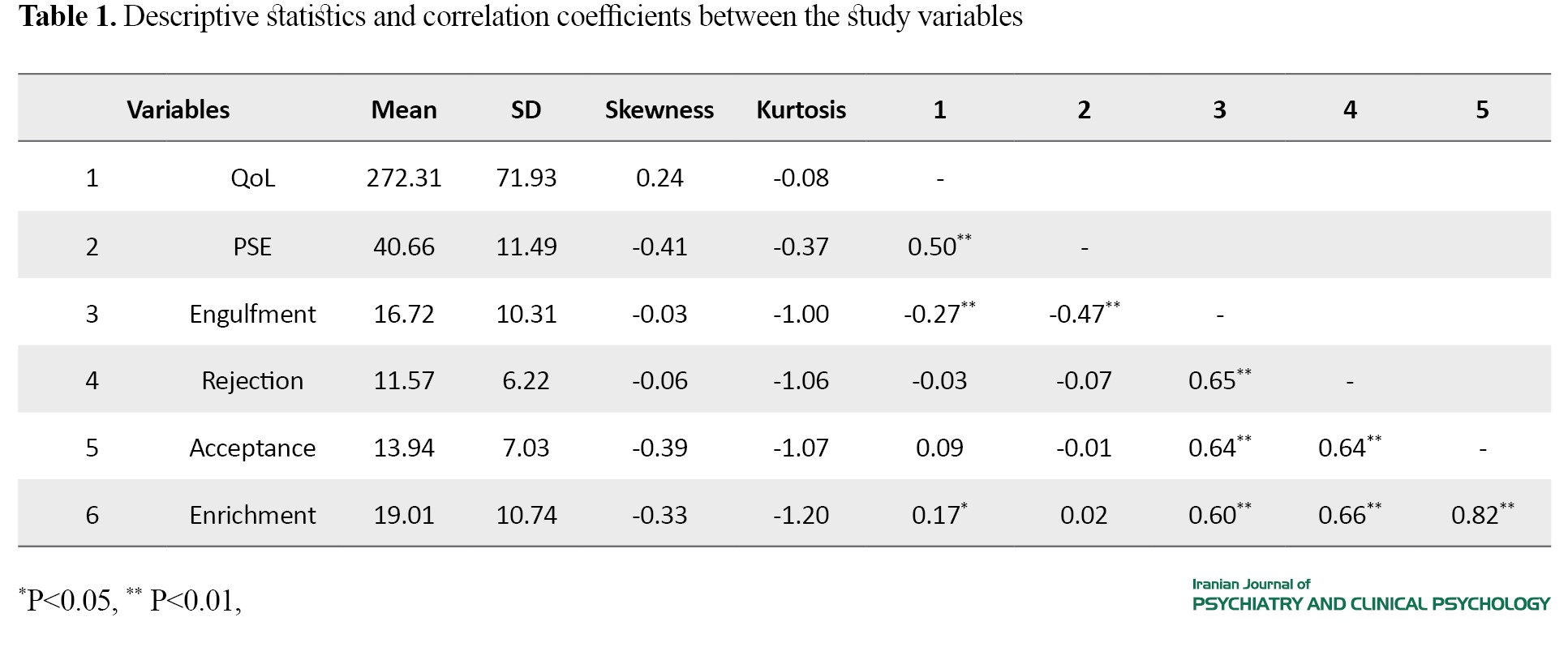
The mean age of participants was 37.16±8.63 years, ranged 18-57 years. They included 107 females and 51 males. Additionally, 42 had a high school diploma or lower education, 82 had an associate/bachelor’s degree, and 32 had a master’s/doctoral degree. Regarding marital status, 49 were single, 97 were married, and 12 were divorced. Concerning the MS types, 63 had relapsing-remitting MS (RRMS), 67 primary progressive MS (PPMS), and 28 secondary progressive MS (SPMS). In terms of illness duration, 44 had been diagnosed for less than 2 years, 26 for 2-5 years, 43 for 5-10 years, and 45 for >10 years. Descriptive statistics for each variable, as well as the correlation coefficients are reported in Table 1.
Given the significant correlation between age and QoL, two hierarchical regressions were conducted to assess the role of independent and moderating variables in predicting QoL (with and without adjusting for the effect of age on QoL). Each hierarchical regression was conducted in three steps (or models). In the first step, PSE was entered into the equation. In the second step, the four types of illness identity were added. In the third step, four new variables (interaction of PSE with the illness identity types)were included in the model (Tables 2 and 3).
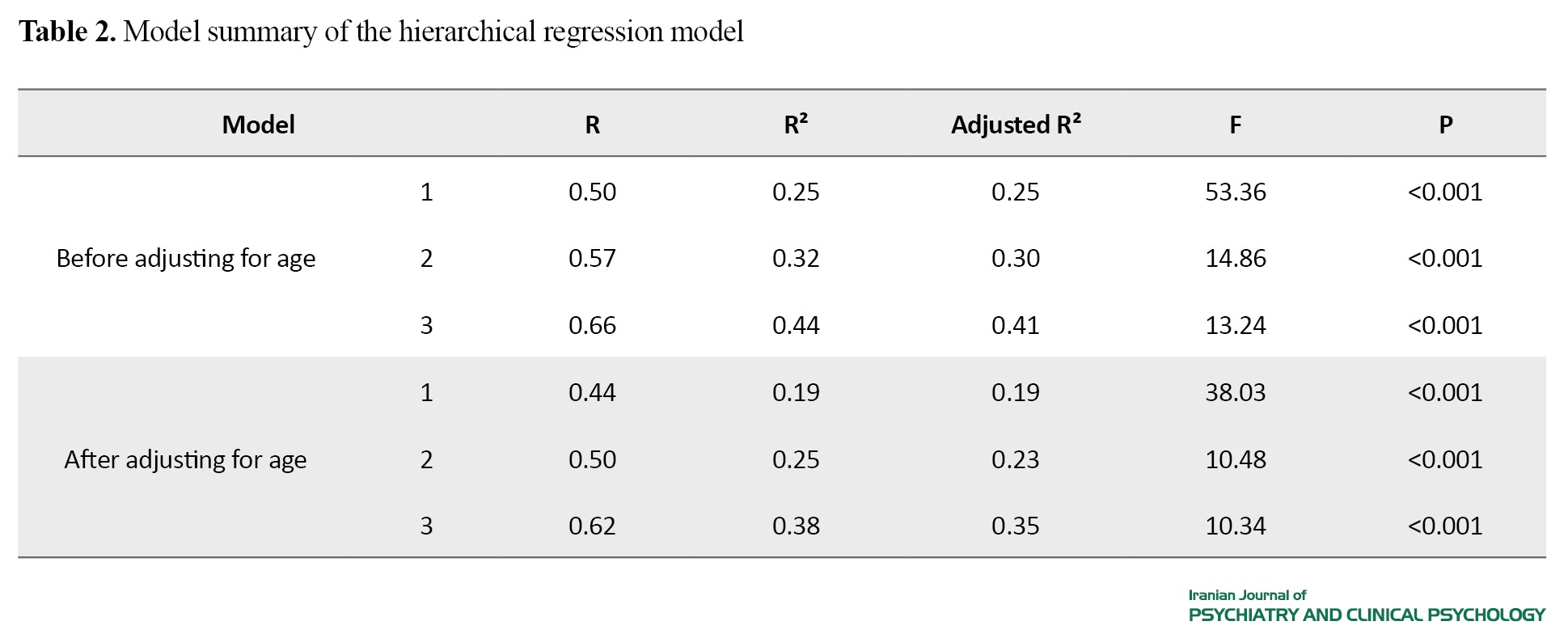
According to the results in Table 2, the third study model explained 44% of the variance in QoL before adjusting for age. However, this decreased to 38% after adjusting for age. Nevertheless, this model retained significant power in explaining the variance of QoL, even after adjusting for the effect of age.
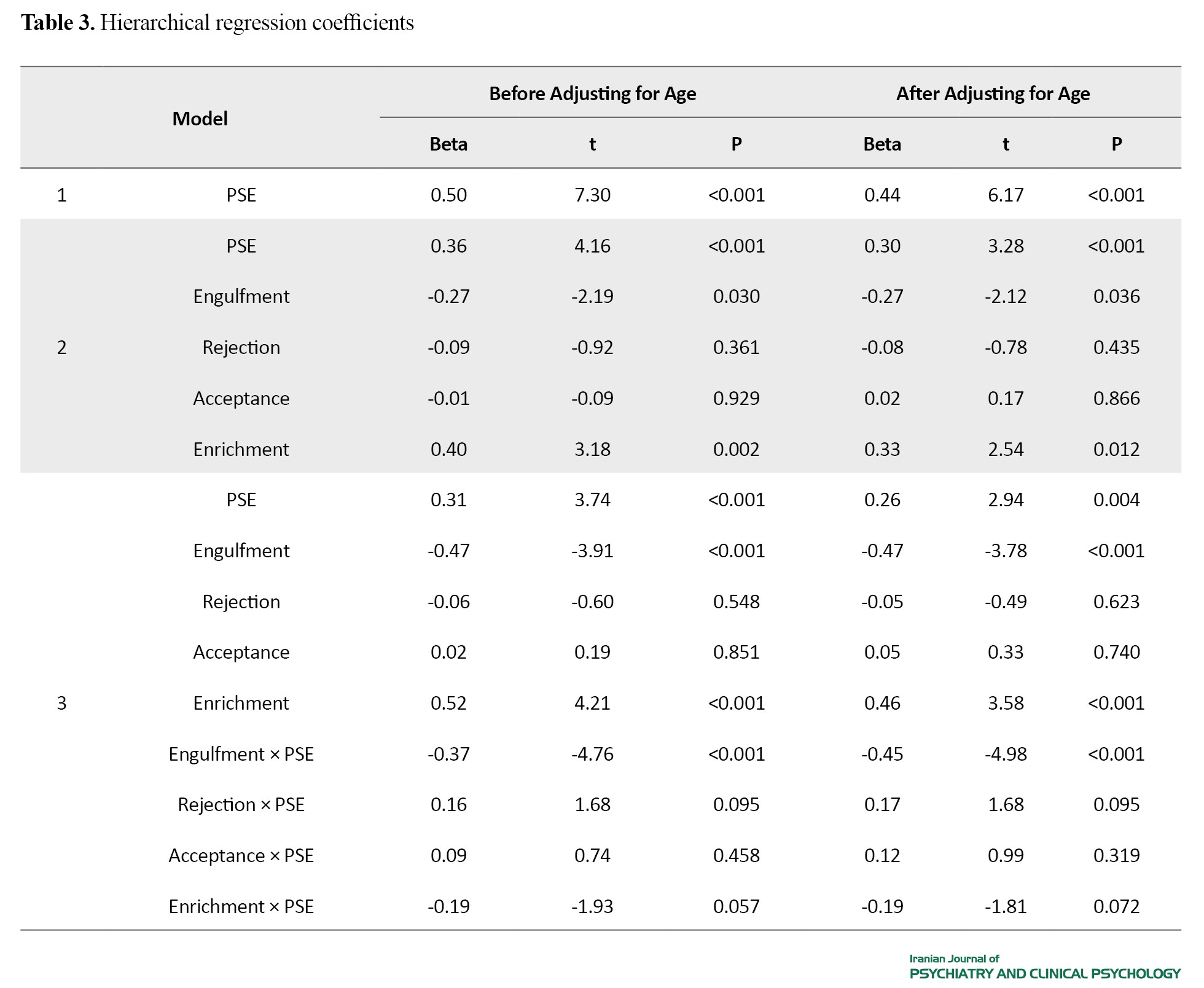
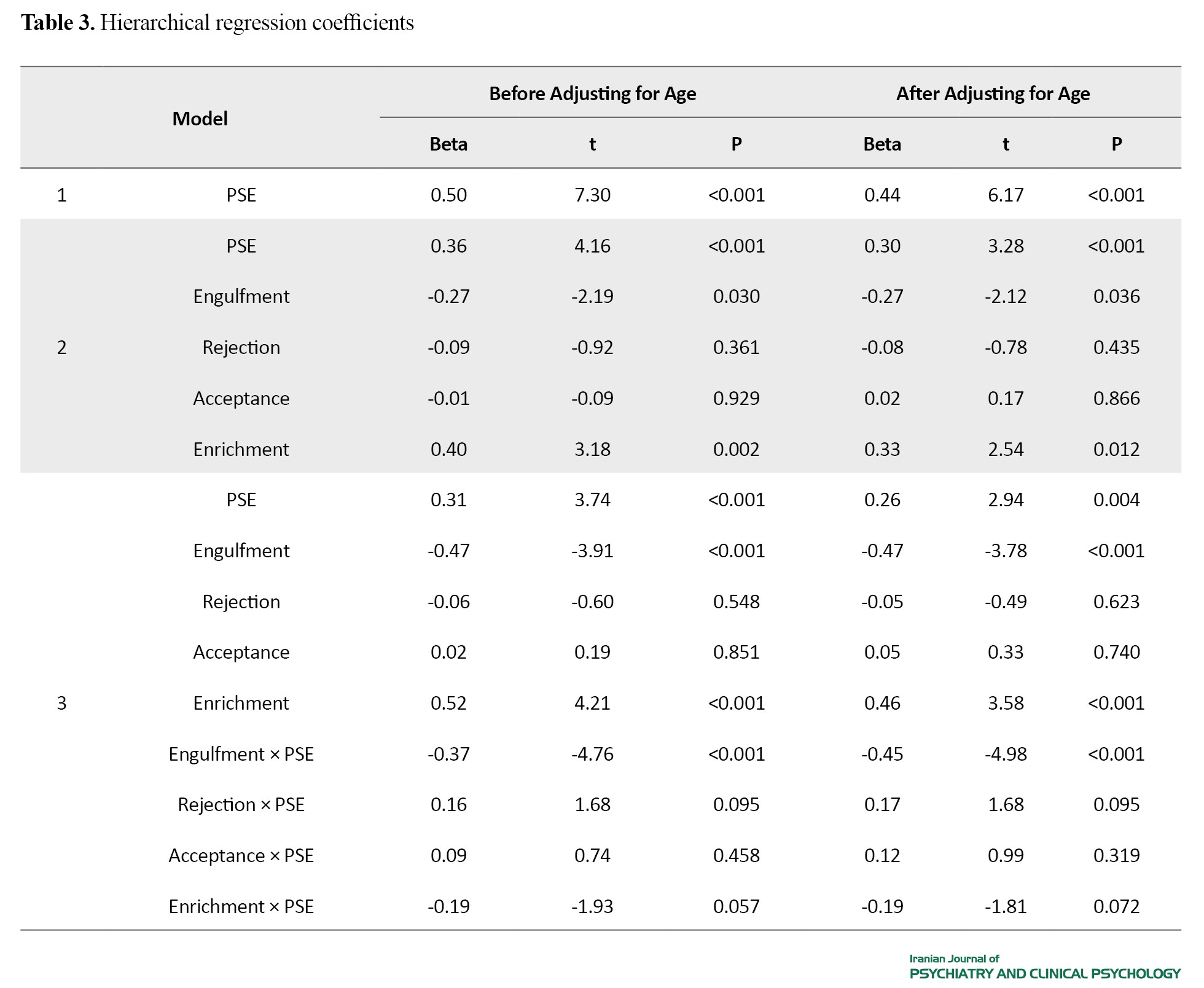
The regression coefficients are presented in Table 3. After adjusting for the effect of age on QoL, the explained variance attributed to PSE and enrichment decreased to 26% (P=0.004) and 46% (P<0.001), respectively. However, the adjustment did not change the beta value for the engulfment (P<0.001). The rejection and acceptance domains of the IIQ did not significantly explain the variance in QoL either before or after controlling for age (P>0.05). Furthermore, among the IIQ domains, only the engulfment domain significantly moderated the effect of PSE on QoL (P<0.001)
Conclusion
There is a positive relationship between PSE and QoL, and PSE predicts higher QoL. The illness identity type “engulfment” has a negative relationship with QoL, while “enrichment” is positively related to QoL. Moreover, the engulfment negatively moderates the relationship between PSE and QoL. This means that the engulfment of people with MS negatively affects how they perceive themselves, reducing the impact of self-efficacy beliefs on their QoL. This, in turn, leads to decreased engagement in social and occupational activities, ultimately resulting in a decline in QoL. Therefore, it is recommended to pay attention to the illness identity (especially engulfment and enrichment) and strengthen PSE in intervention programs for patients with MS to improve their QoL.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for the study was obtained from the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.653).
Funding
This study was funded by the Iran University of Medical Sciences.
Authors contributions
Conceptualization, Methodology, Software, Original Draft Preparation: Parisa Sharifi and Mojtaba Dehghan; Validation, Investigation, Review & Editing: Parisa Sharifi , Maede Amin Roaya, Mojtaba Dehghan ; Formal Analysis, Data Curation: Parisa Sharifi; Project Administration and Funding Acquisition: Mojtaba Dehghan.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the participants and the MS clinics at Asia and Sina hospitals for their cooperation in this study.
References
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system that leads to demyelination and neurodegeneration [3]. Due to its ambiguous, chronic, and life-altering nature, especially in the early stages, MS induces significant levels of distress in affected individuals [3]. This condition can reduce the quality of life (QoL) of patients [5]. The World Health Organization defines QoL as an individual’s perception of their position in life within the cultural and value systems in which they live, and in relation to their goals, expectations, standards, and concerns [6]. Living with a person suffering from MS can disrupt the QoL [7], and studying its antecedent factors is of great importance. Based on the social cognitive approach, the potential antecedents of QoL in individuals with MS may include their perceptions and beliefs about their disease, which can be the constructs such as pain self-efficacy (PSE) and illness identity. The PSE refers to an individual’s belief in their capacity to manage pain symptoms, minimize its impact on daily life, and maintain functionality despite pain [9, 10]. Pain is a common symptom of MS [11], and is experienced by more than 75% of MS people [12]. Examining the effects of PSE in people with MS is important. Illness identity is important in facing chronic illnesses. There are four illness identity types: Rejection, engulfment, acceptance, and enrichment. Their relationship with psychological and physical functioning in chronic physical conditions has been examined in previous studies [22]. Illness identity is a relatively new concept in health psychology and has been studied so far in cases such as people with cardiac disease [23, 24], multisystem connective tissue disorders [23], and epilepsy [25].
The literature review indicates that the experience of MS affects individuals’ beliefs and perceptions about themselves. Understanding the extent to which PSE and each of the four illness identity types explain QoL among people with MS can help health psychologists in designing interventions aimed at improving QoL. However, there is a research gap in this area. Therefore, this study aimed to examine the relationship of PSE and illness identity with QoL among individuals with MS and to assess the moderating role of illness identity in the relationship between PSE and QoL.
Methods
This is a correlational study with a cross-sectional design. The study population included all individuals with MS referred to Sina and Asia hospitals in Tehran, Iran, from November 16, 2023 to June 20, 2024. Using G*Power software (effect size=0.15, α=0.05, test power=0.95), the sample size was estimated at 138, but finally 166 participants were included in the study. Inclusion criteria were the MS diagnosis and age 18-60 years. Exclusion criteria were a prior psychiatric diagnosis before MS and diagnosis of comorbid chronic diseases (based on the patient’s medical records).
For data collection, a demographic form (surveying age, gender, educational level, marital status, duration of illness, and type of MS), the Persian version of the World Health Organization Quality of Life Questionnaire- Brief version [26], the Persian version of the Pain Self-Efficacy Questionnaire [27], and the Persian version of the Illness Identity Questionnaire (IIQ) [22] were employed.
Six participants were excluded during data collection due to outlier data, resulting in a final sample size of 160. Pearson’s correlation test and hierarchical regression analysis (with and without adjusting for age) were utilized for data analysis. Additionally, independent t-test was used to compare the mean QoL based on gender, and a one-way ANOVA was conducted to compare the mean QoL based on other demographic variables.
Results
The mean age of participants was 37.16±8.63 years, ranged 18-57 years. They included 107 females and 51 males. Additionally, 42 had a high school diploma or lower education, 82 had an associate/bachelor’s degree, and 32 had a master’s/doctoral degree. Regarding marital status, 49 were single, 97 were married, and 12 were divorced. Concerning the MS types, 63 had relapsing-remitting MS (RRMS), 67 primary progressive MS (PPMS), and 28 secondary progressive MS (SPMS). In terms of illness duration, 44 had been diagnosed for less than 2 years, 26 for 2-5 years, 43 for 5-10 years, and 45 for >10 years. Descriptive statistics for each variable, as well as the correlation coefficients are reported in Table 1.
Given the significant correlation between age and QoL, two hierarchical regressions were conducted to assess the role of independent and moderating variables in predicting QoL (with and without adjusting for the effect of age on QoL). Each hierarchical regression was conducted in three steps (or models). In the first step, PSE was entered into the equation. In the second step, the four types of illness identity were added. In the third step, four new variables (interaction of PSE with the illness identity types)were included in the model (Tables 2 and 3).
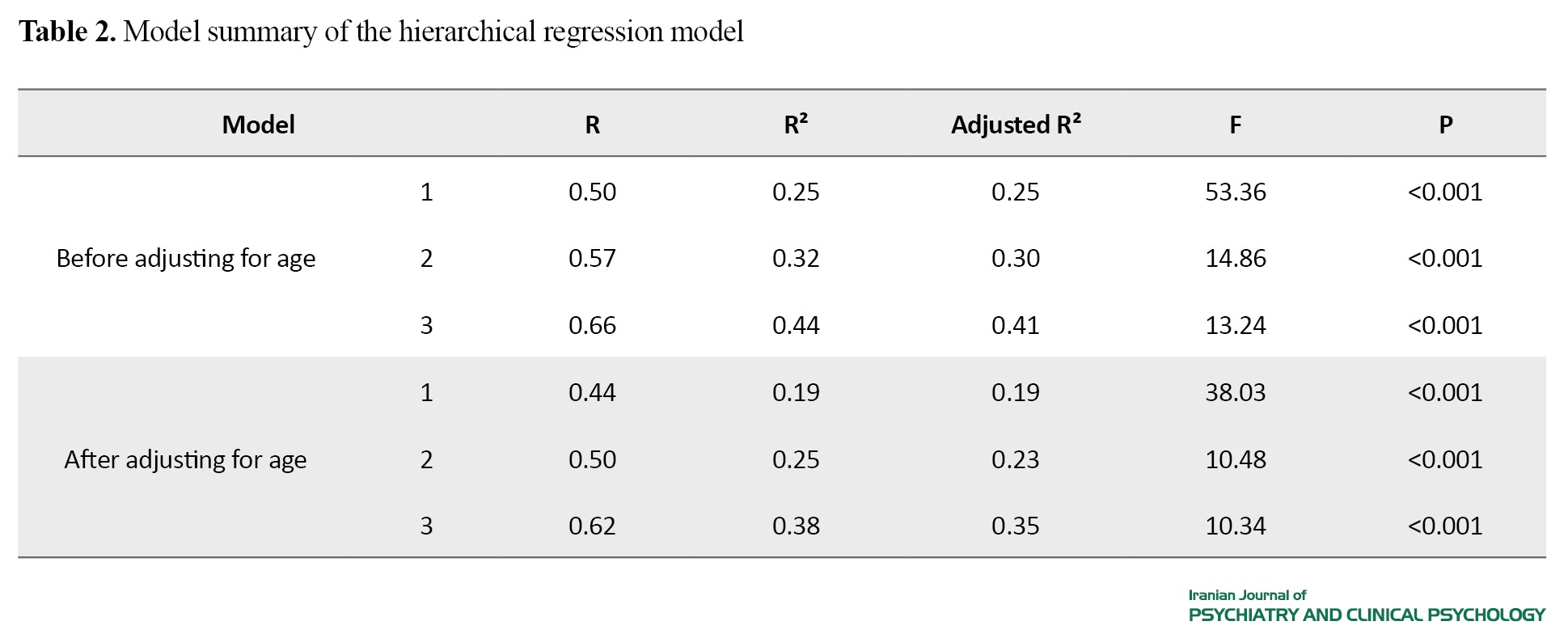
According to the results in Table 2, the third study model explained 44% of the variance in QoL before adjusting for age. However, this decreased to 38% after adjusting for age. Nevertheless, this model retained significant power in explaining the variance of QoL, even after adjusting for the effect of age.
The regression coefficients are presented in Table 3. After adjusting for the effect of age on QoL, the explained variance attributed to PSE and enrichment decreased to 26% (P=0.004) and 46% (P<0.001), respectively. However, the adjustment did not change the beta value for the engulfment (P<0.001). The rejection and acceptance domains of the IIQ did not significantly explain the variance in QoL either before or after controlling for age (P>0.05). Furthermore, among the IIQ domains, only the engulfment domain significantly moderated the effect of PSE on QoL (P<0.001)
Conclusion
There is a positive relationship between PSE and QoL, and PSE predicts higher QoL. The illness identity type “engulfment” has a negative relationship with QoL, while “enrichment” is positively related to QoL. Moreover, the engulfment negatively moderates the relationship between PSE and QoL. This means that the engulfment of people with MS negatively affects how they perceive themselves, reducing the impact of self-efficacy beliefs on their QoL. This, in turn, leads to decreased engagement in social and occupational activities, ultimately resulting in a decline in QoL. Therefore, it is recommended to pay attention to the illness identity (especially engulfment and enrichment) and strengthen PSE in intervention programs for patients with MS to improve their QoL.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for the study was obtained from the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.653).
Funding
This study was funded by the Iran University of Medical Sciences.
Authors contributions
Conceptualization, Methodology, Software, Original Draft Preparation: Parisa Sharifi and Mojtaba Dehghan; Validation, Investigation, Review & Editing: Parisa Sharifi , Maede Amin Roaya, Mojtaba Dehghan ; Formal Analysis, Data Curation: Parisa Sharifi; Project Administration and Funding Acquisition: Mojtaba Dehghan.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the participants and the MS clinics at Asia and Sina hospitals for their cooperation in this study.
References
- Prakash RS, Schirda B, Valentine TR, Crotty M, Nicholas JA. Emotion dysregulation in multiple sclerosis: Impact on symptoms of depression and anxiety. Multiple Sclerosis and Related Disorders. 2019; 36:101399. [DOI:10.1016/j.msard.2019.101399] [PMID]
- Ysrraelit MC, Fiol MP, Gaitán MI, Correale J. Quality of life assessment in multiple sclerosis: Different perception between patients and neurologists. Frontiers in Neurology. 2018; 8:729. [DOI:10.3389/fneur.2017.00729] [PMID]
- Janssens AC, van Doorn PA, de Boer JB, Kalkers NF, van der Meche FG, Passchier J, et al. Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Multiple Sclerosis. 2003; 9(4):397-403. [DOI:10.1191/1352458-503ms930oa] [PMID]
- Confavreux C, Vukusic S, Moreau T, Adeleine P. Relapses and progression of disability in multiple sclerosis. New England Journal of Medicine. 2000; 343(20):1430-8. [DOI:10.1056/NEJM200011163432001] [PMID]
- Arnett PA. Neuropsychological presentation and treatment of demyelinating disorders. In: Halligan UKP, Marshall J, editors. Handbook of Clinical Neuropsychology. Oxford: Oxford University Press; 2003. [DOI:10.1093/acprof:oso/9780199234110.0¬03.029]
- WHOQoL Group. Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQoL). Quality of Life Research. 1993; 2:153-9. [DOI:10.1007/BF00435734]
- Mohammad K, Rimaz S, Dastoorpour M, Sadeghi M, Majdzadeh SR. [Quality of life and related factors among multiple sclerosis patients (Persian)] .Journal of School of Public Health and Institute of Public Health Research. 2014; 11(4):1-14. [Link]
- Young CA, Mills R, Langdon D, Sharrack B, Majeed T, Kalra S, et al. The four self-efficacy trajectories among people with multiple sclerosis: Clinical associations and implications. Journal of Neurological Sciences. 2022; 436:120188. [DOI:10.1016/j.jns.2022.120188] [PMID]
- Anderson KO, Dowds BN, Pelletz RE, Edwards WT, Peeters-Asdourian C. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain. 1995; 63:77-84. [DOI:10.1016/0304-3959(95)00021-J] [PMID]
- Nicholas MK. The pain self-efficacy questionnaire: Taking pain into account. European Journal of Pain. 2007; 11:153-63. [DOI:10.1016/j.ejpain.2005.12.008] [PMID]
- Brownlee WJ, Hardy TA, Fazekas F, Miller DH. Diagnosis of multiple sclerosis: Progress and challenges. Lancet. 2017; 389(10076):1336-46. [DOI:10.1016/S0140-6736(16)30959-X] [PMID]
- Solaro C, Trabucco E, Messmer Uccelli M. Pain and multiple sclerosis: Pathophysiology and treatment. Current Neurology and Neuroscience Reports. 2013; 13(1):320. [DOI:10.1007/s11910-012-0320-5] [PMID]
- Costa LDCM, Maher CG, McAuley JH, Hancock MJ, Smeets RJEM. Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. European Journal of Pain. 2011; 15:213-9. [DOI:10.1016/j.ejpain.2010.06.014] [PMID]
- Somers TJ, Kurakula PC, Criscione-Schreiber L, Keefe FJ, Clowse ME. Self-efficacy and pain catastrophizing in systemic lupus erythematosus: Relationship to pain, stiffness, fatigue, and psychological distress. Arthritis Care & Research. 2012; 64:1334-40. [DOI:10.1002/acr.21686] [PMID]
- Sikes EM, Cederberg KL, Baird JF, Sandroff BM, Motl RW. Self-efficacy and walking performance across the lifespan among adults with multiple sclerosis. Neurodegenerative Disease Management. 2019; 9(5):267-75. [DOI:10.2217/nmt-2019-0007] [PMID]
- Dehghan M, Sharifi P, Hasani J, Young CA, Langdon D. Healthier living with MS: The key role of self-efficacy and emotion regulation. Multiple Sclerosis and Related Disorders. 2023; 7(73):104608. [DOI:10.1016/j.msard.2023.104608] [PMID]
- Young CA, Mills R, Rog D, Sharrack B, Majeed T, Constantinescu CS, et al. Quality of life in multiple sclerosis is dominated by fatigue, disability and self-efficacy. Journal of the Neurological Sciences. 2021; 426:117437. [DOI:10.1016/j.jns.2021.117437] [PMID]
- Motl RW, McAuley E, Snook EM, Gliottoni RC. Physical activity and quality of life in multiple sclerosis: Intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychology, Health & Medicine. 2009; 14(1):111-24. [DOI:10.1080/13¬548500802241902] [PMID]
- Charmaz K. The body, identity, and self. The Sociological Quarterly. 1995; 36:657-80. [DOI:10.1111/j.1533-8525.1995.tb00459.x]
- Charmaz K. Theorizing chronic illness: A life course perspective. In: Halfon N, Forrest CB, Lerner RM, Faustman EM, editors.Handbook of life course health development. Berlin: Springer; 2018. [Link]
- Charmaz K. Identity dilemmas of chronically Ill men. The Sociological Quarterly. 1994; 35(2):269–88. [Link]
- Oris L, Rassart J, Prikken S, Verschueren M, Goubert L, Moons P, et al. Illness identity in adolescents and emerging adults with type 1 diabetes: Introducing the Illness Identity Questionnaire. Diabetes Care. 2016; 39(5):757-63. [DOI:10.2337/dc15-2559] [PMID]
- Oris L, Luyckx K, Rassart J, Goubert L, Goossens E, Apers S, et al. Illness identity in adults with a chronic illness. Journal of Clinical Psychology in Medical Settings. 2018; 25(4):429-40. [DOI:10.1007/s10880-018-9552-0] [PMID]
- Van Bulck L, Goossens E, Luyckx K, Oris L, Apers S, Moons P. Illness identity: A novel predictor for healthcare use in adults with congenital heart disease. Journal of the American Heart Association. 2018; 7(11):e008723. [DOI:10.1161/jaha.118.008723] [PMID]
- Luyckx K, Oris L, Raymaekers K, Rassart J, Moons P, Verdyck L, et al. Illness identity in young adults with refractory epilepsy. Epilepsy & Behavior. 2018; 80:48-55. [DOI:10.1016/j.yebeh.2017.12.036] [PMID]
- Nejat S, Montazeri A, Holakouie Naieni K, Mohammad K, Majdzadeh S. [The World Health Organization quality of life (WHOQoL-BREF) Questionnaire: Translation and validation study of the Iranian version (Persian)]. Journal of School of Public Health and Institute of Public Health Research. 2006; 4(4):1-12. [Link]
- Asghari A, Nicholas MK. An investigation of pain self-efficacy beliefs in Iranian chronic pain patients: A preliminary validation of a translated English-language scale. Pain Medicine. 2009; 10:619-32. [DOI:10.1111/j.1526-4637.2009.00623.x] [PMID]
- Kaivanto KK, Estlander AM, Moneta GB, Vanharanta H. Isokinetic performance in low back pain patients: The predictive power of the Self-Efficacy Scale. Journal of Occupational Rehabilitation. 1995; 5(2):87-99. [DOI:10.1007/BF02109912] [PMID]
- George D, Mallery P. SPSS for Windows Step by Step: A simple guide and reference, 17.0 update. Boston: Pearson; 2010. [Link]
- Karasawa M, Shibata M, Nakagawa A. Pain self-efficacy and quality of life in chronic pain conditions. Pain Medicine. 2019; 20(4):712-20. [DOI:10.1016/j.pain.2019.01.014]
- Yazdi-Ravandi S, Taslimi Z, Jamshidian N, Saberi H, Shams J, Haghparast A. Prediction of quality of life by self-efficacy, pain intensity and pain duration in patient with pain disorders. Basic and Clinical Neuroscience. 2013; 4(2):117-24. [PMID]
- Pakenham KI. Illness identity and quality of life in multiple sclerosis. Journal of Health Psychology. 2007; 12(3):355-68. [DOI:10.1080/13548500500465878] [PMID]
- Shneider CE, Robbertz AS, Cohen LL. A systematic review of relationships between illness identity and health-related outcomes in individuals with chronic illnesses.Journal of Clinical Psychology in Medical Settings. 2024; 31(1):130-42. [DOI:10.1007/s10880-023-09973-1] [PMID]
- Van Bulck L, Luyckx K, Goossens E, Oris L, Moons P. Illness identity: Capturing the influence of illness on the person’s sense of self. European Journal of Cardiovascular Nursing. 2019; 18(1):4–6. [DOI:10.1177/1474515118811960] [PMID]
- Rostami H, Nuri E, Sharghi E. Effect of cognitive-behavioral stress management therapy on pain perception, chronic fatigue and cognitive empowerment of women with fibromyalgia syndrome: A randomized clinical trial. Iranian Journal of Psychiatry and Clinical Psychology. 2024; 30(1):4819.1 [DOI:10.32598/ijpcp.30.4819.1]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/08/9 | Accepted: 2024/11/30 | Published: 2024/07/31
Received: 2024/08/9 | Accepted: 2024/11/30 | Published: 2024/07/31
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |