Sun, Feb 15, 2026
| فارسی
Volume 30, Issue 1 (Continuously Updated 2024)
IJPCP 2024, 30(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Taghinejad H, Otaghi M, Raiesifar A, Sayeh Miri K, Sahami Gilan M. Effects of a Cognitive Behavioral Therapy Program on Sleep Quality and General Health of Older Men Living in Nursing Homes: A Randomized Clinical Trial. IJPCP 2024; 30 (1) : 5070.1
URL: http://ijpcp.iums.ac.ir/article-1-4228-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4228-en.html
Hamid Taghinejad1 
 , Masoumeh Otaghi1
, Masoumeh Otaghi1 
 , Afsaneh Raiesifar1
, Afsaneh Raiesifar1 
 , Kourosh Sayeh Miri2
, Kourosh Sayeh Miri2 
 , MohammadHossein Sahami Gilan3
, MohammadHossein Sahami Gilan3 


 , Masoumeh Otaghi1
, Masoumeh Otaghi1 
 , Afsaneh Raiesifar1
, Afsaneh Raiesifar1 
 , Kourosh Sayeh Miri2
, Kourosh Sayeh Miri2 
 , MohammadHossein Sahami Gilan3
, MohammadHossein Sahami Gilan3 

1- Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
2- Department of Biostatistics, School of Health Psychosocial Injuries Research Center, Ilam University of Medical Sciences, Ilam, Iran.
3- Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran. ,sahami3621@gmail.com
2- Department of Biostatistics, School of Health Psychosocial Injuries Research Center, Ilam University of Medical Sciences, Ilam, Iran.
3- Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran. ,
Full-Text [PDF 8293 kb]
(527 Downloads)
| Abstract (HTML) (1147 Views)
Full-Text: (924 Views)
Introduction
One of the problems in old age is the decrease in the quality and quantity of sleep, which can affect the body and mind, quality of life, and daily activities of older adults and is closely related to mental health problems, including anxiety and anxiety. It can also cause a decline in executive function and memory, an increase in the risk of falls, and a disruption in strategic planning ability. Another problem in old age is the occurrence of psychological disorders. It is the second cause of losing disability-adjusted life years after traffic accidents. One of the non-pharmacological methods for the treatment of various sleep disorders in older adults and is used due to its simplicity and high effectiveness is cognitive behavioral therapy (CBT). This method increases and improves the sleep environment, reduces negative actions and thoughts that can disturb the quality of sleep, and creates a regular sleep schedule. Keeping this in mind, this study aims to determine the effectiveness of a CBT-based educational program on sleep quality and general health of older men living in nursing homes.
Methods
This is a double-blind controlled clinical trial with a pre-test/post-test/one-month follow-up design. The study population consists of all older men aged >65 years living in a nursing home in Kermanshah, Iran (n=85), of whom 68 were selected based on the inclusion criteria and were randomly divided into two groups of intervention (n=34) and control (n=34). The intervention group received a CBT-based educational program for 8 weeks at eight sessions of 45 minutes (one session per week). During this period, the control group did not receive any special treatment except daily routine care and verbal communication. At the end of the intervention, educational content was provided to them in a single session. The data were collected before, immediately after, and one month after the intervention using the Pittsburgh sleep quality index (PSQI) and Goldberg’s general health questionnaire (GHQ-28), where higher scores indicate higher sleep disturbances and distress. Finally, the data were analyzed using descriptive (mean, frequency, percentage, and standard deviation) and inferential (Kolmogorov-Smirnov, paired t-test, independent t-test, and repeated measures ANOVA) statistics in SPSS software, version 16.
Results
The mean age of the participants was 71.55±5.24 years. Most of the participants were married with primary school education and no children, and their previous job status was retired employees. Using the chi-square test, no significant difference in any demographic variables was found between the two groups (P>0.05). Tables 1, 2 and 3 show the mean scores of PSQI and GHQ-28 for the intervention and control groups in the three stages of pre-test, post-test, and follow-up.
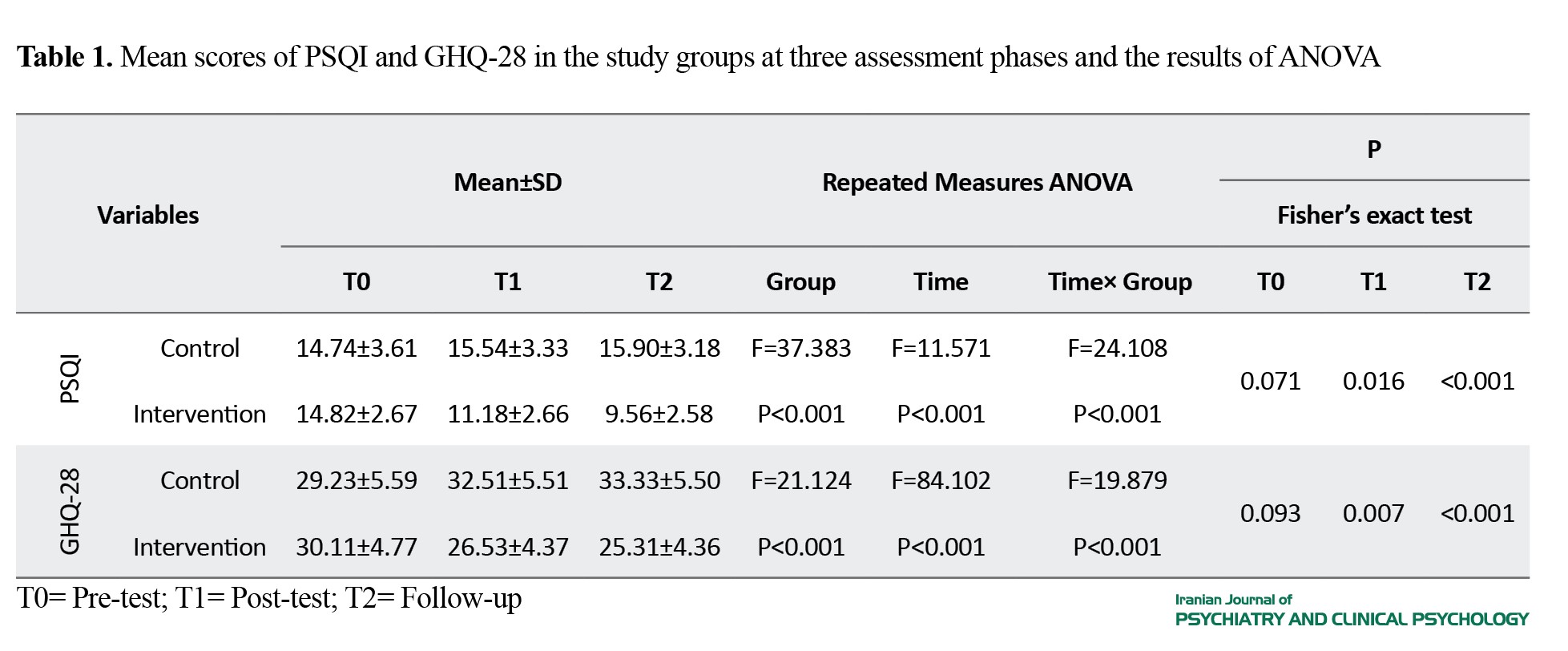
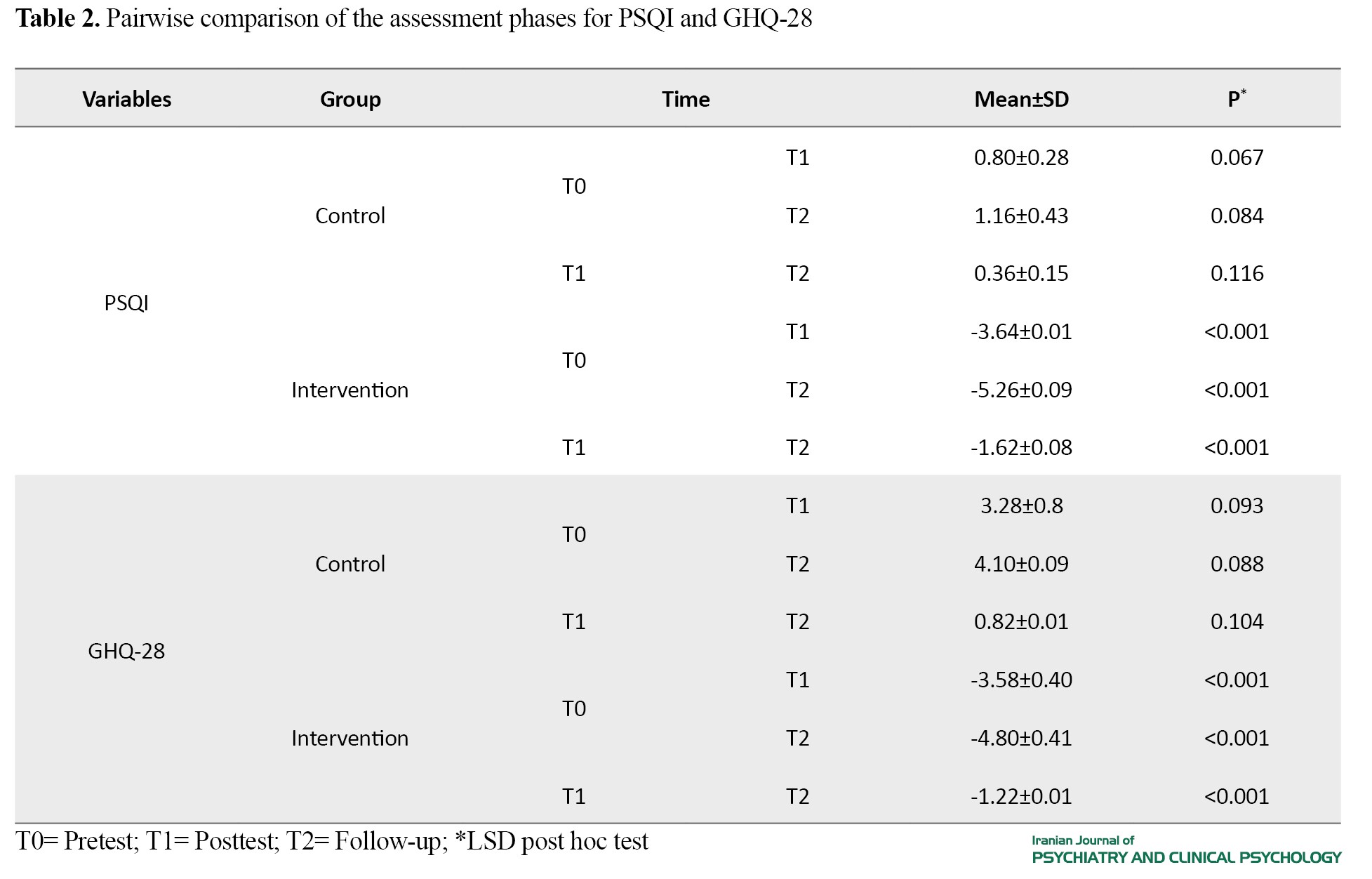
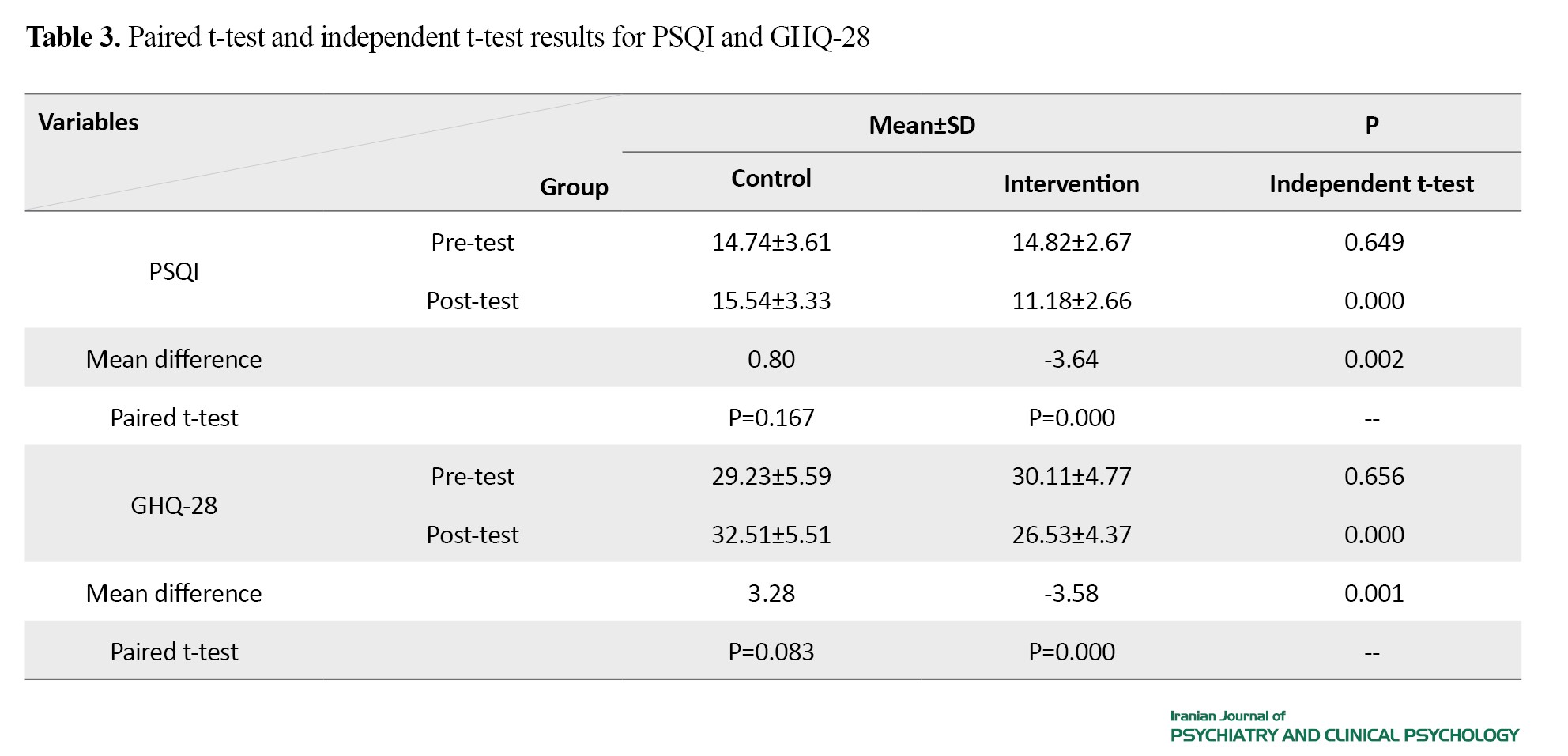
The results showed a significant difference in the mean scores of PSQI and GHQ-28 and their domains between the two groups. Their scores decreased significantly in the posttest and follow-up phases compared to the pretest phase in the intervention group, which shows the positive and significant effect of the educational program.
Conclusions
The CBT-based educational program can improve the sleep quality and general health of older men living in nursing homes.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the Ethics Committee of Ilam University of Medical Sciences (Code: IR.MEDILAM.REC.1402.213) and was registered by the Iranian Registry of Clinical Trials (ID: IRCT20230808059089N1). All participants declared their written informed consent. They were assured of the confidentiality of their information and were free to leave the study at any time.
Funding
This article was extracted from a master’s thesis in geriatric nursing at Ilam University of Medical Sciences. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors contributions
Conceptualization: Hamid Taghinejad and Masoumeh Otaghi; methodology: Hamid Taghinejad, Masoumeh Otaghi, and Mohammad Hossein Sahami Gilan; Investigation and original draft preparation: Hamid Taghinejad and Afsaneh Raiesifar; Resources: Kourosh Sayeh Miri; Review and editing: Masoumeh Otaghi and Afsaneh Raiesifar; Visualization, supervision, and funding acquisition: Mohammad Hossein Sahami Gilan.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the Welfare Organization and the nursing homes in Kermanshah, and all seniors who participated in this research for their cooperation.
References
One of the problems in old age is the decrease in the quality and quantity of sleep, which can affect the body and mind, quality of life, and daily activities of older adults and is closely related to mental health problems, including anxiety and anxiety. It can also cause a decline in executive function and memory, an increase in the risk of falls, and a disruption in strategic planning ability. Another problem in old age is the occurrence of psychological disorders. It is the second cause of losing disability-adjusted life years after traffic accidents. One of the non-pharmacological methods for the treatment of various sleep disorders in older adults and is used due to its simplicity and high effectiveness is cognitive behavioral therapy (CBT). This method increases and improves the sleep environment, reduces negative actions and thoughts that can disturb the quality of sleep, and creates a regular sleep schedule. Keeping this in mind, this study aims to determine the effectiveness of a CBT-based educational program on sleep quality and general health of older men living in nursing homes.
Methods
This is a double-blind controlled clinical trial with a pre-test/post-test/one-month follow-up design. The study population consists of all older men aged >65 years living in a nursing home in Kermanshah, Iran (n=85), of whom 68 were selected based on the inclusion criteria and were randomly divided into two groups of intervention (n=34) and control (n=34). The intervention group received a CBT-based educational program for 8 weeks at eight sessions of 45 minutes (one session per week). During this period, the control group did not receive any special treatment except daily routine care and verbal communication. At the end of the intervention, educational content was provided to them in a single session. The data were collected before, immediately after, and one month after the intervention using the Pittsburgh sleep quality index (PSQI) and Goldberg’s general health questionnaire (GHQ-28), where higher scores indicate higher sleep disturbances and distress. Finally, the data were analyzed using descriptive (mean, frequency, percentage, and standard deviation) and inferential (Kolmogorov-Smirnov, paired t-test, independent t-test, and repeated measures ANOVA) statistics in SPSS software, version 16.
Results
The mean age of the participants was 71.55±5.24 years. Most of the participants were married with primary school education and no children, and their previous job status was retired employees. Using the chi-square test, no significant difference in any demographic variables was found between the two groups (P>0.05). Tables 1, 2 and 3 show the mean scores of PSQI and GHQ-28 for the intervention and control groups in the three stages of pre-test, post-test, and follow-up.
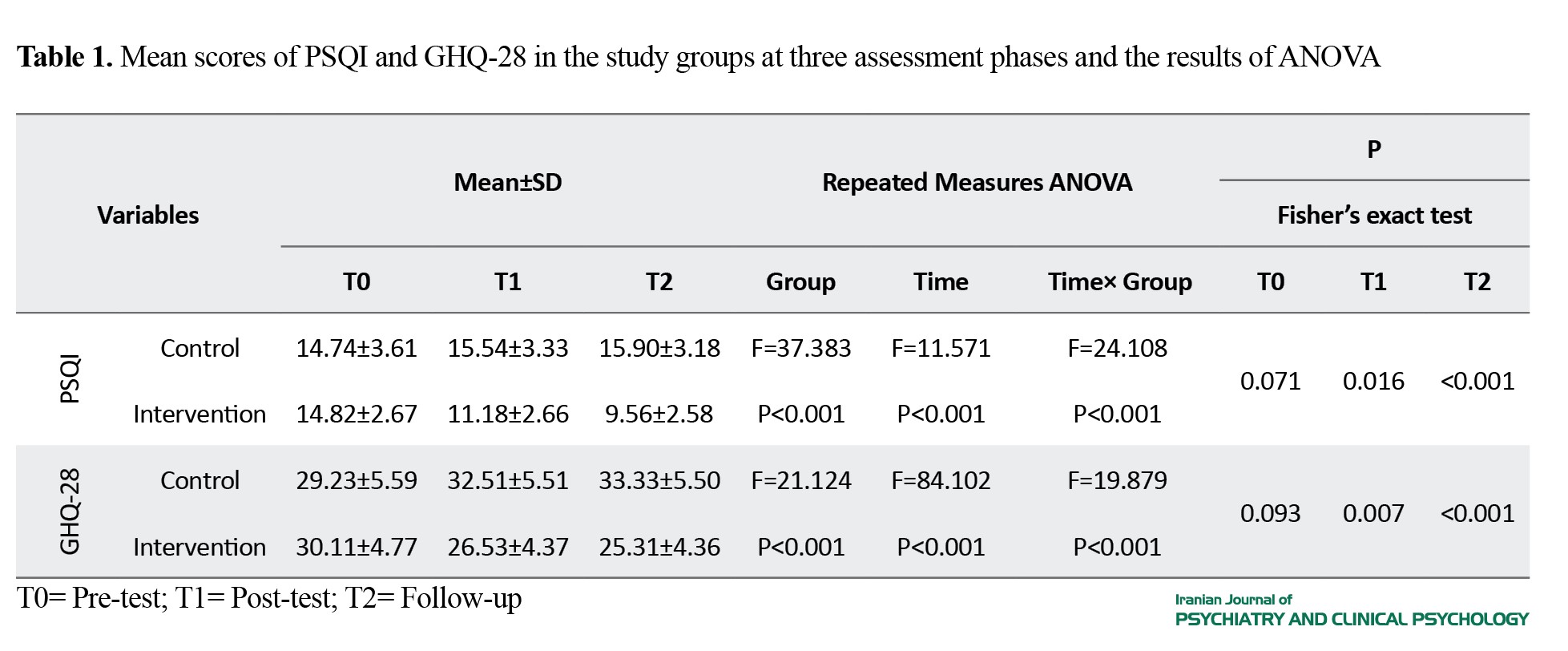
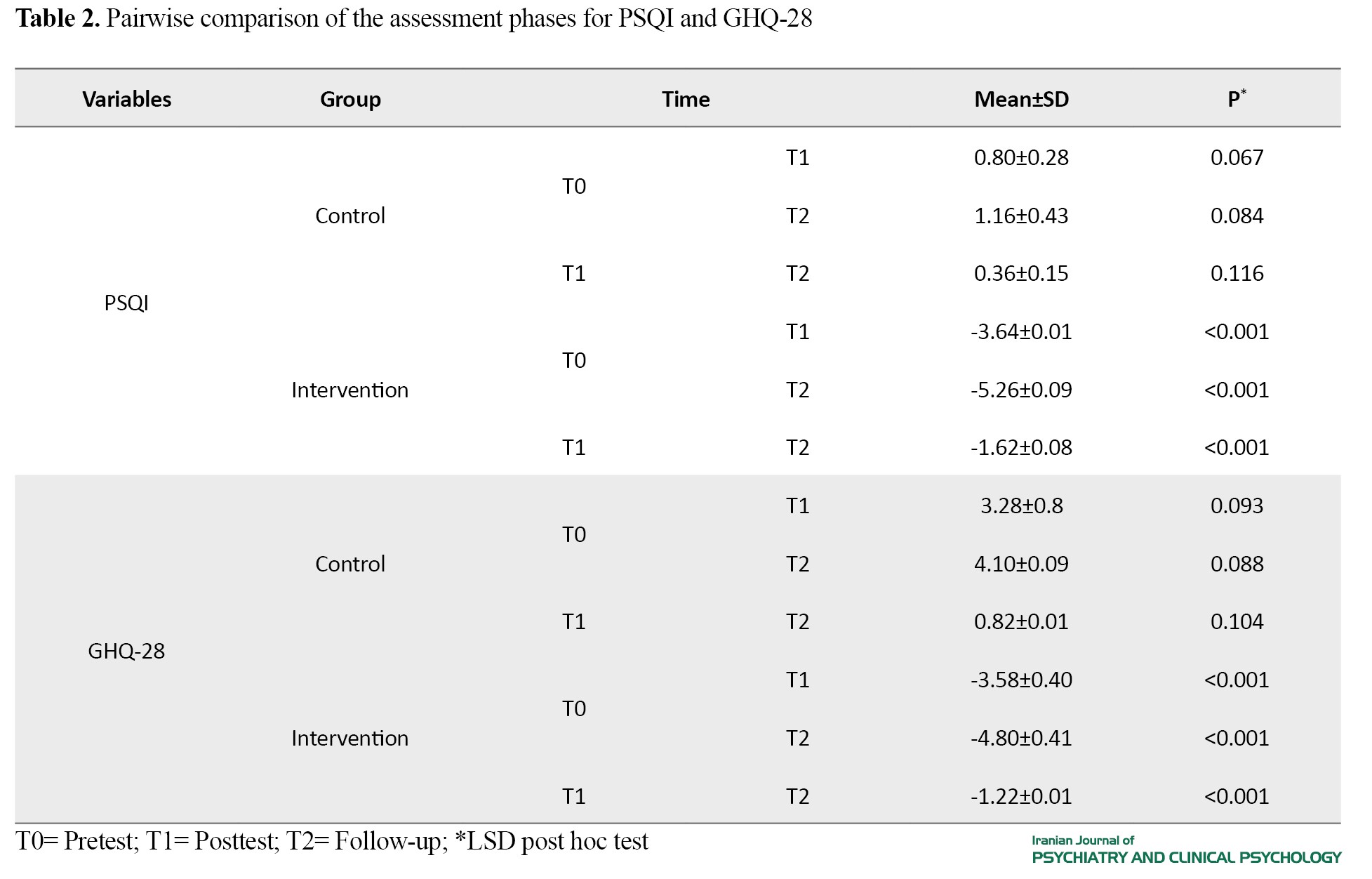
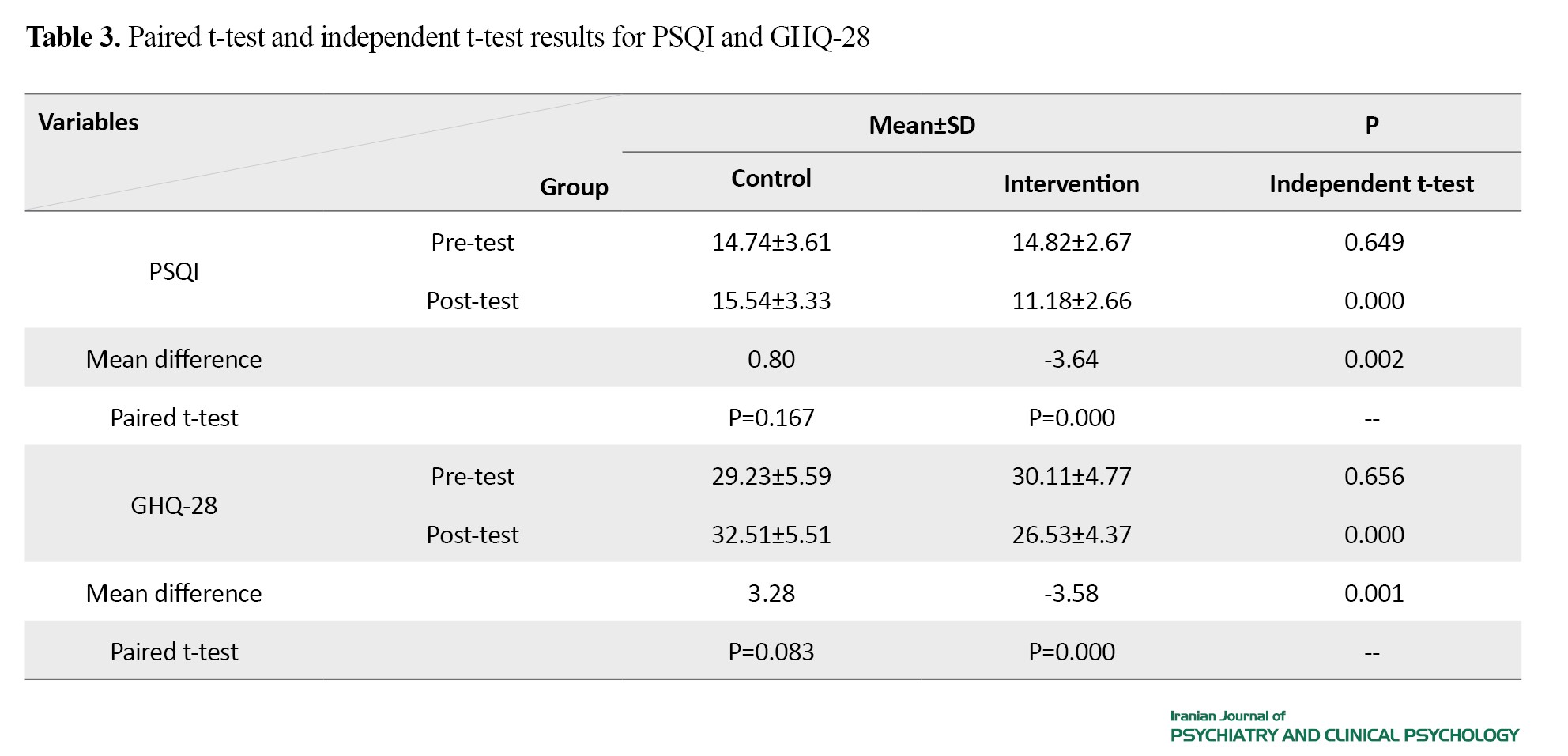
The results showed a significant difference in the mean scores of PSQI and GHQ-28 and their domains between the two groups. Their scores decreased significantly in the posttest and follow-up phases compared to the pretest phase in the intervention group, which shows the positive and significant effect of the educational program.
Conclusions
The CBT-based educational program can improve the sleep quality and general health of older men living in nursing homes.
Ethical Considerations
Compliance with ethical guidelines
This research was approved by the Ethics Committee of Ilam University of Medical Sciences (Code: IR.MEDILAM.REC.1402.213) and was registered by the Iranian Registry of Clinical Trials (ID: IRCT20230808059089N1). All participants declared their written informed consent. They were assured of the confidentiality of their information and were free to leave the study at any time.
Funding
This article was extracted from a master’s thesis in geriatric nursing at Ilam University of Medical Sciences. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors contributions
Conceptualization: Hamid Taghinejad and Masoumeh Otaghi; methodology: Hamid Taghinejad, Masoumeh Otaghi, and Mohammad Hossein Sahami Gilan; Investigation and original draft preparation: Hamid Taghinejad and Afsaneh Raiesifar; Resources: Kourosh Sayeh Miri; Review and editing: Masoumeh Otaghi and Afsaneh Raiesifar; Visualization, supervision, and funding acquisition: Mohammad Hossein Sahami Gilan.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the Welfare Organization and the nursing homes in Kermanshah, and all seniors who participated in this research for their cooperation.
References
- Khami L, Motalebi SA, Mohammadi F, Momeni M, Shahrokhi A. Can social support predict health promoting behaviors among community dwelling older adults? Social Health and Behavior. 2020; 3(1):22. [DOI:10.4103/SHB.SHB_50_19]
- Beard JR, Officer A, De Carvalho IA, Sadana R, Pot AM, Michel J P, et al. The World report on ageing and health: a policy framework for healthy ageing. The Lancet. 2016; 387(10033):2145 54. [DOI:10.1016/S0140-6736(15)00516-4] [PMID]
- Mottaghi R, Maredpour AR, Kharamin S. The effectiveness of sleep health education on sleep quality, blood pressure, heart rate and oxygen saturation in blood of the elderly with insomnia. Aging Psychology. 2021; 7(3):282 69.
- Machado AM, Vilaça M, Patrão AL, Pereira MG. Predictors and Moderators of Quality of Life in Male Users of Anti Aging Products. PsyCh Journal. 2023; 12(1):73-83. [DOI:10.1002/pchj.609] [PMID]
- Isfahani P, Afshin M, Mohammadi F, Arefnezhad M. [Prevalence of depression among Iranian elderly: A Systematic review and Meta-analysis (Persian). Journal of Gerontology. 2021; 5(3):66-77. [Link]
- Ghasemyani S, Jafari M, Teymourlouy AA, Fadayevatan R. Components of elderly long term care system in Iran and selected countries: A comparative study. Health Scope. 2021; 10(3). [DOI:10.5812/jhealthscope.109140]
- Novrouzi R, Ghaffari M, Sabouri M, Marashi T, Rakhshanderou S. Investigating the Effect of Self care on the Nutritional Status of the Elderly by Structural Equation Modeling Analysis. Yektaweb_Journals. 2023; 18(1):46 59. [DOI:10.32598/sija.2022.3368.1]
- Bagi M, Abbasi Shawazi MJ. Greater burden of responsibility in old age: investigation of trends and patterns of living arrangements of the elderly in Iran. Welfare Planning and Social Development. 2021; 13(47):135 66.
- Bagi M, Abbasi Shavazi MJ. More responsibilities at the older ages: the study of trends and patterns of elderly living arrangements in Iran. Social Development & Welfare Planning. 2021; 12(47):135 66.
- Corbo I, Forte G, Favieri F, Casagrande M. Poor Sleep Quality in Aging: The Association with Mental Health. International Journal of Environmental Research and Public Health. 2023; 20(3):1661. [DOI:10.3390/ijerph20031661] [PMID]
- Haryati MC, Kusumaningsih I, Supardi S. Factors related to sleep quality of elderly people in RW 03 Kelurahan Kebon Manggis Jakarta. Jurnal Keperawatan Malang. 2022; 7(2):190-205. [DOI:10.36916/jkm.v7i2.177]
- Taherpour M, Mirzaei Alavijeh M, Khazaie H, Hosseini SN, Fatahi M, Karimi N, et al. Socio cognitive Determinants of Healthy Sleep Behaviors Among Iranian Elderly: Application of the Theory of Planned Behavior. Journal of Education and Community Health. 2022; 9(2):80 5. [DOI:10.34172/jech.2022.12]
- Ling J, Sun W, Chan NY, Zhang J, Lam SP, Li AM, et al. Effects of insomnia symptoms and objective short sleep duration on memory performance in youths. Journal of Sleep Research. 2020; 29(4):e13049. [DOI:10.1111/jsr.13049] [PMID]
- Azimi M, Moradi A, Hasani J. Effectiveness of cognitive behavioral therapy for insomnia (traditional and Internet-based) on everyday memory of people with insomnia and comorbid depression. Advances in Cognitive Science. 2019; 20(4):20–34. [Link]
- Van As BAL, Imbimbo E, Franceschi A, Menesini E, Nocentini A. The longitudinal association between loneliness and depressive symptoms in the elderly: A systematic review. International Psychogeriatrics. 2022; 34(7):657-69. [Link]
- Sasanipour M. Provincial Differences in the Main Causes of Years of Life Lost Due to Premature Death of Iranian Elderly in 2016. Qom University of Medical Sciences Journal. 2022; 15(10):708 17. [DOI:10.32598/qums.15.10.2503.1]
- Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta analysis. Sleep Medicine Reviews. 2019; 43:96 105. [DOI:10.1016/j.smrv.2018.10.006] [PMID]
- Scott AJ, Webb TL, Martyn St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta analysis of randomised controlled trials. Sleep Medicine Reviews. 2021; 60:101556. [DOI:10.1016/j.smrv.2021.101556] [PMID]
- Sterina E, Hermida AP, Gerberi DJ, Lapid MI. Emotional resilience of older adults during COVID 19: A systematic review of studies of stress and well being. Clinical Gerontologist. 2022; 45(1):4 19. [DOI:10.1080/07317115.2021.1928355] [PMID]
- Hashemi Z, Afshari A, Einy S. The effectiveness of acceptance and commitment education on improving the mental health and quality of life of elderly people with cancer. Iranian Journal of Health Education and Health Promotion. 2020; 8(2):160-71. [DOI:10.29252/ijhehp.8.2.160]
- Amini A, Shirvani H, Bazgir B. [Comparison of sleep quality in active and non active military retirement and its relationship with mental health (Persian)]. Journal of Military Medicine. 2020; 22(3):252-63. [Link]
- Silva Perez LJ, Gonzalez Cardenas N, Surani S, Sosso FE, Surani SR, Surani S. Socioeconomic status in pregnant women and sleep quality during pregnancy. Cureus. 2019; 11(11). [DOI:10.7759/cureus.6183] [PMID]
- João KADR, de Jesus SN, Carmo C, Pinto P. The impact of sleep quality on the mental health of a non clinical population. Sleep Medicine. 2018; 46:69 73. [DOI:10.1016/j.sleep.2018.02.010] [PMID]
- Ghobadimehr A, Pasha H, Hosseini SR, Bijani A. Relationship between sleep quality and falls among elderly people in Amirkola, Northern of Iran. Journal of Education and Community Health. 2022; 9(2):94-100. [DOI:10.34172/jech.2022.14]
- Taheri Tanjani P, Khodabakhshi H, Etemad K, Mohammadi M. Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016. Iranian Journal of Ageing. 2019; 14(2):248 59.
- de C Williams AC, Fisher E, Hearn L, Eccleston C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews. 2020; 8(8):CD007407. [DOI:10.1002/14651858.CD007407.pub4] [PMID]
- Yazdani M, Hosseini SF, Gilvari T, Khajehmirzaei F, Mazruee R, Akhoundzadeh G. The effect of continuous care model on maternal perception of infant sleep in Bint Al Huda Hospital in Bojnourd. International Journal of Medical Investigation. 2021; 10(3):135 46. [Link]
- Sakkas GK, Giannaki CD, Karatzaferi C, Manconi M. Sleep abnormalities in multiple sclerosis. Current Treatment Options in Neurology. 2019; 21:1-12. [DOI:10.1007/s11940-019-0544-7] [PMID]
- Moradi Farsani H, Afshari P, Sadeghniiat Haghighi K, Gholamzadeh Jefreh M, Abedi P, Haghighizadeh MH. The effect of group cognitive behavioural therapy for insomnia in postmenopausal women. Journal of Sleep Research. 2021; 30(5):e13345. [DOI:10.1111/jsr.13345] [PMID]
- Anderson KN. Insomnia and cognitive behavioural therapy-how to assess your patient and why it should be a standard part of care. Journal of Thoracic Disease. 2018; 10(Suppl 1):S94. [DOI:10.21037/jtd.2018.01.35] [PMID]
- Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020; 45(1):74-89. [DOI:10.1038/s41386-019-0411-y] [PMID]
- Tanaka M, Kusaga M, Nyamathi AM, Tanaka K. Effects of brief cognitive behavioral therapy for insomnia on improving depression among community dwelling older adults: A randomized controlled comparative study. Worldviews on Evidence Based Nursing. 2019; 16(1):78 86. [DOI:10.1111/wvn.12342] [PMID]
- Espie CA. Standard CBT-I Protocol for the Treatment of Insomnia Disorder. In: Baglioni C, Espie CA, Riemann D, European Sleep Research Society, European Insomnia Network, European Academy for Cognitive Behavioural Therapy for Insomnia, editors. Cognitive-Behavioural Therapy For Insomnia (CBT-I) Across The Life Span: Guidelines and Clinical Protocols for Health Professionals. New Jersey: John Wiley & Sons Ltd; 2022. [Link]
- Dastres F, Ghaljeh M, Jalalodini A, Ghaljaei F. The effect of distance teaching to mothers on primary school boys’ sleep habits related to computer games: A quasi experimental study. International Journal of Pediatrics. 2022; 10(3):15653 63. [Link]
- Edinger JD, Arnedt JT, Bertisch SM, Carney CE, Harrington JJ, Lichstein KL, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: An American Academy of Sleep Medicine systematic review, meta analysis, and GRADE assessment. Journal of Clinical Sleep Medicine. 2021; 17(2):263-98. [DOI:10.5664/jcsm.8988]
- Mostafa Amer H, Sh Shehata H, Hasan Alam F, Kamal Mohamed Sweelam R, Mostafa Arrab M. Effectiveness of cognitive behavioral therapy intervention on depressive symptoms and sleep quality among postnatal women. Egyptian Journal of Health Care. 2022; 13(3):940 56. [DOI:10.21608/ejhc.2022.255807]
- Yeung T, Martin JL, Fung CH, Fiorentino L, Dzierzewski JM, Rodriguez Tapia JC, et al. Sleep outcomes with cognitive behavioral therapy for insomnia are similar between older adults with low vs high self reported physical activity. Frontiers in Aging Neuroscience. 2018; 10:274. [DOI:10.3389/fnagi.2018.00274] [PMID]
- Chen HY, Cheng IC, Pan Y J, Chiu YL, Hsu SP, Pai MF, et al. Cognitive behavioral therapy for sleep disturbance decreases inflammatory cytokines and oxidative stress in hemodialysis patients. Kidney International. 2011; 80(4):415-22. [DOI:10.1038/ki.2011.151] [PMID]
- Hwang J, Park S. Sex differences of sarcopenia in an elderly Asian population: The prevalence and risk factors. International Journal of Environmental Research and Public Health. 2022; 19(19):11980. [DOI:10.3390/ijerph191911980] [PMID]
- Eliopoulos C. Gerontological Nursing. Pennsylvania: Wolters Kluwer Health; 2014. [Link]
- Mohammadi Shirmahaleh F, Soleimanian L, Peymani J, Gholami Tooranposhti M, Havasi Soomar N. [Comparative study the effectiveness of Cognitive Behavioral therapy and Compassion based therapy on sleep quality and glycosylated hemoglobin in diabetic patients (Persian)]. Iranian Journal of Psychiatric Nursing. 2023; 10(6):64 -74. [DOI:10.22034/IJPN.10.6.64]
- Espie CA. Overcoming Insomnia 2nd Edition: A self help guide using cognitive behavioural techniques. London: Hachette UK; 2021. [Link]
- Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989; 28(2):193 -213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Haydari A, Ehteshamzadeh P, Marashi M. The relationship between insomnia severity, sleep quality, sleepiness and mental health disorder with academic performance in girls. Woman Cultural Psychology. 1389; 4(1):65-76.
- Goldberg D. Use of the general health questionnaire in clinical work. British Medical Journal (Clinical Research Ed). 1986; 293(6556):1188. [DOI:10.1136/bmj.293.6556.1188] [PMID]
- Taghavi S. [Validity and reliability of the general health questionnaire (GHQ 28) in college students of Shiraz University (Persian)]. Journal of Psychology. 2002; 5(4):381 -98. [Link]
- Blesa R, Pujol M, Aguilar M, Santacruz P, Bertran Serra I, Hernández G, et al. Clinical validity of the ‘mini mental state’ for Spanish speaking communities. Neuropsychologia. 2001; 39(11):1150 7. [DOI:10.1016/S0028-3932(01)00055-0] [PMID]
- Bahiraee A. [Preliminary study of the effectiveness of the brief examination of mental status in elderly people with dementia (Persian) [MA thesis]. Tehran: University of Welfare and Rehabilitation Sciences; 2000. [Link]
- Ymer L, McKay A, Wong D, Frencham K, Grima N, Tran J, et al. Cognitive behavioural therapy versus health education for sleep disturbance and fatigue after acquired brain injury: A pilot randomised trial. Annals of Physical and Rehabilitation Medicine. 2021; 64(5):101560. [DOI:10.1016/j.rehab.2021.101560] [PMID]
- Prados G, Miró E, Martínez MP, Sánchez AI, Lami MJ, Cáliz R. Combined cognitive behavioral therapy for fibromyalgia: Effects on polysomnographic parameters and perceived sleep quality. International Journal of Clinical and Health Psychology. 2020; 20(3):232-42. [DOI:10.1016/j.ijchp.2020.04.002] [PMID]
- Redeker NS, Jeon S, Andrews L, Cline J, Mohsenin V, Jacoby D. Effects of cognitive behavioral therapy for insomnia on sleep related cognitions among patients with stable heart failure. Behavioral Sleep Medicine. 2019; 17(3):342-54. [DOI:10.1080/15402002.2017.1357120] [PMID]
- Padron A, McCrae CS, Robinson ME, Waxenberg LB, Antoni MH, Berry RB, et al. Impacts of cognitive behavioral therapy for insomnia and pain on sleep in women with gynecologic malignancies: A randomized controlled trial. Behavioral Sleep Medicine. 2022; 20(4):460-76. [DOI:10.1080/15402002.2021.1932500] [PMID]
- Paardekooper D, Thayer Z, Miller L, Nikpour A, Gascoigne MB. Group based cognitive behavioral therapy program for improving poor sleep quality and quality of life in people with epilepsy: A pilot study. Epilepsy & Behavior. 2020; 104:106884. [DOI:10.1016/j.yebeh.2019.106884] [PMID]
- Carletti TM, Meira IA, Gama LT, Medeiros MMDd, Cavalcanti YW, Garcia RCMR. Association of sociodemographic characteristics, mental health, and sleep quality with COVID 19 fear in an elderly Brazilian population. Brazilian Journal of Oral Sciences. 2023; 22:e238271. [DOI:10.20396/bjos.v22i00.8668271]
- Alavi SMA, Irani RD, Fattahi P, Pakseresht S. Effects of brief cognitive behavioral therapy on mental health in substance related disorder: A randomized controlled trial. BMC Psychiatry. 2023; 23(1):924. [DOI:10.1186/s12888-023-05413-4] [PMID]
- Axelsson E, Andersson E, Ljótsson B, Björkander D, Hedman Lagerlöf M, Hedman Lagerlöf E. Effect of internet vs face to face cognitive behavior therapy for health anxiety: A randomized noninferiority clinical trial. JAMA Psychiatry. 2020; 77(9):915-24. [DOI:10.1001/jamapsychiatry.2020.0940] [PMID]
- Weintraub MJ, Denenny D, Ichinose MC, Zinberg J, Morgan Fleming G, Done M, et al. A randomized trial of telehealth mindfulness based cognitive therapy and cognitive behavioral therapy groups for adolescents with mood or attenuated psychosis symptoms. Journal of Consulting and Clinical Psychology. 2023; 91(4):234. [DOI:10.1037/ccp0000782] [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/07/31 | Accepted: 2024/12/4 | Published: 2024/07/31
Received: 2024/07/31 | Accepted: 2024/12/4 | Published: 2024/07/31
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |