Tue, Feb 17, 2026
| فارسی
Volume 31, Issue 1 (Continuously Updated 2025)
IJPCP 2025, 31(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fathi F, Vaziri S, Pourasghar M, Nasri M. Transference-focused Psychotherapy Versus Acceptance & Commitment Therapy on Personality Organization and Defense Styles of People With BPD: A Clinic Trial. IJPCP 2025; 31 (1)
URL: http://ijpcp.iums.ac.ir/article-1-4166-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4166-en.html
1- Department of Psychology, Birjand Medical School, Birjand Branch, Islamic Azad University, Birjand, Iran.
2- Department of Fellowship and Spirituality Therapy, Faculty of Medicine, Roodehen Branch, Islamic Azad University, Roodehen, Iran. ,shahram.vaziri@gmail.com.
3- Department of Psychiatry, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Fellowship and Spirituality Therapy, Faculty of Medicine, Roodehen Branch, Islamic Azad University, Roodehen, Iran. ,
3- Department of Psychiatry, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
Keywords: Transference-focused psychotherapy, Acceptance & commitment therapy, Personality organization, Defense styles, borderline personality disorder
Full-Text [PDF 7869 kb]
(107 Downloads)
| Abstract (HTML) (294 Views)
Full-Text: (97 Views)
Introduction
It is important to understand the patient’s personality organization when planning psychotherapy and observing its results. Kernberg recognized three levels of personality organization: neurotic, borderline, and psychotic. Borderline personality disorder (BPD) is a common mental disorder that is associated with high rates of suicide, severe functional impairment, high rates of comorbid mental disorders, high use of treatment, high use of defense mechanisms, and high cost burden on the healthcare system. Defense mechanisms are automatic regulatory processes that act to reduce cognitive abnormalities and minimize sudden changes in reality and perception of threatening events. Studies have indicated the effectiveness of psychotherapy methods for BPD patients, including the transference-focused psychotherapy (TFP), whose goal is to change symptoms and interpersonal problems through structured psychological care that corrects mental representations of self and others. This process leads to behavior conduction. Another treatment option for these patients is acceptance and commitment therapy (ACT). ACT begins with fundamental research on human distress and establishes a general psychological model, collecting related interventions.
There are several organized psychotherapies for BPD, but none of them have priority over the others in reducing symptoms. It is essential to explore why TFP and ACT are unique. In fact, we choose these types of treatment because their goals are beyond symptom reduction. The main question is whether TFP and ACT are effective in addressing personality organization and defensive styles in people with BPD.
Method
In this randomized clinical trial, the study population consisted of all individuals with BPD referred to Zare Psychiatric Hospital and Khaney-e Ma’na Clinic in Sari, north of Iran, in 2020 (n=32). Those who met the entry criteria were selected using a convenience sampling method (n=11) and were randomly assigned to TFP (n=4), ACT (n=4), and control (n=3) groups using a lottery method. The questionnaires included Kernberg’s Inventory of Personality Organization (IPO) and Defense Styles Questionnaire. The TFP and ACT interventions were provided for one year, two sessions per week, each for 48 minutes, following the formal treatment protocols, done by trained therapists. Data were collected before the interventions, at the first session, during the 40th session, during the 80th session, at the 100th session (after intervention), and six months after interventions (follow-up). The TFP sessions were conducted under the supervision of two experts—one from Iran and one from Sweden. For ACT, another supervisor from Iran was also involved. Both therapy sessions adhered to the official guidelines established for these treatments.
Results
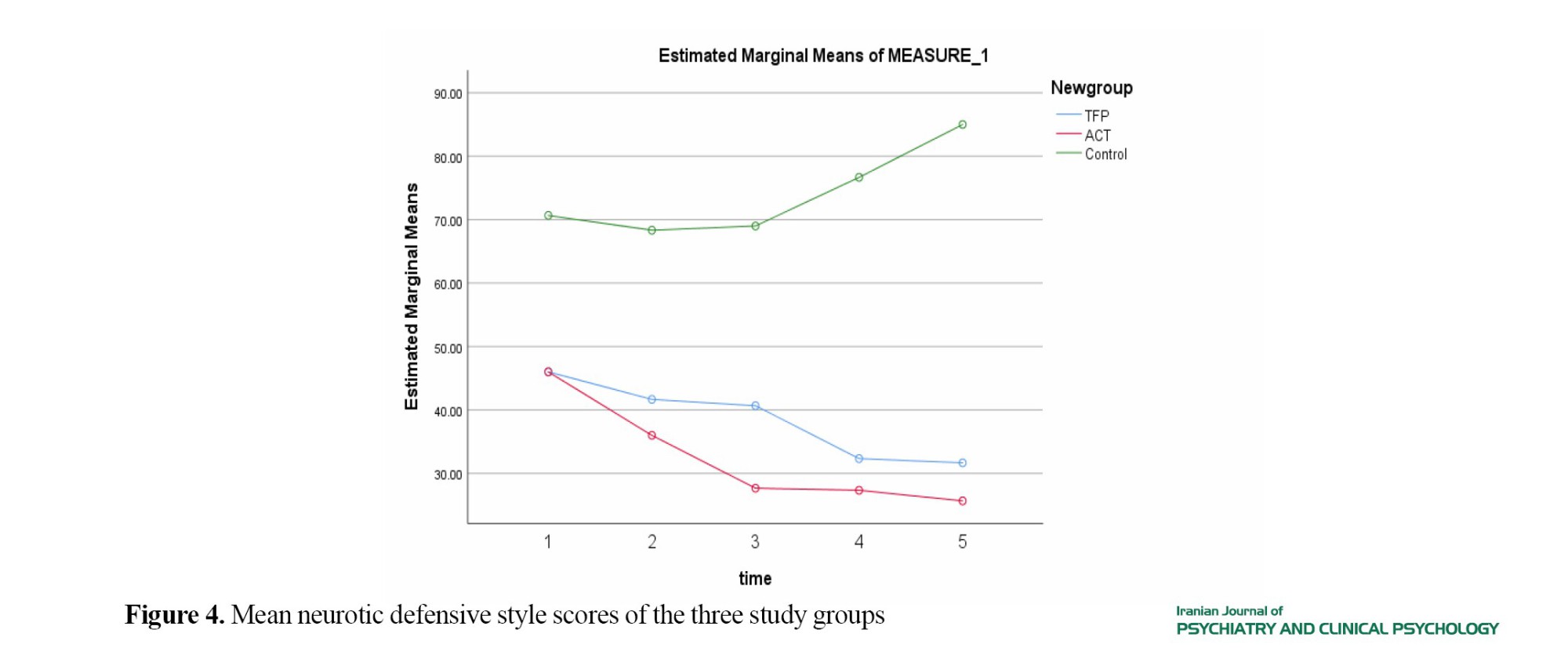
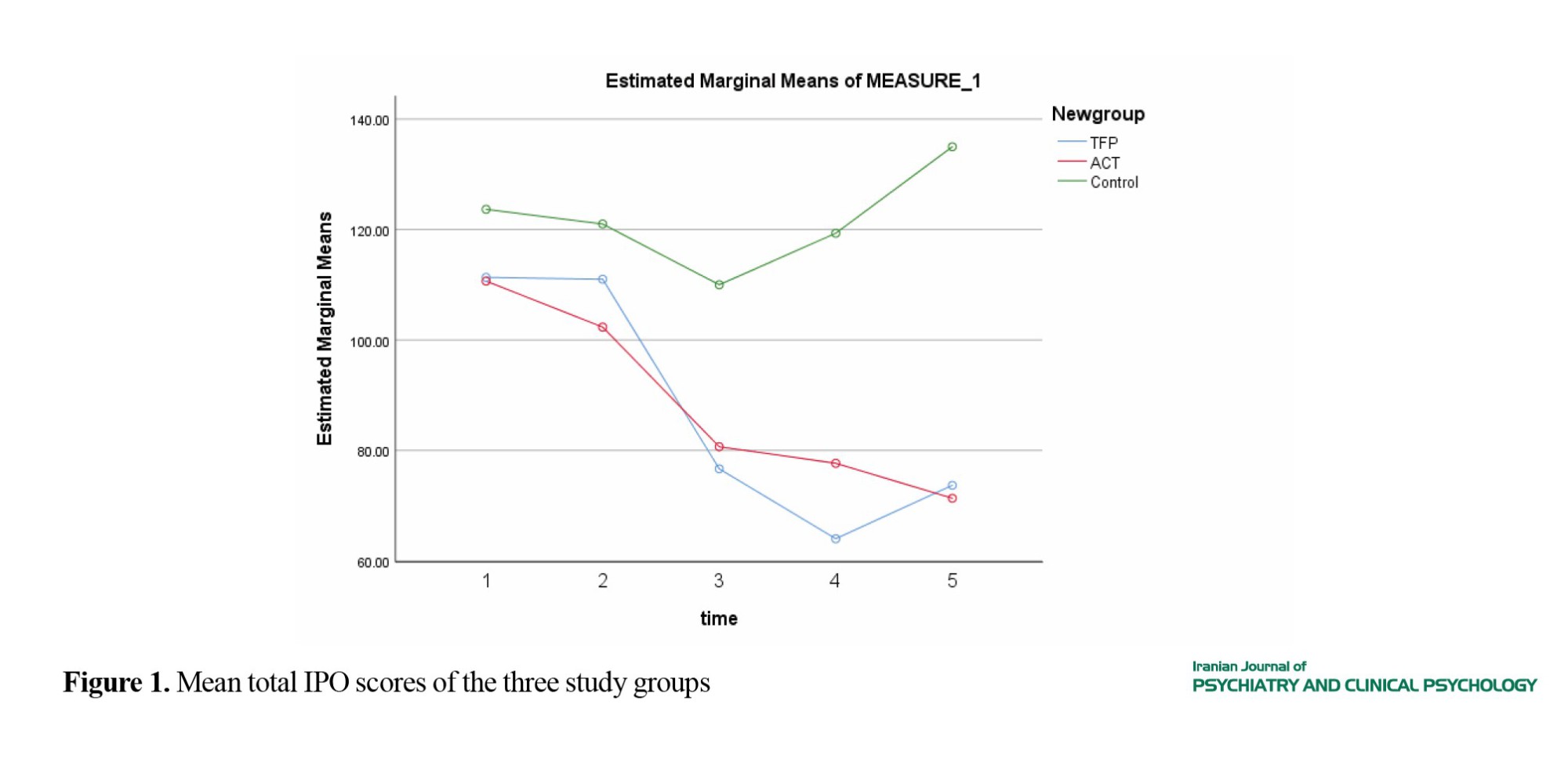
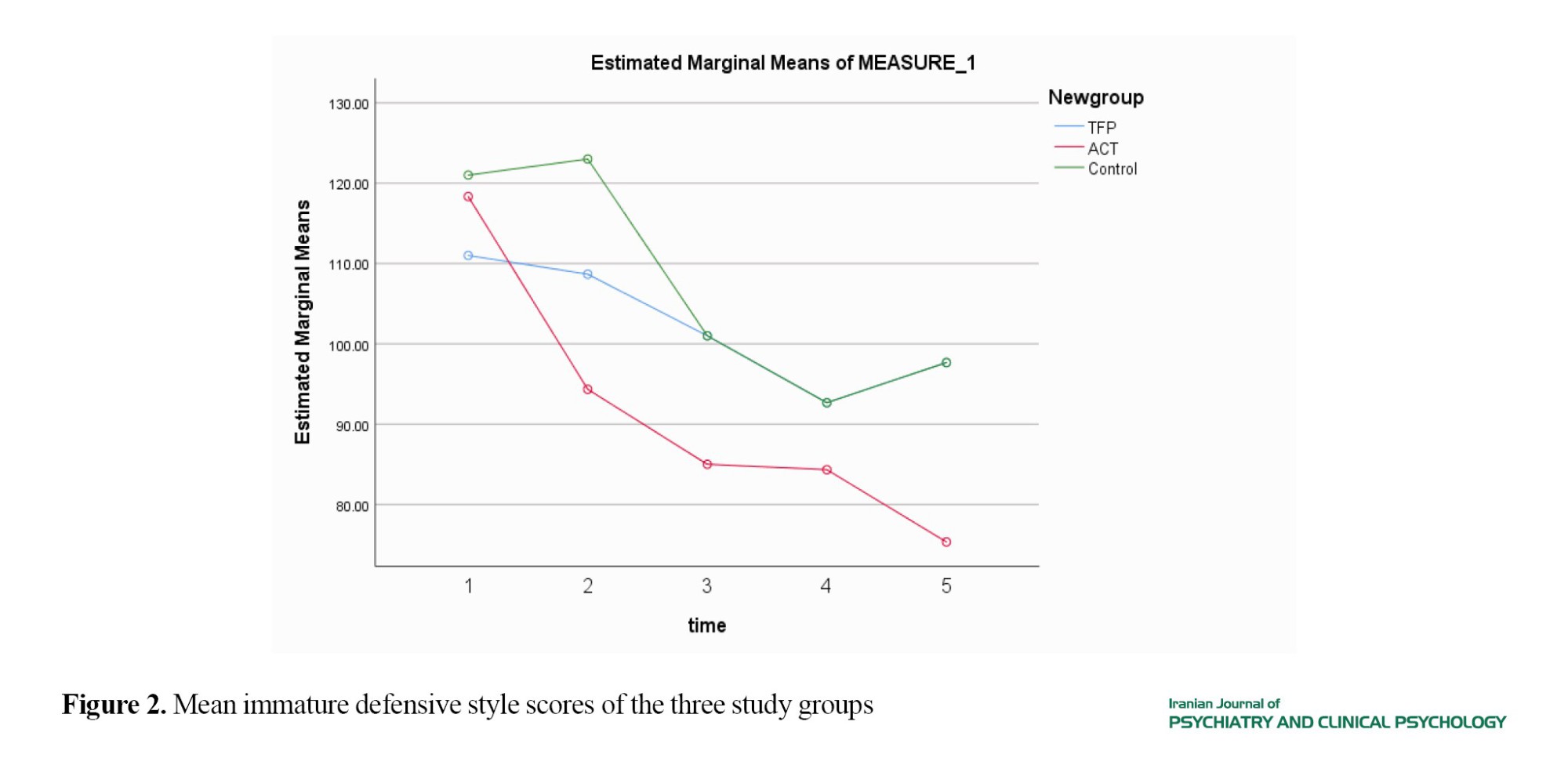
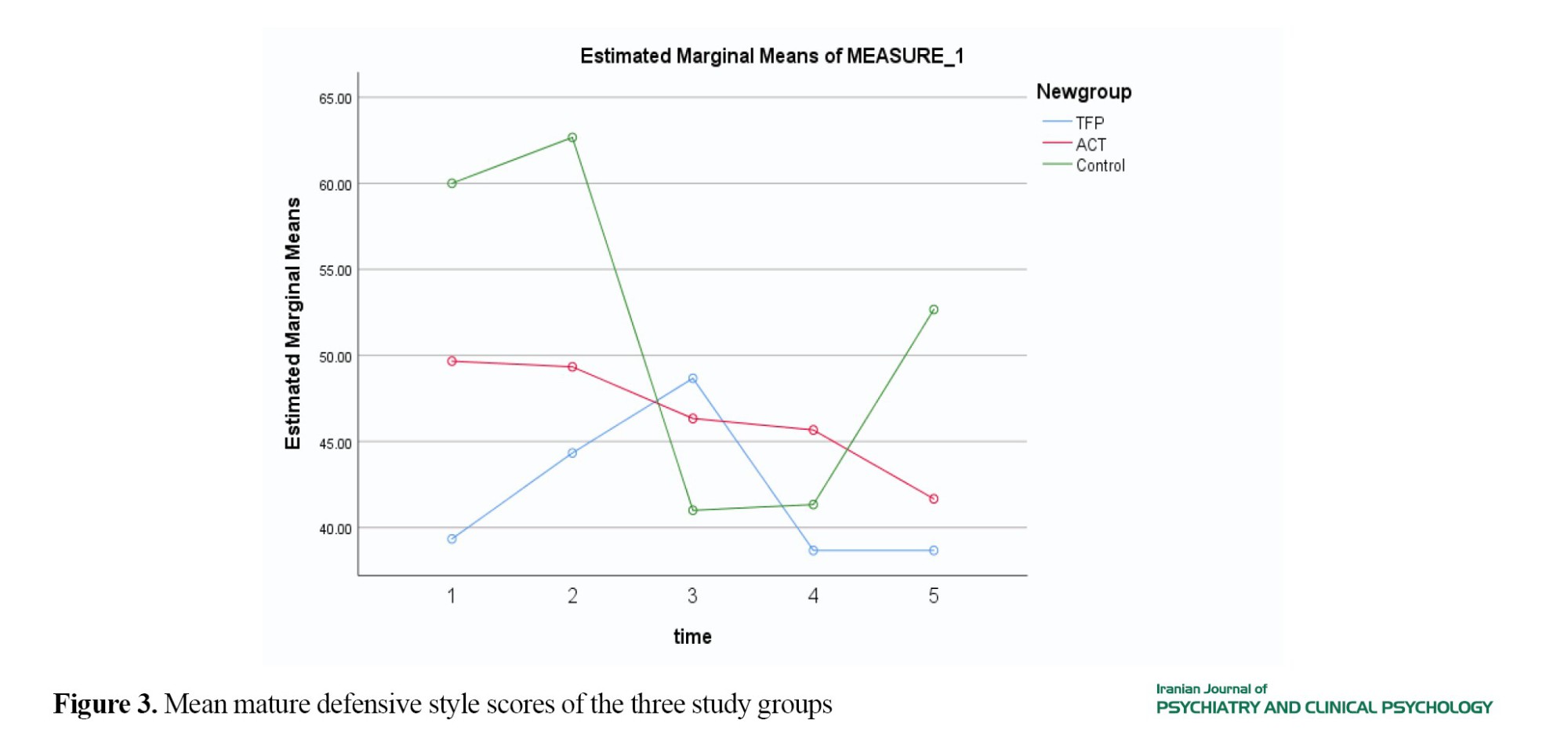
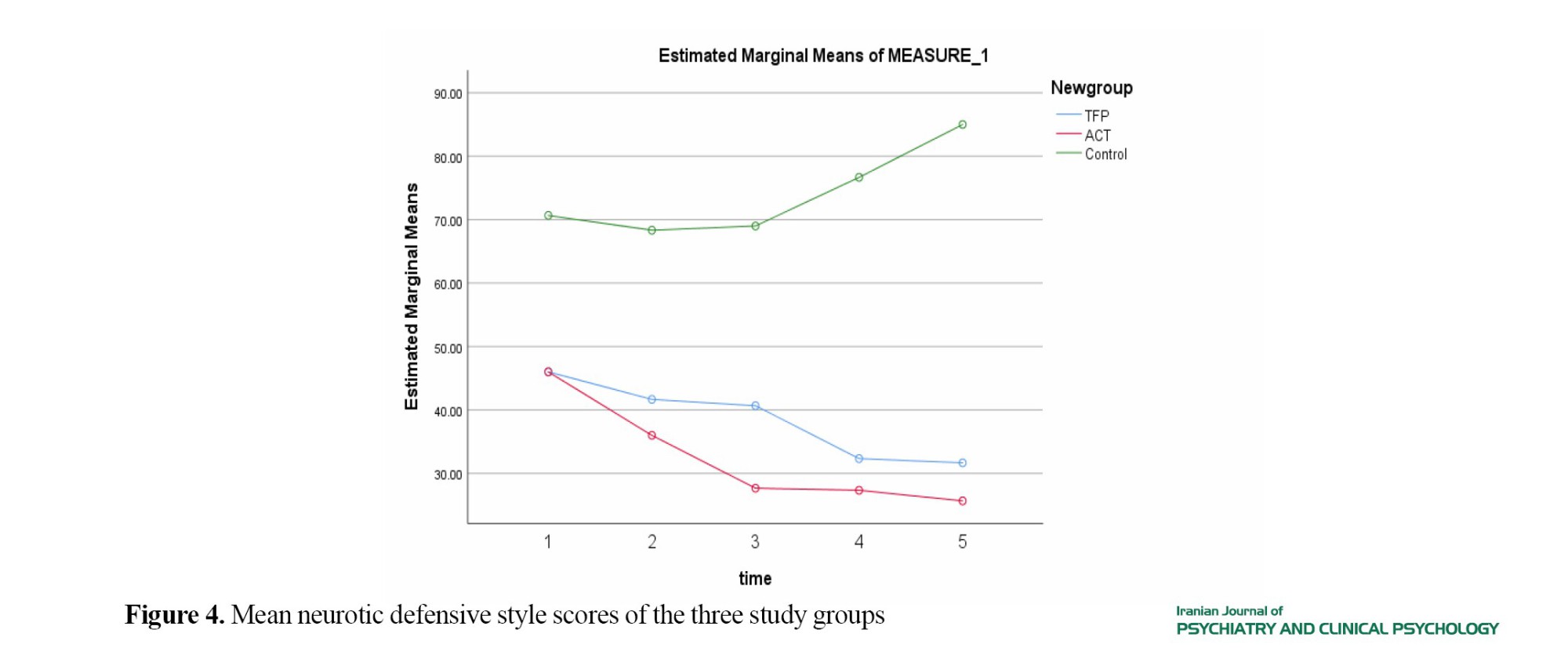
Figures 1, 2, 3, and 4 show the mean scores of the study variables for three groups. There was a statistically significant difference in the total IPO score among the groups (P=0.023). Regarding the IPO domains, the difference was also significant in primitive psychological defences, reality testing, and identity diffusion (P<0.05). There was no significant difference in the immature defensive style (P=0.603), but a significant difference was found in the mature defensive style (P=0.041) and neurotic defensive style (P=0.366).
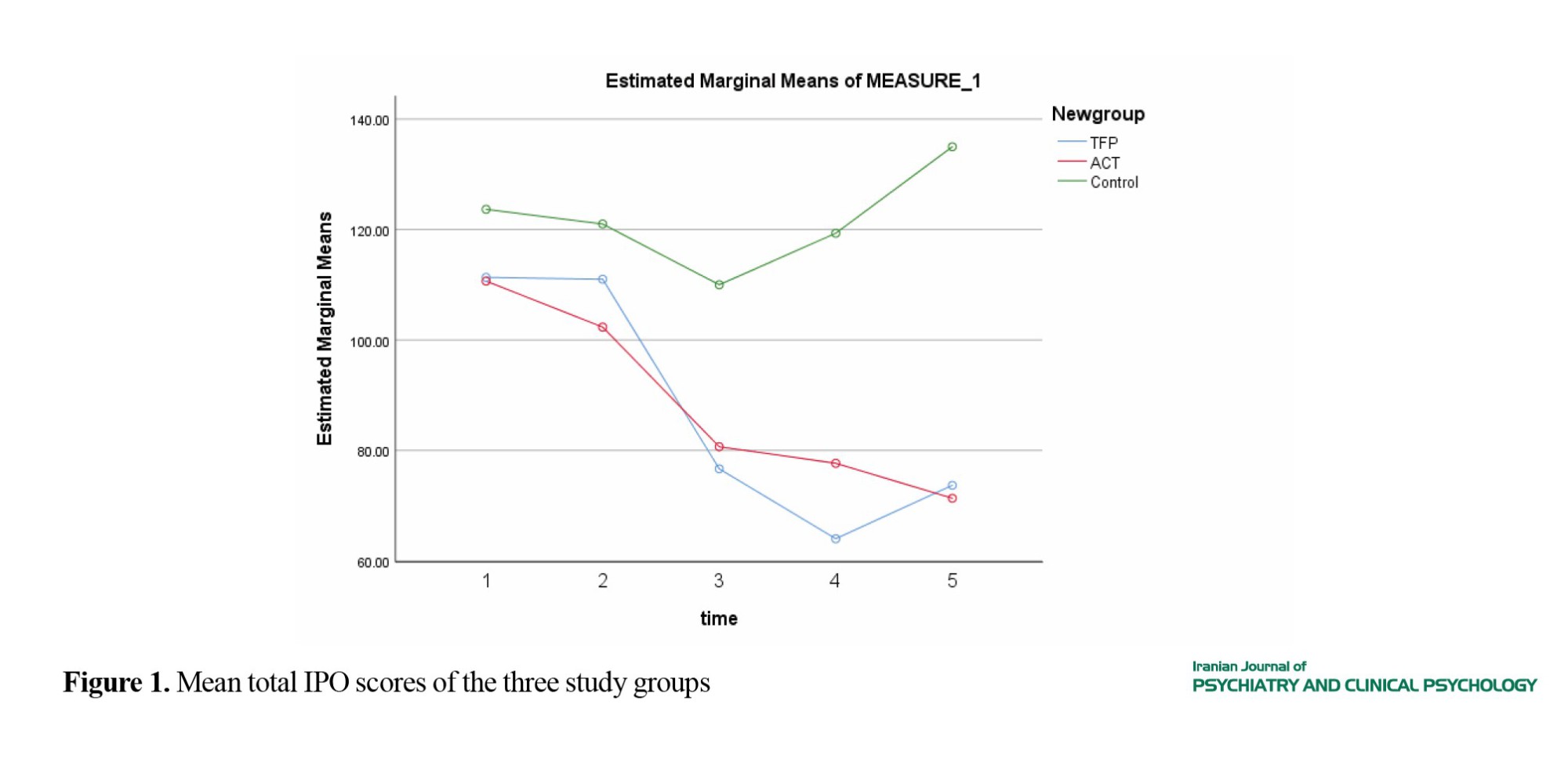
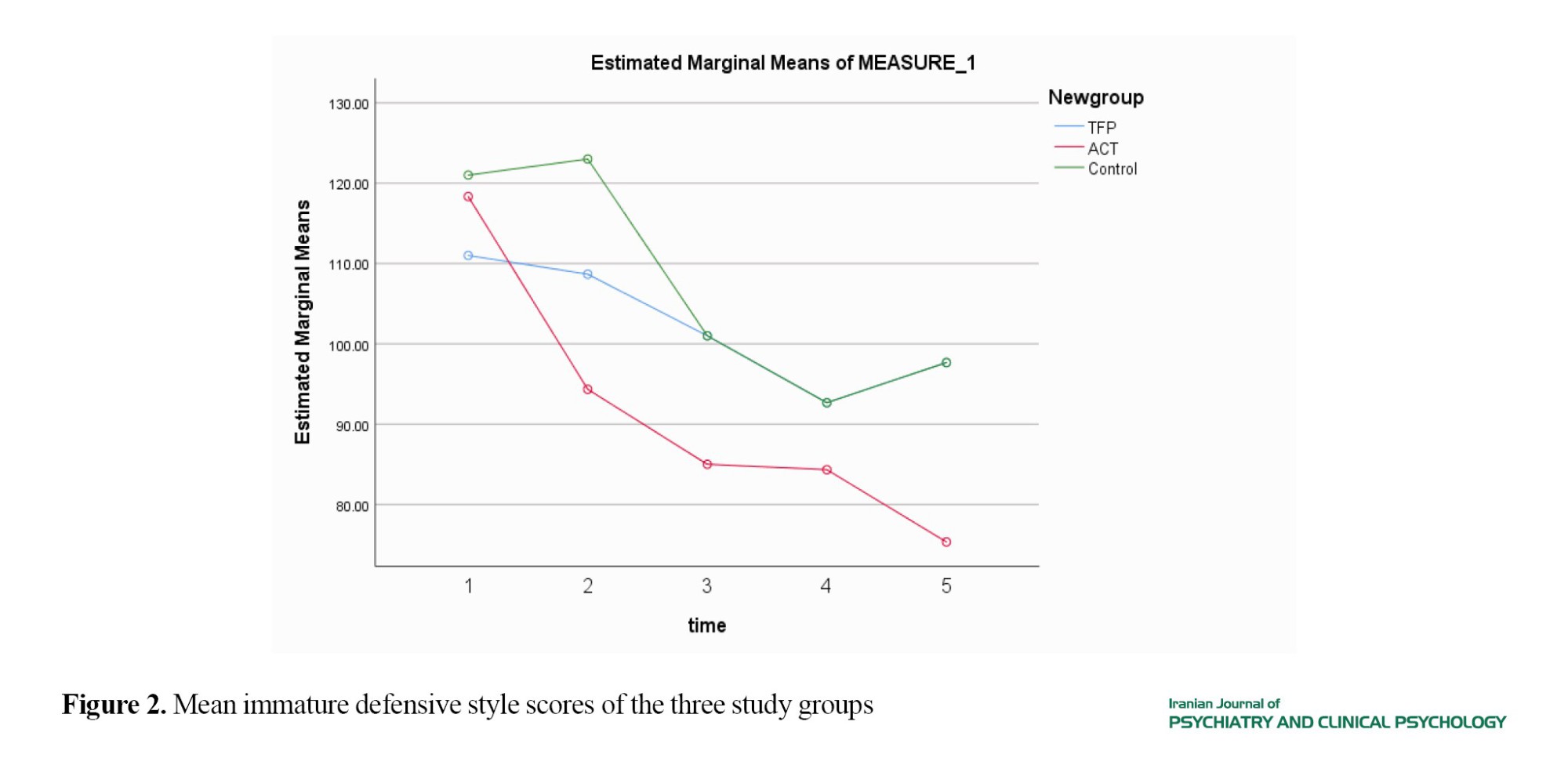
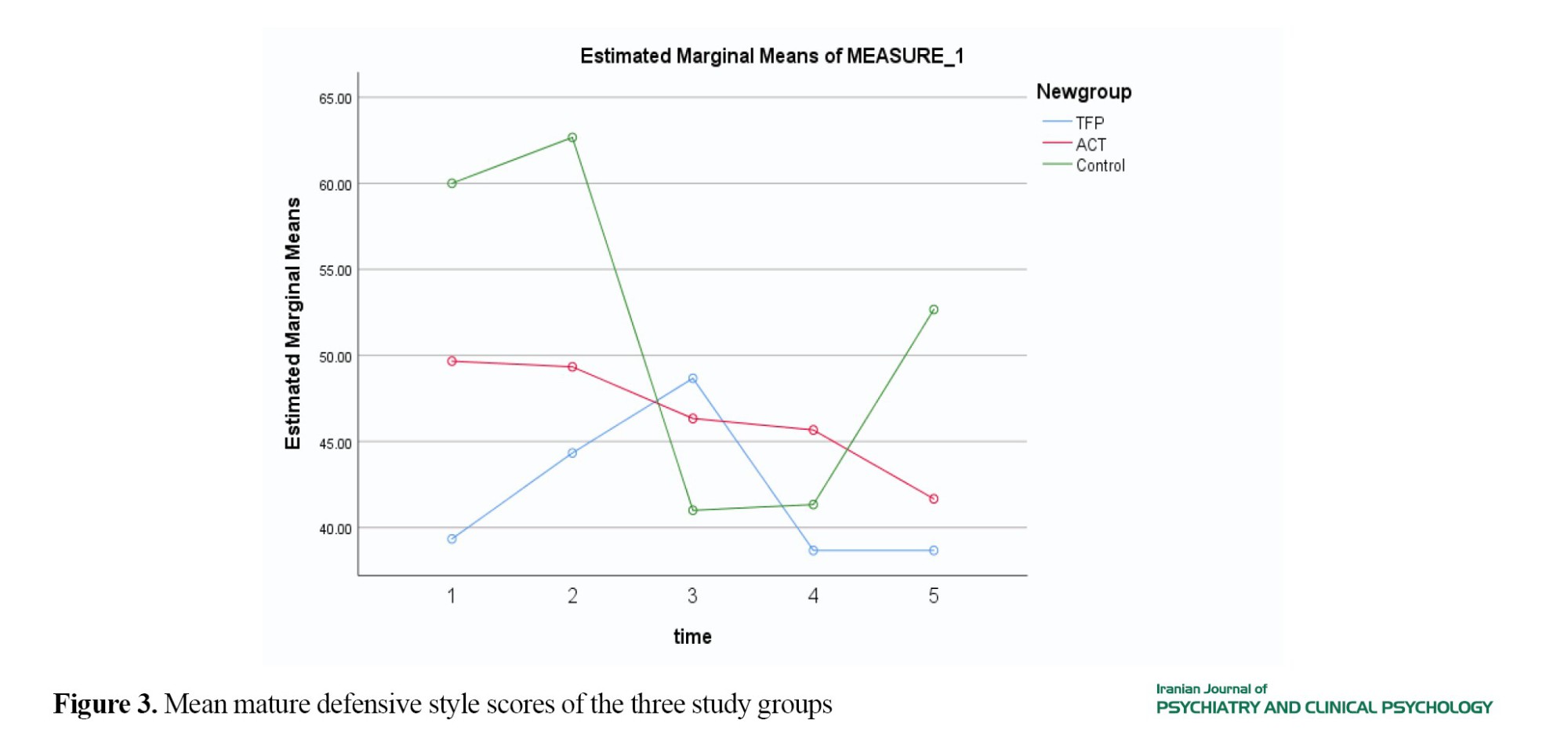
Conclusion
The findings demonstrated that both TFP and ACT were effective in improving personality organization in patients with BPD. Additionally, both TFP and ACT have a significant impact on the defense styles of these patients. For TFP, the effectiveness is observed in mature, neurotic, and immature defensive styles. In contrast, ACT only affects immature and mature defensive styles. It is recommended that future studies combine TFP and ACT and use larger samples to obtain more generalizable results.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the committee of Birjand University of Medical Science (Code: IR.BUMS.REC.1399.245) and was registered by the Iranian Registry of Clinical Trails (ID: IRCT20131007014928N7).
Funding
This article was extracted from the PhD thesis of Fatemeh Fathi at Islamic Azad University Birjand, Birjand. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Authors contributions
Conceptualization and initial draft preparation: Fatemeh Fathi; Supervision: Shahram Vaziri and Mehdi PourasghR. Methodology: Maryam Nasri.
Conflicts of interest
The authors declare no conflict of interest
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
It is important to understand the patient’s personality organization when planning psychotherapy and observing its results. Kernberg recognized three levels of personality organization: neurotic, borderline, and psychotic. Borderline personality disorder (BPD) is a common mental disorder that is associated with high rates of suicide, severe functional impairment, high rates of comorbid mental disorders, high use of treatment, high use of defense mechanisms, and high cost burden on the healthcare system. Defense mechanisms are automatic regulatory processes that act to reduce cognitive abnormalities and minimize sudden changes in reality and perception of threatening events. Studies have indicated the effectiveness of psychotherapy methods for BPD patients, including the transference-focused psychotherapy (TFP), whose goal is to change symptoms and interpersonal problems through structured psychological care that corrects mental representations of self and others. This process leads to behavior conduction. Another treatment option for these patients is acceptance and commitment therapy (ACT). ACT begins with fundamental research on human distress and establishes a general psychological model, collecting related interventions.
There are several organized psychotherapies for BPD, but none of them have priority over the others in reducing symptoms. It is essential to explore why TFP and ACT are unique. In fact, we choose these types of treatment because their goals are beyond symptom reduction. The main question is whether TFP and ACT are effective in addressing personality organization and defensive styles in people with BPD.
Method
In this randomized clinical trial, the study population consisted of all individuals with BPD referred to Zare Psychiatric Hospital and Khaney-e Ma’na Clinic in Sari, north of Iran, in 2020 (n=32). Those who met the entry criteria were selected using a convenience sampling method (n=11) and were randomly assigned to TFP (n=4), ACT (n=4), and control (n=3) groups using a lottery method. The questionnaires included Kernberg’s Inventory of Personality Organization (IPO) and Defense Styles Questionnaire. The TFP and ACT interventions were provided for one year, two sessions per week, each for 48 minutes, following the formal treatment protocols, done by trained therapists. Data were collected before the interventions, at the first session, during the 40th session, during the 80th session, at the 100th session (after intervention), and six months after interventions (follow-up). The TFP sessions were conducted under the supervision of two experts—one from Iran and one from Sweden. For ACT, another supervisor from Iran was also involved. Both therapy sessions adhered to the official guidelines established for these treatments.
Results
Figures 1, 2, 3, and 4 show the mean scores of the study variables for three groups. There was a statistically significant difference in the total IPO score among the groups (P=0.023). Regarding the IPO domains, the difference was also significant in primitive psychological defences, reality testing, and identity diffusion (P<0.05). There was no significant difference in the immature defensive style (P=0.603), but a significant difference was found in the mature defensive style (P=0.041) and neurotic defensive style (P=0.366).
Conclusion
The findings demonstrated that both TFP and ACT were effective in improving personality organization in patients with BPD. Additionally, both TFP and ACT have a significant impact on the defense styles of these patients. For TFP, the effectiveness is observed in mature, neurotic, and immature defensive styles. In contrast, ACT only affects immature and mature defensive styles. It is recommended that future studies combine TFP and ACT and use larger samples to obtain more generalizable results.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the committee of Birjand University of Medical Science (Code: IR.BUMS.REC.1399.245) and was registered by the Iranian Registry of Clinical Trails (ID: IRCT20131007014928N7).
Funding
This article was extracted from the PhD thesis of Fatemeh Fathi at Islamic Azad University Birjand, Birjand. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Authors contributions
Conceptualization and initial draft preparation: Fatemeh Fathi; Supervision: Shahram Vaziri and Mehdi PourasghR. Methodology: Maryam Nasri.
Conflicts of interest
The authors declare no conflict of interest
Acknowledgments
The authors would like to thank all participants for their cooperation in this study.
References
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, et al. Treatment utilization by patients with personality disorders. The American Journal of Psychiatry. 2001; 158(2):295-302. [DOI:10.1176/appi.ajp.158.2.295] [PMID]
- Genderson J, Hoffman P. Diagnosis and treatment of borderline personality disorder [ S. M. Jafarzadeh & M. Mirshajaeian, Persian trans.]. Tehran: Arjmand Publishing; 2005. [Link]
- Beck A, Freeman D, Davis D. Cognitive Therapy of personality disorders, second edition. New York: Guilford Press; 2004. [Link]
- The American Psychiatric Association. Diagnostic and statistical guide to DSM 5 [F. Gholamialn, S. S. Moosavi Nadoshan, A. Mohamad Sadegh, Persian trans]. Tehran: Ebn-E-Sina; 2015. [Link]
- Soeteman DI, Hakkaart-van Roijen L, Verheul R, Busschbach JJ. The economic burden of personality disorders in mental health care. The Journal of Clinical Psychiatry. 2008; 69(2):259-65. [DOI:10.4088/JCP.v69n0212] [PMID]
- Lenzenweger MF, Clarkin JF, Kernberg OF, Foelsch PA. The inventory of personality organization: Psychometric properties, factorial composition, and criterion relations with affect, aggressive dyscontrol, psychosis proneness, and self-domains in a nonclinical sample. Psychological Assessment. 2001; 13(4):577-91. [DOI:10.1037//1040-3590.13.4.577] [PMID]
- Kernberg O. Borderline personality organization. Journal of the American Psychoanalytic Association. 1967; 15(3):641-85. [DOI:10.1177/000306516701500309] [PMID]
- Clarkin JF. Transference-focused psychotherapy for borderline personality disorder: A clinical guide. Washington: American Psychiatric Publishing; 2015. [Link]
- Vaillant GE. Ego mechanisms of defense and personality psychopathology. Journal of Abnormal Psychology. 1994; 103(1):44-50. [DOI:10.1037//0021-843X.103.1.44] [PMID]
- Shafi Abadi A, Nasseri G. [Psychotherapy theories (Persian)]. Tehran: University Publishing Center; 2010. [Link]
- Perry JC, Presniak MD, Olson TR. Defense mechanisms in schizotypal, borderline, antisocial, and narcissistic personality disorders. Psychiatry. 2013; 76(1):32-52. [DOI:10.1521/psyc.2013.76.1.32] [PMID]
- Kramer U, de Roten Y, Perry JC, Deplaned JN. Beyond splitting: Observer-rated defense mechanisms in borderline personality disorder, Psychoanalytic Psychology. 2013; 30(1):15-30. [DOI:10.1037/a0029463]
- Clarkin JF, Cain NM, Lenzenweger MF. Advances in transference-focused psychotherapy derived from the study of borderline personality disorder: Clinical insights with a focus on mechanism. Current Opinion in Psychology. 2018; 21:80-85. [DOI:10.1016/j.copsyc.2017.09.008] [PMID]
- Fassbinder E, Schuetze M, Kranich A, Sipos V, Hohagen F, Shaw I, et al. Feasibility of group schema therapy for outpatients with severe borderline personality disorder in germany: A pilot study with three year follow-up. Frontiers in Psychology. 2016; (7):1851. [DOI:10.3389/fpsyg.2016.01851]
- Stoffers-Winterling JM, Storebø OJ, Kongerslev MT, Faltinsen E, Todorovac A, Sedoc Jørgensen M, et al. Psychotherapies for borderline personality disorder: A focused systematic review and meta-analysis. The British Journal of Psychiatry. 2022; 221(3):538-52. [DOI:10.1192/bjp.2021.204] [PMID]
- Rashn S, Makvand-Hosseini S, Rezaei A, Tabatabaee S. [The effect of long-term dynamic psychotherapy on the personality structure of patients with Dependent Personality Disorder (Persian)]. Journal of Clinical Psychology. 2018; 9(4):1-2. [DOI:10.22075/jcp.2018.13685.1343]
- Khorianian M, Bakhshipour-Roudsari A, Mahmoud-Alilou M, Hashemi T. [Effectiveness of transference-focused psychotherapy on reflective functioning and symptomatology of the borderline personality disordered patients (Persian)]. Journal of Clinical Psychology. 2019; 10(4):45-58. [DOI:10.22075/jcp.2019.15996.1531]
- Morton j, Snowdon S, Gopold M, Guymer E. Acceptance and commitment therapy group treatment for symptoms of borderline personality disorder: A public sector pilot study. Journal of Cognitive and Behavioral Practice. 2012; 19(4):527-44. [DOI:10.1016/j.cbpra.2012.03.005]
- Chapman AL. Acceptance and mindfulness in behavior therapy: A comparison of dialectical behavior therapy and acceptance and commitment therapy. International Journal of Behavioral Consultation and Therapy. 2006; 2(3):308-13. [DOI:10.1037/h0100785]
- Bach P, Moran DC. ACT in practice the conceptualization of the case in the treatment of acceptance and commitment [ S. Kamali & N. Kian Rad, Persian trans.]. Tehran: Arjmand Publishing; 2017. [Link]
- Reyes-Ortega MA, Miranda EM, Fresán A, Vargas AN, Barragán SC, Robles García R, et al. Clinical efficacy of a combined acceptance and commitment therapy, dialectical behavioural therapy, and functional analytic psychotherapy intervention in patients with borderline personality disorder. Psychology and Psychotherapy. 2020; 93(3):474-89. [DOI:10.1111/papt.12240] [PMID]
- Shaw L, Gopold M, Tisbury N, Wyman K. Acceptance and Commitment Therapy Group Treatment for Borderline Personality Disorder. Australian Postgraduate Medicine. 2012.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM 5 [ F. Rezaei, A. Fakhrai, A. Farmand, A. Niloufri, J. Hashemi Azar& F. Shamloo, Persian trans]. Tehran: Arjomand Publishing; 2014. [Link]
- Khodabakhsh R. [Comparing the prevalence of personality disorders in men and women using adjusted raw scores of the Million III (Persian)]. Quarterly Journal of Cultural and Educational Studies of Women and Family. 2013 ; 7(22), 103-125. [Link]
- Sperry, L. Handbook of diagnosis and treatment of DSM-IV-TR personality disorders: Assessment, case conceptualization, and treatment, third edition. New York: Brunner Rutledge; 2003. [DOI:10.4324/9780203427088]
- Keng SL, Tan HH. Effects of brief mindfulness and loving-kindness meditation inductions on emotional and behavioral responses to social rejection among individuals with high borderline personality traits. Behaviour Research and Therapy. 2018; 100:44-53. [DOI:10.1016/j.brat.2017.11.005] [PMID]
- Al Behbahani M, Mohammadi N. [Investigating the Psychometric Characteristics of the Cornberg Personality Organization. Examining the psychometric properties of Kernberg’s personality organization inventory (Persian)]. Journal of Psychology. 2017; 11(2):186-97. [Link]
- Lenzenweger MF, Clarkin JF, Levy KN, Yeomans FE, Kernberg OF. Predicting domains and rates of change in borderline personality disorder. Personality Disorders. 2012; 3(2):185-95. [DOI:10.1037/a0025872] [PMID]
- Yeomans FE, Clarkin JF, Kernberg OF. Transference-focused psychotherapy for borderline personality disorder: A clinician’s guide. Washington: American Psychiatric Publishing; 2015. [DOI:10.1176/appi.books.9781615371006]
- Heydari Nasab L, Shu’iri, MR. [Factor of defense style questionnaire (DSQ-40) in Iranian non-clinical samples (Persian)]. Journal of Modern Psychological Research. 2011; 6(21):77-97. [Link]
- Stern BL, Yeomans F. The psychodynamic treatment of borderline personality disorder: An introduction to transference-focused psychotherapy. The Psychiatric Clinics of North America. 2018; 41(2):207-23. [DOI:10.1016/j.psc.2018.01.012] [PMID]
- Gabbard GO, Horowitz MJ. Insight, transference interpretation, and therapeutic change in the dynamic psychotherapy of borderline personality disorder. The American Journal of Psychiatry. 2009; 166(5):517-21. [DOI:10.1176/appi.ajp.2008.08050631] [PMID]
- Hayes SC. The state of the ACT evidence. Houston, TX: Assocciation for Contextual Behavior Science(ACBS); 2007. [Link]
- Freeman A. Comparative treatments for borderline personality disorder. New York: Springer; 2005. [Link]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/12/14 | Accepted: 2025/08/16 | Published: 2025/09/23
Received: 2024/12/14 | Accepted: 2025/08/16 | Published: 2025/09/23
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |