Sat, Feb 14, 2026
| فارسی
Volume 30, Issue 1 (Continuously Updated 2024)
IJPCP 2024, 30(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kami M, Pourshahbaz A, Rezaei O, Keshavarz-Akhlaghi A, Banihashem S S, Dehghanizadeh Z, et al . Clinical Symptoms and Personality Traits of Inpatients With Borderline Personality Disorder in Iran. IJPCP 2024; 30 (1) : 4982.1
URL: http://ijpcp.iums.ac.ir/article-1-4160-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4160-en.html
Maryam Kami1 

 , Abbas Pourshahbaz2
, Abbas Pourshahbaz2 

 , Omid Rezaei3
, Omid Rezaei3 

 , Amir-Abbas Keshavarz-Akhlaghi4
, Amir-Abbas Keshavarz-Akhlaghi4 

 , Seyed Shahab Banihashem5
, Seyed Shahab Banihashem5 

 , Zahra Dehghanizadeh1
, Zahra Dehghanizadeh1 

 , Marzie Olamaie Koopaie6
, Marzie Olamaie Koopaie6 

 , Masoud Nosratabadi1
, Masoud Nosratabadi1 




 , Abbas Pourshahbaz2
, Abbas Pourshahbaz2 

 , Omid Rezaei3
, Omid Rezaei3 

 , Amir-Abbas Keshavarz-Akhlaghi4
, Amir-Abbas Keshavarz-Akhlaghi4 

 , Seyed Shahab Banihashem5
, Seyed Shahab Banihashem5 

 , Zahra Dehghanizadeh1
, Zahra Dehghanizadeh1 

 , Marzie Olamaie Koopaie6
, Marzie Olamaie Koopaie6 

 , Masoud Nosratabadi1
, Masoud Nosratabadi1 


1- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,apourshahbaz@yahoo.com
3- Department of Psychiatry, Psychosis Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Mental Health Research Center, Psychosocial Health Research Institute (PHRI), Department of Psychiatry, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Psychosomatic Medicine, Taleghani Hospital Research Development Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
6- Razi Educational and Therapeutic Psychiatric Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
3- Department of Psychiatry, Psychosis Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Mental Health Research Center, Psychosocial Health Research Institute (PHRI), Department of Psychiatry, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Psychosomatic Medicine, Taleghani Hospital Research Development Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
6- Razi Educational and Therapeutic Psychiatric Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Full-Text [PDF 6868 kb]
(623 Downloads)
| Abstract (HTML) (1976 Views)
Full-Text: (795 Views)
Introduction
Borderline personality disorder (BPS) is a serious mental disorder that is characterized by instability in self-image, interpersonal relationships, and emotions [1]. The prevalence of this disorder in the general population is estimated to be about 1%, and in psychiatric outpatients and inpatients to be 12 and 22%, respectively [6]. The pathology of this disorder is such that some patients are prone to hospitalization and rehospitalization [15]. The prevalence of suicidal thoughts and attempts among BPD patients have been estimated to be over 60% [16]. About 50% of patients admitted for suicide and self-harm risk management have BPD [17]. Psychotic symptoms, including auditory hallucinations, are another important reason for hospitalization and a risk factor for suicide in some BPD patients [18, 19]. Transient paranoia experienced under stress and characterized by exaggerated beliefs, alongside hearing “voices” (auditory hallucinations), is a psychiatric symptom that predicts hospitalization in BPD patients. Risky and uncontrolled behaviors, including extreme aggression, impulsive sexual activity, and self-medication, can also be reasons for hospitalization in BPD patients [20-22].
Not only the clinical symptoms of BPD inpatients can differ from those of BPD outpatients, but they also differ between male and female patients with BPD, although some studies have not reported any differences between the sexes [24, 25], while there are studies suggesting that emotional instability and interpersonal problems more common in female BPD patients and impulsivity and aggression more common in males [9, 11, 26]. In this study, we aim to investigate the clinical symptoms of BPD in hospitalized patients in Iran, and compare male and female inpatients in clinical symptoms and comorbid personality disorders.
Methods
The study population consists of inpatients admitted to three psychiatric centers in Iran (Iran Psychiatric Hospital, the Neurology Department of Taleghani Hospital, and Razi Psychiatric Hospital). During one year, 120 inpatients were introduced to the research team, of whom 26 inpatients did not meet the diagnostic criteria for BPD, and 7 inpatients were excluded due to incomplete responses to the questionnaires. Finally, data from 87 inpatients (64 females and 23 males) were included in the analysis. The data were collected using the Personality Inventory for DSM-5 (PID-5), the Structured Clinical Interview for DSM-5 Screening Personality Questionnaire, and the Structured Clinical Interview for DSM-5 Personality Disorders. To examine the difference in clinical variables based on sex, the chi-square test was used. To compare men and women in PID-5 scores, the one-way analysis of variance (ANOVA) was used.
Results
The mean age of the inpatients was 27.23±7.31 years. The frequencies of clinical symptoms of BPD and comorbid personality disorders in inpatients are shown in Table 1.
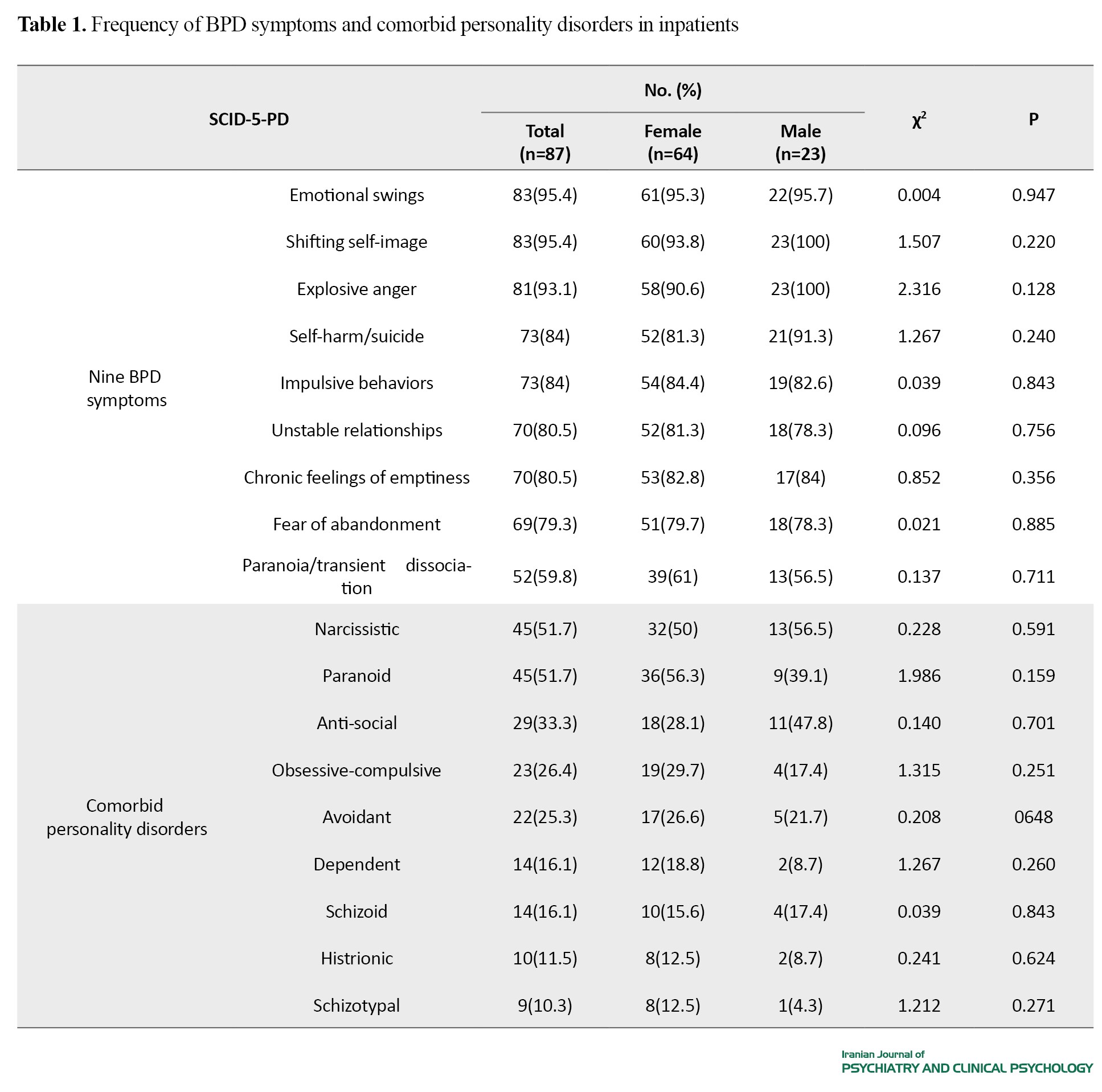
Overall, emotional swings (95.4%), shifting self-image (95.4%), and explosive anger (93.1%) had the highest prevalence, while paranoia/transient dissociation (59.8%) had the lowest prevalence rate. In females, emotional swings (95.3%) had the highest prevalence, while paranoia/transient dissociation (70%) had the lowest prevalence rate. All males (100%) had both shifting self-image and explosive anger, while paranoia/transient dissociation (56.5%) was the least prevalent symptom. Based on the Chi-square test, there was no significant difference in BPD symptoms and comorbid personality disorders between males and females (Table 1). Table 2 shows the mean scores of PID-5 in males and females.
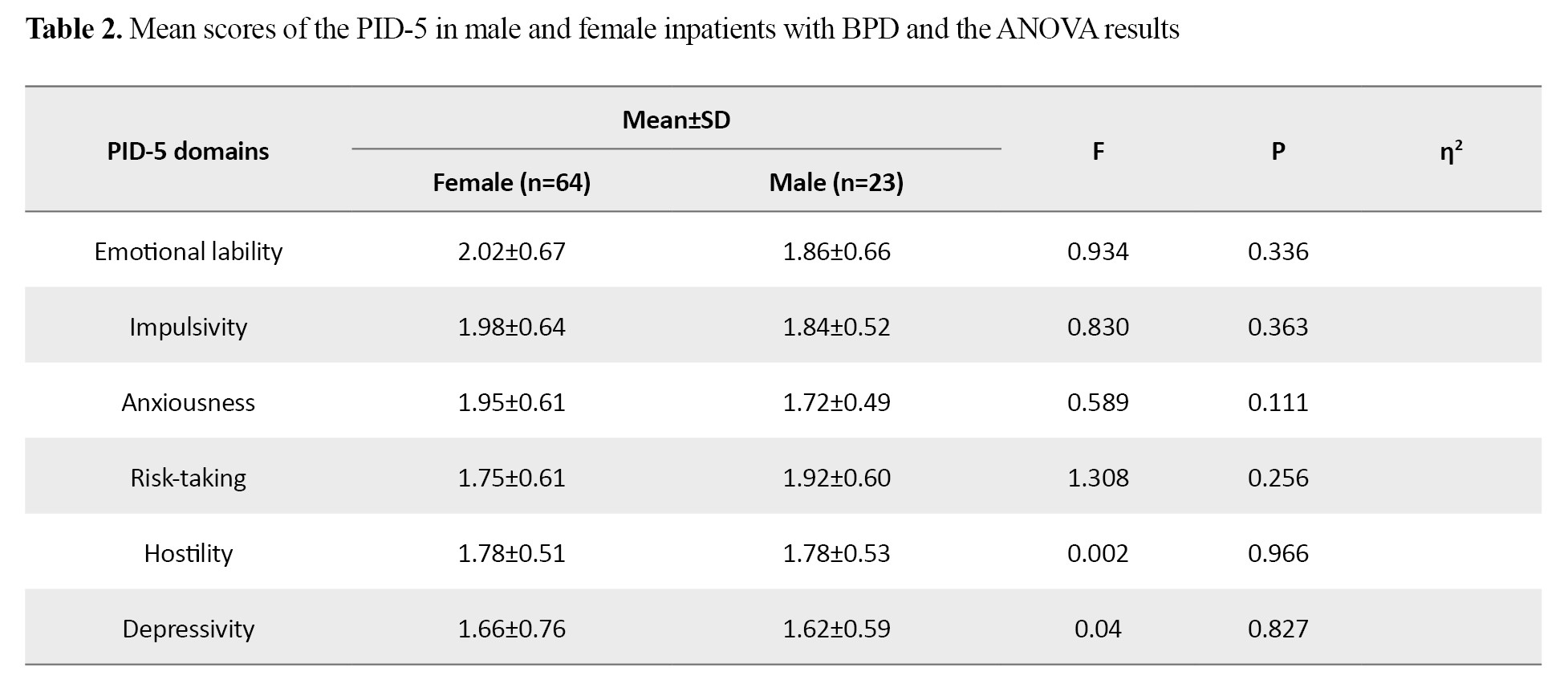
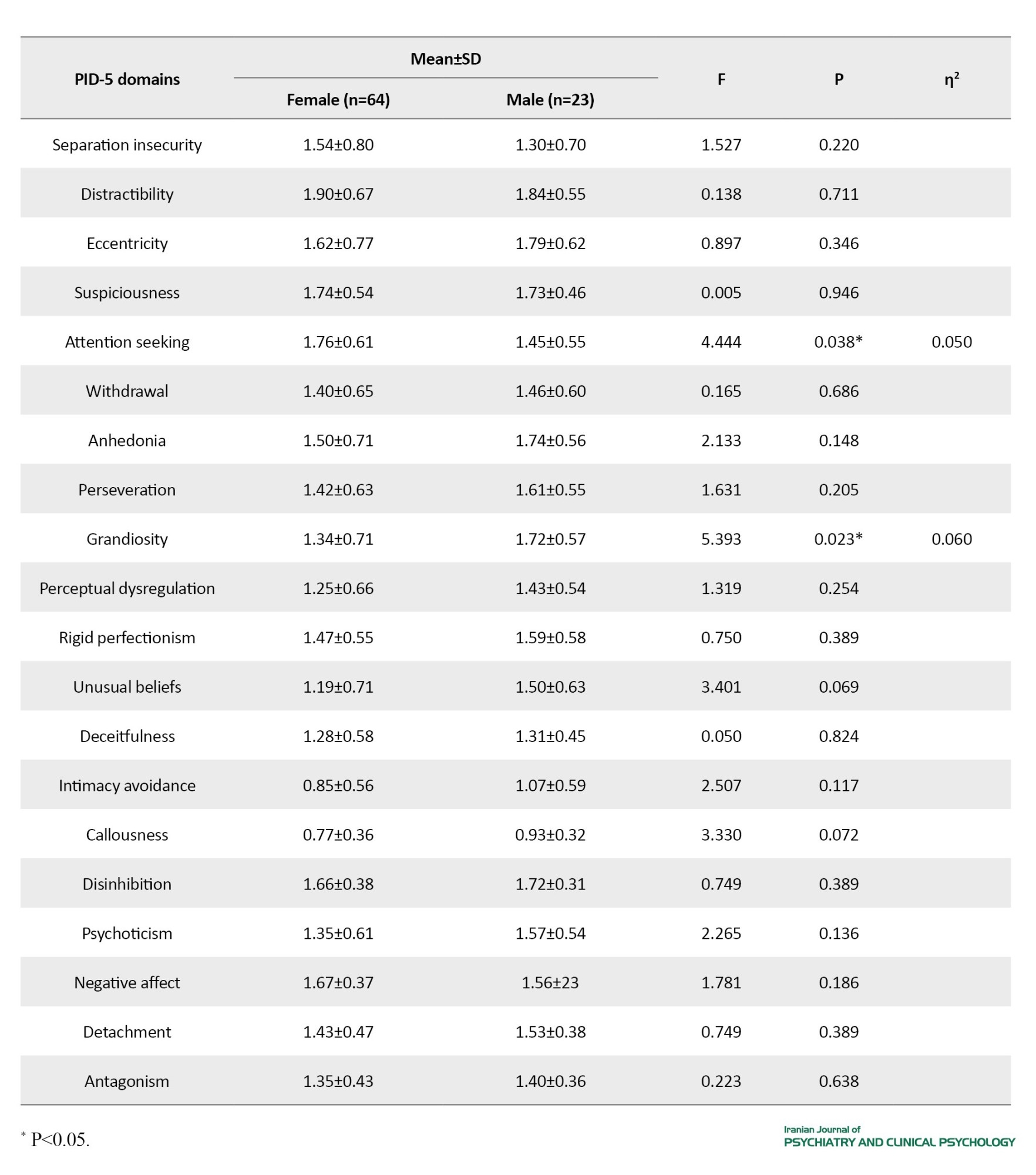
The mean scores of females in attention seeking were significantly higher than that of males, while the scores of males in grandiosity were significantly higher than that of females (P<0.05).
Conclusion
Overall, the results showed that emotional liability, anger, and shifting self-image are the most prominent clinical symptoms in BPD inpatients in Iran. Self-harm/suicide and impulsive behaviors are also prevalent in more than 80% of these inpatients. There is no significant difference between male and female inpatients with BPD in clinical symptoms and comorbid personality disorders. Further studies in Iran are recommended with the participation of outpatients with BPD and investigating the effect of cultural factors on the clinical symptoms of BPD.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR. USWR.RECI1398.049). All participants declared a written informed consent, and their information was kept confidential.
Funding
This article was extracted from the PhD thesis of Maryam Kami at the Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences. This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Abbas Pourshahbaz, Masoud Nosratabadi, and Maryam Kami; Sampling: Maryam Kami, Zahra Dehghanizadeh, and Marzie Olamaie Koopaie; referring the inpatients and supervision: Omid Rezaei , Amir-Abbas Keshavarz-Akhlaghi, and Seyed Shahab Banihashem; Data analysis and writing the initial draft: Maryam Kami; Editing, review, and final approval: All authors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all participants and treatment staff of the Iran Psychiatric Hospital, Taleghani Hospital, and Razi Psychiatric Hospital for their cooperation.
Borderline personality disorder (BPS) is a serious mental disorder that is characterized by instability in self-image, interpersonal relationships, and emotions [1]. The prevalence of this disorder in the general population is estimated to be about 1%, and in psychiatric outpatients and inpatients to be 12 and 22%, respectively [6]. The pathology of this disorder is such that some patients are prone to hospitalization and rehospitalization [15]. The prevalence of suicidal thoughts and attempts among BPD patients have been estimated to be over 60% [16]. About 50% of patients admitted for suicide and self-harm risk management have BPD [17]. Psychotic symptoms, including auditory hallucinations, are another important reason for hospitalization and a risk factor for suicide in some BPD patients [18, 19]. Transient paranoia experienced under stress and characterized by exaggerated beliefs, alongside hearing “voices” (auditory hallucinations), is a psychiatric symptom that predicts hospitalization in BPD patients. Risky and uncontrolled behaviors, including extreme aggression, impulsive sexual activity, and self-medication, can also be reasons for hospitalization in BPD patients [20-22].
Not only the clinical symptoms of BPD inpatients can differ from those of BPD outpatients, but they also differ between male and female patients with BPD, although some studies have not reported any differences between the sexes [24, 25], while there are studies suggesting that emotional instability and interpersonal problems more common in female BPD patients and impulsivity and aggression more common in males [9, 11, 26]. In this study, we aim to investigate the clinical symptoms of BPD in hospitalized patients in Iran, and compare male and female inpatients in clinical symptoms and comorbid personality disorders.
Methods
The study population consists of inpatients admitted to three psychiatric centers in Iran (Iran Psychiatric Hospital, the Neurology Department of Taleghani Hospital, and Razi Psychiatric Hospital). During one year, 120 inpatients were introduced to the research team, of whom 26 inpatients did not meet the diagnostic criteria for BPD, and 7 inpatients were excluded due to incomplete responses to the questionnaires. Finally, data from 87 inpatients (64 females and 23 males) were included in the analysis. The data were collected using the Personality Inventory for DSM-5 (PID-5), the Structured Clinical Interview for DSM-5 Screening Personality Questionnaire, and the Structured Clinical Interview for DSM-5 Personality Disorders. To examine the difference in clinical variables based on sex, the chi-square test was used. To compare men and women in PID-5 scores, the one-way analysis of variance (ANOVA) was used.
Results
The mean age of the inpatients was 27.23±7.31 years. The frequencies of clinical symptoms of BPD and comorbid personality disorders in inpatients are shown in Table 1.
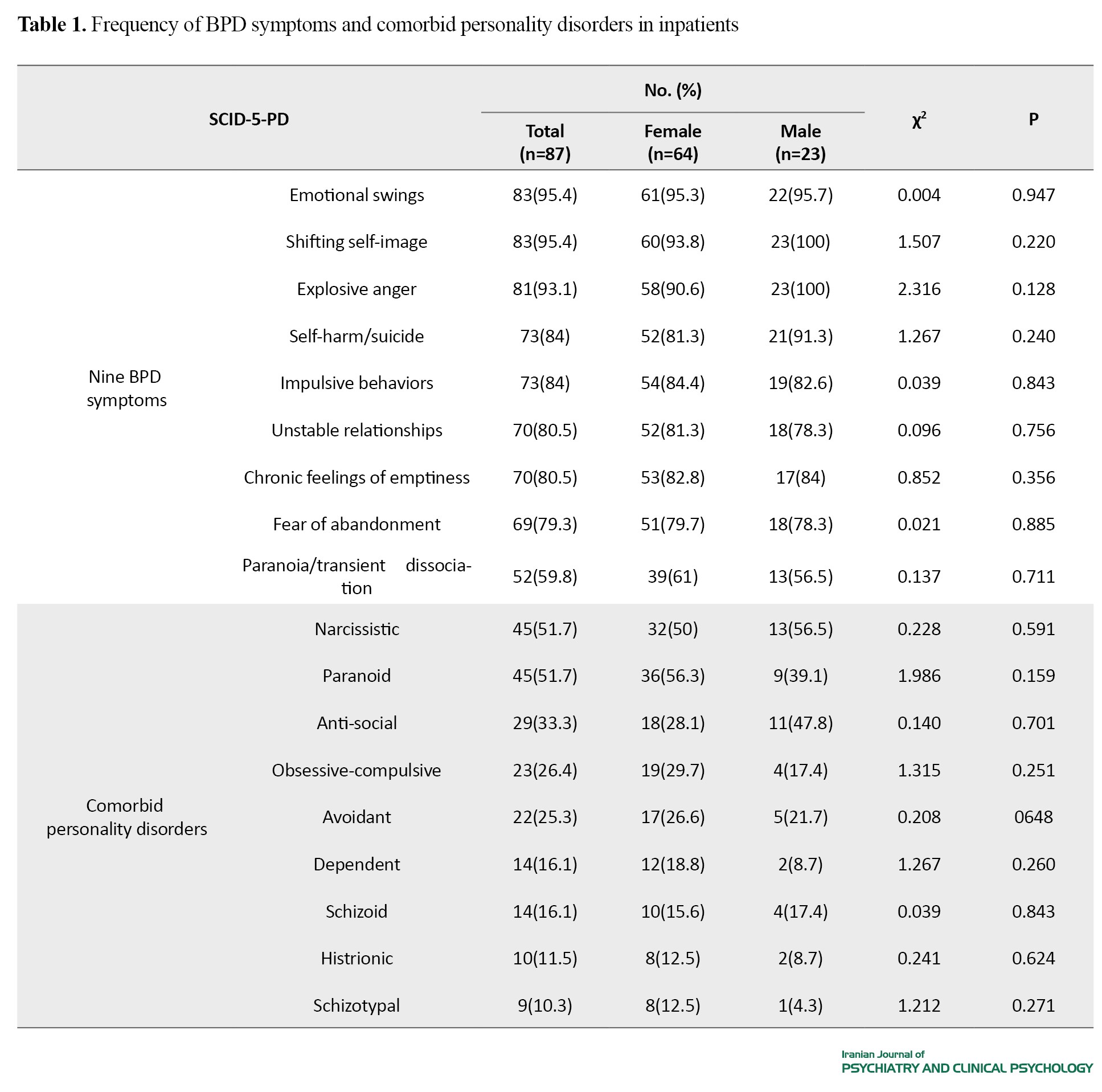
Overall, emotional swings (95.4%), shifting self-image (95.4%), and explosive anger (93.1%) had the highest prevalence, while paranoia/transient dissociation (59.8%) had the lowest prevalence rate. In females, emotional swings (95.3%) had the highest prevalence, while paranoia/transient dissociation (70%) had the lowest prevalence rate. All males (100%) had both shifting self-image and explosive anger, while paranoia/transient dissociation (56.5%) was the least prevalent symptom. Based on the Chi-square test, there was no significant difference in BPD symptoms and comorbid personality disorders between males and females (Table 1). Table 2 shows the mean scores of PID-5 in males and females.
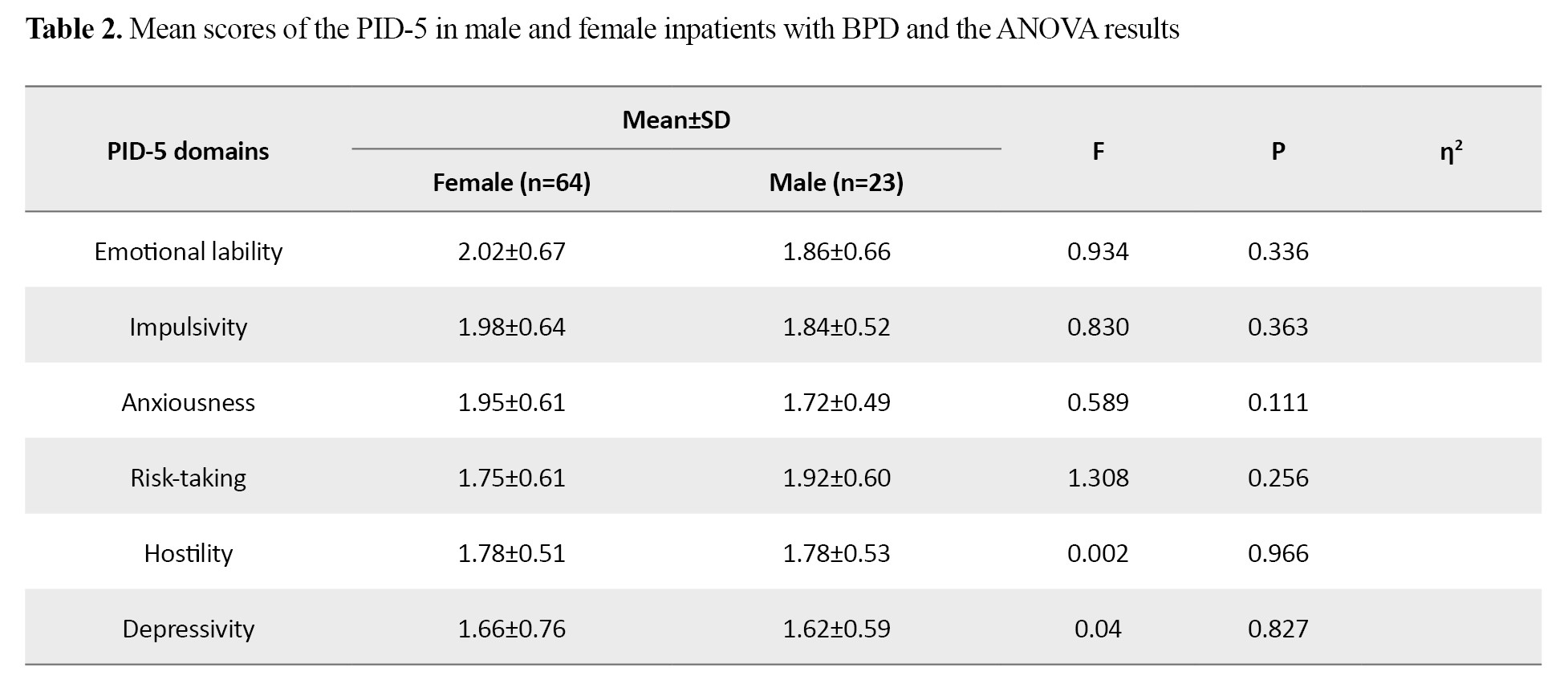
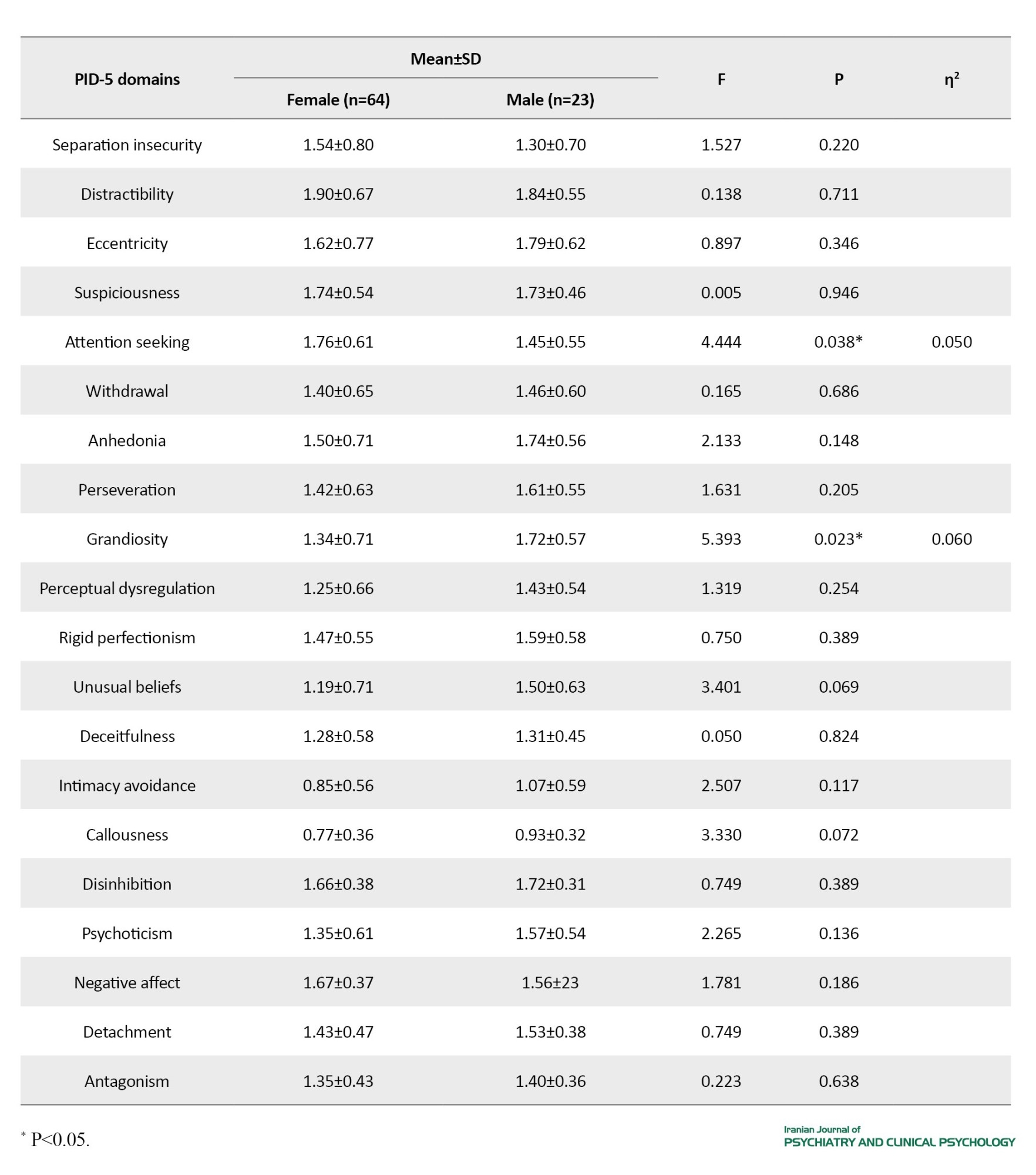
The mean scores of females in attention seeking were significantly higher than that of males, while the scores of males in grandiosity were significantly higher than that of females (P<0.05).
Conclusion
Overall, the results showed that emotional liability, anger, and shifting self-image are the most prominent clinical symptoms in BPD inpatients in Iran. Self-harm/suicide and impulsive behaviors are also prevalent in more than 80% of these inpatients. There is no significant difference between male and female inpatients with BPD in clinical symptoms and comorbid personality disorders. Further studies in Iran are recommended with the participation of outpatients with BPD and investigating the effect of cultural factors on the clinical symptoms of BPD.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran (Code: IR. USWR.RECI1398.049). All participants declared a written informed consent, and their information was kept confidential.
Funding
This article was extracted from the PhD thesis of Maryam Kami at the Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences. This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Abbas Pourshahbaz, Masoud Nosratabadi, and Maryam Kami; Sampling: Maryam Kami, Zahra Dehghanizadeh, and Marzie Olamaie Koopaie; referring the inpatients and supervision: Omid Rezaei , Amir-Abbas Keshavarz-Akhlaghi, and Seyed Shahab Banihashem; Data analysis and writing the initial draft: Maryam Kami; Editing, review, and final approval: All authors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all participants and treatment staff of the Iran Psychiatric Hospital, Taleghani Hospital, and Razi Psychiatric Hospital for their cooperation.
References
- Boland R, Verdiun M, Ruiz P. Kaplan & Sadock’s Synopsis of Psychiatry. Pennsylvania: Wolters Kluwer Health; 2021. [link]
- Ellison WD, Rosenstein LK, Morgan TA, Zimmerman M. Community and clinical epidemiology of borderline personality disorder. Psychiatric Clinics of North America. 2018; 41(4):561-73. [DOI:10.1016/j.psc.2018.07.008] [PMID]
- Mellesdal L, Mehlum L, Wentzel-Larsen T, Kroken R, Jørgensen HA. Suicide risk and acute psychiatric readmissions: A prospective cohort study. Psychiatric Services. 2010; 61(1):25-31. [DOI:10.1176/ps.2010.61.1.25] [PMID]
- Söderholm JJ, Socada JL, Rosenström T, Ekelund J, Isometsä ET. Borderline personality disorder with depression confers significant risk of suicidal behavior in mood disorder patients-a comparative study. Frontiers in Psychiatry. 2020; 11. [DOI:10.3389/fpsyt.2020.00290] [PMID]
- Hayashi N, Igarashi M, Imai A, Osawa Y, Utsumi K, Ishikawa Y, et al. Psychiatric disorders and clinical correlates of suicidal patients admitted to a psychiatric hospital in Tokyo. BMC Psychiatry. 2010; 10:109. [DOI:10.1186/1471-244X-10-109] [PMID]
- Hayward M, Jones AM, Strawson WH, Quadt L, Larsson DEO, Silva M, et al. A cross-sectional study of auditory verbal hallucinations experienced by people with a diagnosis of borderline personality disorder. Clinical Psychology & Psychotherapy. 2022; 29(2):631-41. [DOI:10.1002/cpp.2655] [PMID]
- Slotema CW, Niemantsverdriet MBA, Blom JD, van der Gaag M, Hoek HW, Sommer IE. Suicidality and hospitalisation in patients with borderline personality disorder who experience auditory verbal hallucinations. European Psychiatry. 2017; 41(1):47-52. [DOI:10.1016/j.eurpsy.2016.10.003] [PMID]
- Hong V, Casher MI. The inpatient with borderline personality disorder. In: Casher MI, Bess JD, editors. Manual of Inpatient Psychiatry. 2nd ed. Cambridge: Cambridge University Press; 2020. pp.82-105. [DOI:10.1017/9781108656672.006]
- Juan C, Pascual MD, Córcoles D, Castaño J, Ginés JM, Gurrea A, et al. Hospitalization and pharmacotherapy for borderline personality disorder in a psychiatric emergency service. Psychiatric Services. 2007; 58(9):1199-204. [DOI:10.1176/ps.2007.58.9.1199] [PMID]
- Koehne K, Sands N. Borderline personality disorder-An overview for emergency clinicians. Australasian Emergency Nursing Journal. 2008; 11(4):173-7. [DOI:10.1016/j.aenj.2008.07.003]
- Bloom JM, Woodward EN, Susmaras T, Pantalone DW. Use of dialectical behavior therapy in inpatient treatment of borderline personality disorder: A systematic review. Psychiatric Services. 2012; 63(9):881-8. [DOI:10.1176/appi.ps.201100311] [PMID]
- Casher MI, Bess JD. Manual of Inpatient Psychiatry. Cambridge: Cambridge University Press; 2020. [DOI:10.1017/9781108656672]
- Zlotnick C, Rothschild L, Zimmerman M. The role of gender in the clinical presentation of patients with borderline personality disorder. Journal of Personality Disorders. 2002; 16(3):277-82. [DOI:10.1521/pedi.16.3.277.22540] [PMID]
- Johnson DM, Shea MT, Yen S, Battle CL, Zlotnick C, Sanislow CA, et al. Gender differences in borderline personality disorder: Findings from the Collaborative Longitudinal Personality Disorders Study. Comprehensive Psychiatry. 2003; 44(4):284-92. [DOI:10.1016/S0010-440X(03)00090-7] [PMID]
- Bayes A, Parker G. Borderline personality disorder in men: A literature review and illustrative case vignettes. Psychiatry Research. 2017; 257:197-202. [DOI:10.1016/j.psychres.2017.07.047] [PMID]
- Silberschmidt A, Lee S, Zanarini MC, Schulz SC. Gender differences in borderline personality disorder: Results from a multinational, clinical trial sample. Journal of Personality Disorders. 2015; 29(6):828-38. [DOI:10.1521/pedi_2014_28_175] [PMID]
- Tadić A, Wagner S, Hoch J, Başkaya O, von Cube R, Skaletz C, et al. Gender differences in Axis I and Axis II comorbidity in patients with borderline personality disorder. Psychopathology. 2009; 42(4):257-63. [DOI:10.1159/000224149] [PMID]
- Bozzatello P, Blua C, Brandellero D, Baldassarri L, Brasso C, Rocca P, et al. Gender differences in borderline personality disorder: A narrative review. Frontiers in Psychiatry. 2024; 15:1320546.[DOI:10.3389/fpsyt.2024.1320546] [PMID]
- Sansone RA, Sansone LA. Gender patterns in borderline personality disorder. Innovative Clinical Neuroscience. 2011; 8(5):16-20. [PMID]
- Banzhaf A, Ritter K, Merkl A, Schulte-Herbrüggen O, Lammers CH, Roepke S. Gender differences in a clinical sample of patients with borderline personality disorder. Journal of Personality Disorders. 2012; 26(3):368-80. [DOI:10.1521/pedi.2012.26.3.368] [PMID]
- Dawson DA, Goldstein RB, Moss HB, Li TK, Grant BF. Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: Likelihood, expression and course. Drug and Alcohol Dependence. 2010; 112(1-2):9-17. [DOI:10.1016/j.drugalcdep.2010.04.019] [PMID]
- Nolen-Hoeksema S, Aldao A. Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Personality and Individual Differences. 2011; 51(6):704-8. [DOI:10.1016/j.paid.2011.06.012]
- Deng Y, Chang L, Yang M, Huo M, Zhou R. Gender differences in emotional response: Inconsistency between experience and expressivity. Plos One. 2016; 11(6):e0158666. [DOI:10.1371/journal.pone.0158666] [PMID]
- Barnow S, Herpertz SC, Spitzer C, Stopsack M, Preuss UW, Grabe HJ, et al. Temperament and character in patients with borderline personality disorder taking gender and comorbidity into account. Psychopathology. 2007; 40(6):369-78. [DOI:10.1159/000106467] [PMID]
- Ebrahimi A, Akbarzadeh F, Bimorgh MS, Pirkhaefi A. Investigating the prevalence of personality disorders among psychiatric inpatients and their non-inpatient family members. Journal of Fundamentals of Mental Health. 2023; 25(6):363. [Link]
- Bazrafshan S, Eftekhar Ardebili M, Karimzad N, Nohe Sara S, Ranjbar M, Mohammadsadeghi H. Borderline personality disorder over time: A one-year follow-up study. Journal of Iranian Medical Council. 2019; 2(5):134-42. [Link]
- Sharifi A, Mohammadsadeghi H, Eftekhar Ardebili M, Saeidi M. A cross-sectional study on outcomes of hospitalization in patients with borderline personality disorder after six months. Journal of Iranian Medical Council. 2023; 6(4):695-702. [DOI:10.18502/jimc.v6i4.13450]
- American Psychiatric Association. DSM-5-TR Classification. Washington: American Psychiatric Association Publishing; 2022. [Link]
- Allik J, Realo A. Culture and personality. In: Matsumoto D, Hwang HC, editors. The Handbook of Culture and Psychology. Oxford: Oxford University Press; 2019. [DOI:10.1093/oso/9780190679743.003.0013]
- Neacsiu AD, Eberle W, Keng SL, Fang CM, Rosenthal MZ. Understanding borderline personality disorder across sociocultural groups: Findings, issues, and future directions. Current Psychiatry Reviews. 2017; 13(3):188-223. [DOI:10.2174/1573400513666170612122034]
- Mulder RT. 260 cultural aspects of personality disorder. In: Widiger TA, editor. The Oxford Handbook of Personality Disorders. Oxford: Oxford University Press; 2012. [DOI:10.1093/oxfordhb/9780199735013.013.0013]
- Zimmerman M. Borderline personality disorder: A disorder in search of advocacy. Journal of Nervous and Mental Disease. 2015; 203(1):8-12. [DOI:10.1097/NMD.0000000000000226] [PMID]
- Choudhary S, Gupta R. Culture and borderline personality disorder in India. Frontiers in Psychology. 2020; 11:714. [DOI:10.3389/fpsyg.2020.00714] [PMID]
- Munson KA, Janney CA, Goodwin K, Nagalla M. Cultural representations of borderline personality disorder. Frontiers in Sociology. 2022; 7:832497. [DOI:10.3389/fsoc.2022.832497] [PMID]
- Psychiatry CSo. Chinese Classification of Mental Disorders (CCMD). Jinan: Shandong Science and Technique Press; 2001. [Link]
- Ronningstam EF, Keng SL, Ridolfi ME, Arbabi M, Grenyer BFS. Cultural aspects in symptomatology, assessment, and treatment of personality disorders. Current Psychiatry Reports. 2018; 20(4):22. [DOI:10.1007/s11920-018-0889-8] [PMID]
- Hamedani NG, Purvis TM, Glazer S, Dien J. Ways of manifesting collectivism: An analysis of Iranian and African cultures. 2012. [Link]
- Huang LS, Molenberghs P, Mussap AJ. Cognitive distortions mediate relationships between early maladaptive schemas and aggression in women and men. Aggressive Behavior. 2023; 49(4):418-30. [DOI:10.1002/ab.22083] [PMID]
- Young JE, Klosko JS, Weishaar ME. Schema Therapy: A Practitioner’s Guide. New York, NY: Guilford Press; 2006. [Link]
- Naing L, Winn T, Nordin R. Practical issues in calculating the sample size for prevalence studies. Archives of Orofacial Sciences. 2006; 1:9-14. [Link]
- Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian Journal of Psychological Medicine. 2013; 35(2):121-6. [DOI:10.4103/0253-7176.116232] [PMID]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington: American Psychiatric Publishing; 2013. [Link]
- Al-Dajani N, Gralnick TM, Bagby RM. A psychometric review of the Personality Inventory for DSM-5 (PID-5): Current status and future directions. Journal of Personality Assessment. 2016; 98(1):62-81. [DOI:10.1080/00223891.2015.1107572] [PMID]
- Shojaei Z, Mohammadi A, Zarei M. Psychometric properties of the Persian version of Personality Inventory for DSM-5 (PID-5) in psychiatric patients. Iranian Journal of Psychiatry and Behavioral Sciences. 2020; 14(4): e87974. [DOI:10.5812/ijpbs.87974]
- First MB, Williams JB, Benjamin LS, Spitzer RL. User’s Guide for the Structured Clinical Interview for DSM-5 Personality Disorders (SCID-5-PD). Washington: American Psychiatric Association Publishing; 2015. [Link]
- Somma A, Borroni S, Gialdi G, Carlotta D, Giarolli LE, Barranca M, et al. The inter-rater reliability and validity of the Italian translation of the Structured Clinical Interview for DSM-5 Alternative Model for Personality Disorders Module I and Module II: A preliminary report on consecutively admitted psychotherapy outpatients. Journal of Personality Disorders. 2020; 34(Suppl C):95-123. [DOI:10.1521/pedi_2020_34_511] [PMID]
- Gharrae B, Masoumian S, Zamirinejad S, Yaghmaeezadeh H. Psychometric properties of the Persian version of the Self-report Personality Questionnaire for Personality Disorders of DSM-5 (SCID-5-SPQ) in clinical samples. Iranian Journal of Psychiatry and Clinical Psychology. 2022; 27(4):508-19. [DOI:10.32598/ijpcp.27.4.2497.3]
- Ghamkhar Fard Z, Pourshahbaz A, Anderson JL, Boland JK, Shakiba S, Mirabzadeh A. The continuity between DSM-5 criterion-based and trait-based models for personality disorders in an Iranian community sample. Current Psychology. 2021; [DOI:10.1007/s12144-021-01751-2]
- Bayad S, Alp-Topbaş Ö, Kocabaş T, Elbir M, Gökten-Ulusoy D, Korkmaz U, et al. Adaptation and the psychometric properties of Turkish version of the Structured Clinical Interview for the DSM-5-Personality Disorders-Clinician Version (SCID-5-PD/CV). Turkish Journal of Psychiatry. 2021; 32(4):267-74. [DOI:10.5080/u25484] [PMID]
- Gharraee B, Shabani A, Masoumian S, Zamirinejad S, Yaghmaeezadeh H, Khanjani S, et al. Psychometric properties of Persian version of Structured Clinical Interview for DSM-5 for Personality Disorders. East Asian Archives of Psychiatry. 2022; 32(4):95-9. [DOI:10.12809/eaap2208] [PMID]
- Cano K, Sumlin E, Sharp C. Screening for borderline personality pathology on college campuses. Personality and Mental Health. 2022; 16(3):235-43. [DOI:10.1002/pmh.1534] [PMID]
- Ikuta N, Zanarini MC, Minakawa K, Miyake Y, Moriya N, Nishizono-Maher A. Comparison of American and Japanese outpatients with borderline personality disorder. Comprehensive Psychiatry. 1994; 35(5):382-5. [DOI:10.1016/0010-440X(94)90279-8] [PMID]
- Moriya N, Miyake Y, Minakawa K, Ikuta N, Nishizono-Maher A. Diagnosis and clinical features of borderline personality disorder in the east and west: A preliminary report. Comprehensive Psychiatry. 1993; 34(6):418-23. [DOI:10.1016/0010-440X(93)90069-G] [PMID]
- Wright-Hughes A, Graham E, Farrin A, Collinson M, Boston P, Eisler I, et al. Self-Harm Intervention: Family Therapy (SHIFT), a study protocol for a randomised controlled trial of family therapy versus treatment as usual for young people seen after a second or subsequent episode of self-harm. Trials. 2015; 16(1):501. [DOI:10.1186/s13063-015-1007-4] [PMID]
- Buckmaster R, McNulty M, Guerin S. Family factors associated with self-harm in adults: A systematic review. Journal of Family Therapy. 2019; 41(4):537-58. [DOI:10.1111/1467-6427.12232]
- Plutchik R. Outward and inward directed aggressiveness: The interaction between violence and suicidality. Pharmacopsychiatry. 1995; 28(Suppl 2):47-57. [DOI:10.1055/s-2007-979620] [PMID]
- Shafti M, Taylor PJ, Forrester A, Pratt D. The co-occurrence of self-harm and aggression: A cognitive-emotional model of dual-harm. Frontiers in Psychology. 2021; 12:586135. [DOI:10.3389/fpsyg.2021.586135] [PMID]
- Fossati A, Somma A, Borroni S, Maffei C, Markon KE, Krueger RF. Borderline personality disorder and narcissistic personality disorder diagnoses from the perspective of the DSM-5 personality traits: A study on Italian clinical participants. Journal of Nervous and Mental Disease. 2016; 204(12):939-49. [DOI:10.1097/NMD.0000000000000587] [PMID]
- Bach B, Sellbom M, Bo S, Simonsen E. Utility of DSM-5 section III personality traits in differentiating borderline personality disorder from comparison groups. European Psychiatry. 2016; 37:22-7. [DOI:10.1016/j.eurpsy.2016.04.006] [PMID]
- Calvo N, Valero S, Sáez-Francàs N, Gutiérrez F, Casas M, Ferrer M. Borderline personality disorder and Personality Inventory for DSM-5 (PID-5): Dimensional personality assessment with DSM-5. Comprehensive Psychiatry. 2016; 70:105-11. [DOI:10.1016/j.comppsych.2016.07.002] [PMID]
- Palomares N, McMaster A, Díaz-Marsá M, de la Vega I, Montes A, Carrasco JL. Multiple cluster Axis II comorbidity and functional outcome in severe patients with borderline personality disorder. Actas Españolas de Psiquiatría. 2016; 44(6):212-21.
- Barrachina J, Pascual JC, Ferrer M, Soler J, Rufat MJ, Andión O, et al. Axis II comorbidity in borderline personality disorder is influenced by sex, age, and clinical severity. Comprehensive Psychiatry. 2011; 52(6):725-30. [DOI:10.1016/j.comppsych.2010.11.009] [PMID]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis II comorbidity of borderline personality disorder. Comprehensive Psychiatry. 1998; 39(5):296-302. [DOI:10.1016/S0010-440X(98)90038-4] [PMID]
- Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich DB, Silk KR. Axis II comorbidity of borderline personality disorder: Description of 6-year course and prediction to time-to-remission. Acta Psychiatrica Scandinavica. 2004; 110(6):416-20. [DOI:10.1111/j.1600-0447.2004.00362.x] [PMID]
- Sher L, Fisher AM, Kelliher CH, Penner JD, Goodman M, Koenigsberg HW, et al. Clinical features and psychiatric comorbidities of borderline personality disorder patients with versus without a history of suicide attempt. Psychiatry Research. 2016; 246:261-6. [DOI:10.1016/j.psychres.2016.10.003] [PMID]
- Stone LE, Segal DL, Krus GC. Relationships between pathological narcissism and maladaptive personality traits among older adults. Aging & Mental Health. 2021; 25(5):930-5. [DOI:10.1080/13607863.2020.1725802] [PMID]
- Millon T, Millon CM, Meagher SE, Grossman SD, Ramnath R. Personality disorders in modern life. New Jersey: Wiley; 2012. [Link]
- Sękowski M, Gambin M, Sumlin E, Sharp C. Associations between symptoms of borderline personality disorder and suicidality in inpatient adolescents: The significance of identity disturbance. Psychiatry Research. 2022; 312:114558. [DOI:10.1016/j.psychres.2022.114558] [PMID]
- Sher L, Rutter SB, New AS, Siever LJ, Hazlett EA. Gender differences and similarities in aggression, suicidal behaviour, and psychiatric comorbidity in borderline personality disorder. Acta Psychiatrica Scandinavica. 2019; 139(2):145-53. [DOI:10.1111/acps.12981] [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/04/24 | Accepted: 2024/10/29 | Published: 2024/07/31
Received: 2024/04/24 | Accepted: 2024/10/29 | Published: 2024/07/31
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |