Tue, Jul 1, 2025
| فارسی
Volume 30, Issue 1 (Continuously Updated 2024)
IJPCP 2024, 30(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sobhani S, Fathali Lavasani F, Moniri R, Farahani H, Samadi A. Validity and Reliability of the Persian Version of the Adaptive Coping with Disease (AKU) Questionnaire for Iranian Patients with Chronic Diseases. IJPCP 2024; 30 (1) : 2152.2
URL: http://ijpcp.iums.ac.ir/article-1-4116-en.html
URL: http://ijpcp.iums.ac.ir/article-1-4116-en.html
Sara Sobhani1 

 , Fahimeh Fathali Lavasani2
, Fahimeh Fathali Lavasani2 

 , Reihaneh Moniri1
, Reihaneh Moniri1 

 , Hojjatollah Farahani3
, Hojjatollah Farahani3 

 , Arezoo Samadi4
, Arezoo Samadi4 




 , Fahimeh Fathali Lavasani2
, Fahimeh Fathali Lavasani2 

 , Reihaneh Moniri1
, Reihaneh Moniri1 

 , Hojjatollah Farahani3
, Hojjatollah Farahani3 

 , Arezoo Samadi4
, Arezoo Samadi4 


1- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Science, Tehran, Iran.
2- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Science, Tehran, Iran. ,lavasani.f@iums.ac.ir
3- Department of Psychology, Faculty of Humanities, Tarbiat Modares University, Tehran, Iran.
4- Psychiatrist, Fellowship of Psychosomatic Medicine, Faculty of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Science, Tehran, Iran. ,
3- Department of Psychology, Faculty of Humanities, Tarbiat Modares University, Tehran, Iran.
4- Psychiatrist, Fellowship of Psychosomatic Medicine, Faculty of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 6636 kb]
(523 Downloads)
| Abstract (HTML) (1476 Views)
Full-Text: (471 Views)
Introduction
Chronic diseases put high pressure on patients, families, and society [1، 2]. According to the World Health Organization, nearly one in three adults globally suffers from multiple chronic diseases [3]. These diseases have negative impact on various aspects of life, including physical, emotional, and social aspects [4-7]. Challenges with managing chronic diseases lead to losing self-esteem in patients, and make them vulnerable to mental health problems such as depression and anxiety, as well as fatigue and decreased quality of life [3, 8-11]. When there is no specific treatment for chronic diseases, patients need to improve coping strategies to enhance their quality of life. According to studies, coping strategies have two types of adaptive and maladaptive. Adaptive coping is associated with a decrease in psychological distress [9], while maladaptive coping is associated with psychological pressure and impaired function [9, 12]. The Adaptive Coping with Disease (AKU) questionnaire was designed by Bussing et al. [13] to identify adaptive coping strategies for chronic diseases. This study aims to assess the psychometric properties of the Persian version of the AKU questionnaire for Iranian patients with chronic diseases.
Methods
After translating, the questionnaire was completed by 477 patients with chronic diseases referred to medical centers in Tehran, Iran in 2022. To determine convergent validity, 153 participants also completed Lazarus’ ways of coping questionnaire (WCQ) and the 36-item short form health survey (SF-36) questionnaires. The internal consistency was assessed using Cronbach’s alpha coefficient. Construct validity was evaluated using the confirmatory factor analysis (CFA), the calculation of the Average Variance Extracted (AVE) and Composite Reliability (CR) indices.
Results
The average age of participants was 39 years (SD=13.43). The results of CFA to evaluate construct validity are presented in Table 1.
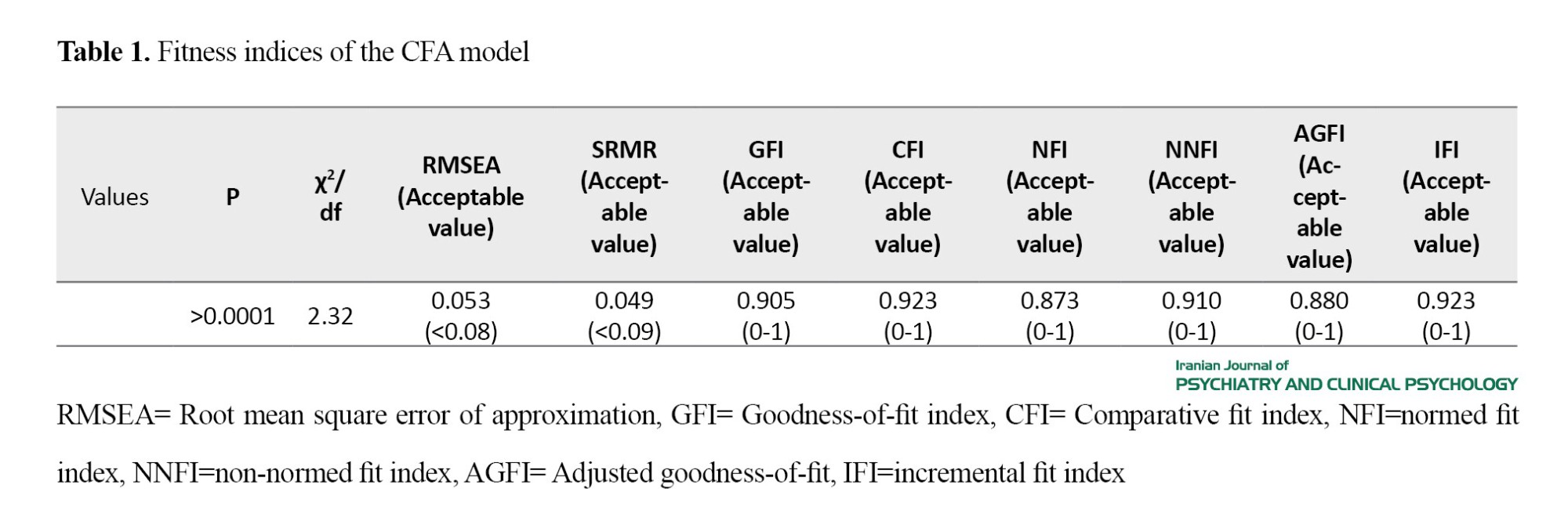
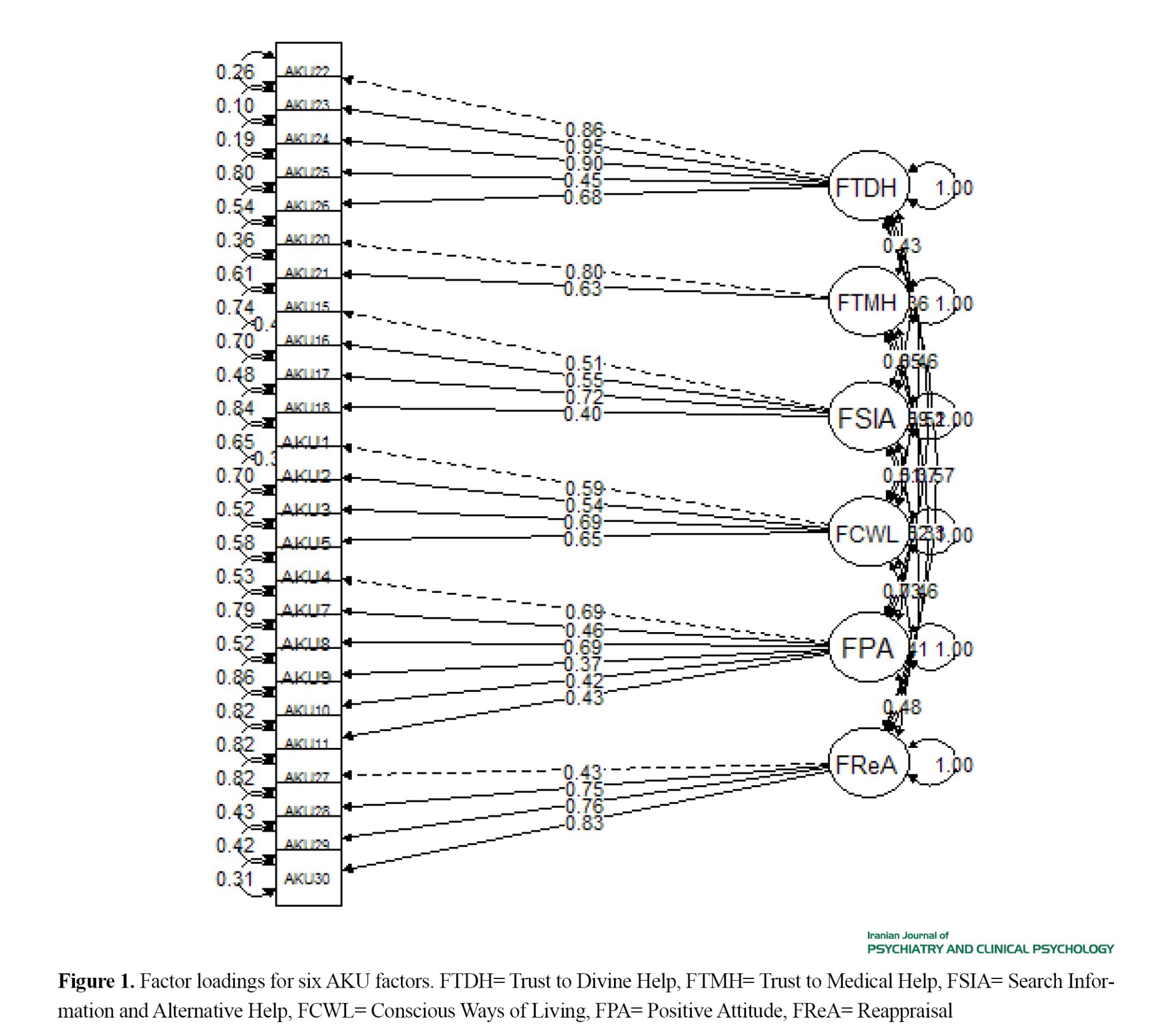
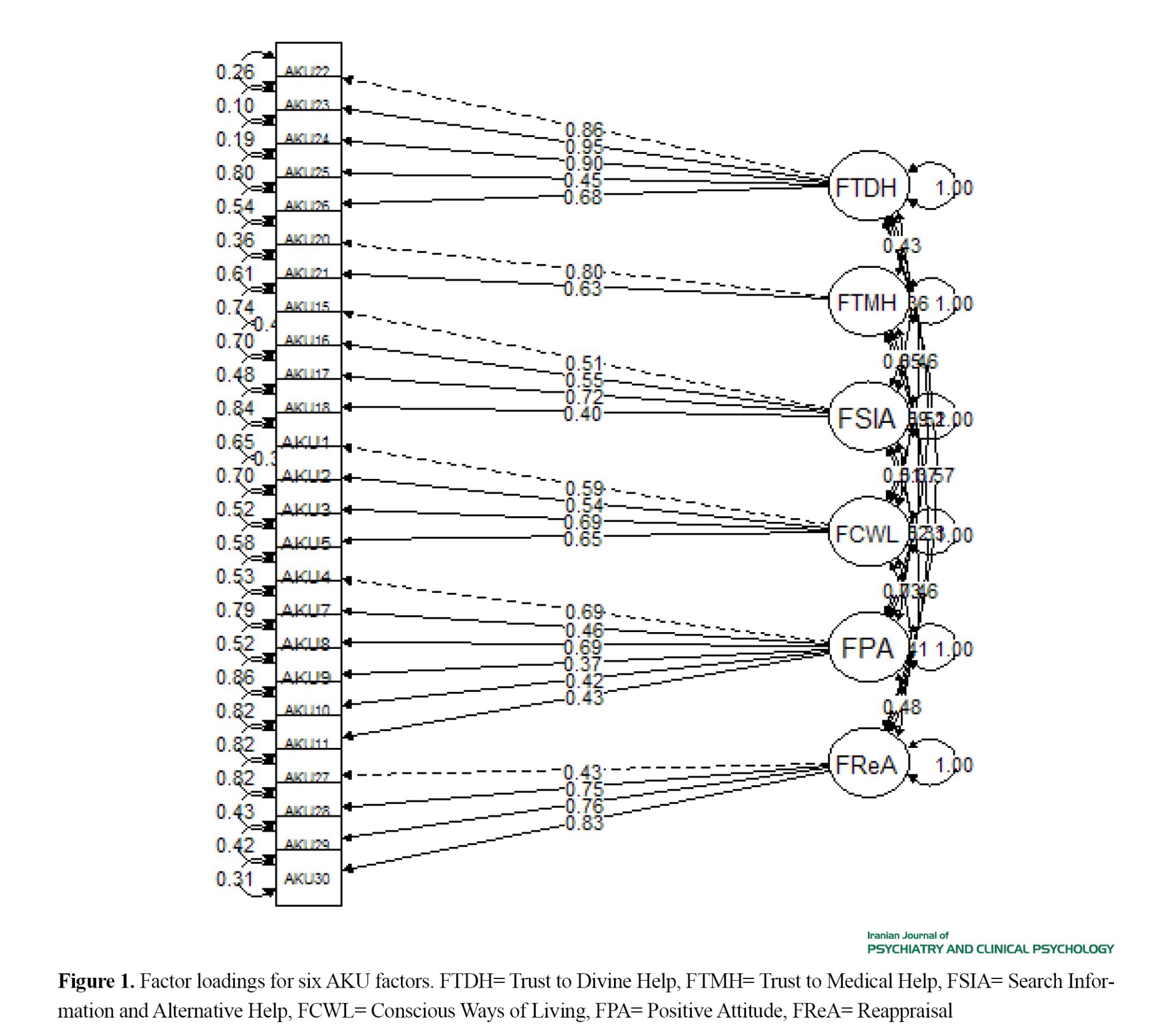
The results of CFA confirmed the 6-factor structure of the Persian AKU questionnaire, but two items (6 and 19) were removed due to non-significant factor loadings (Figure 1).
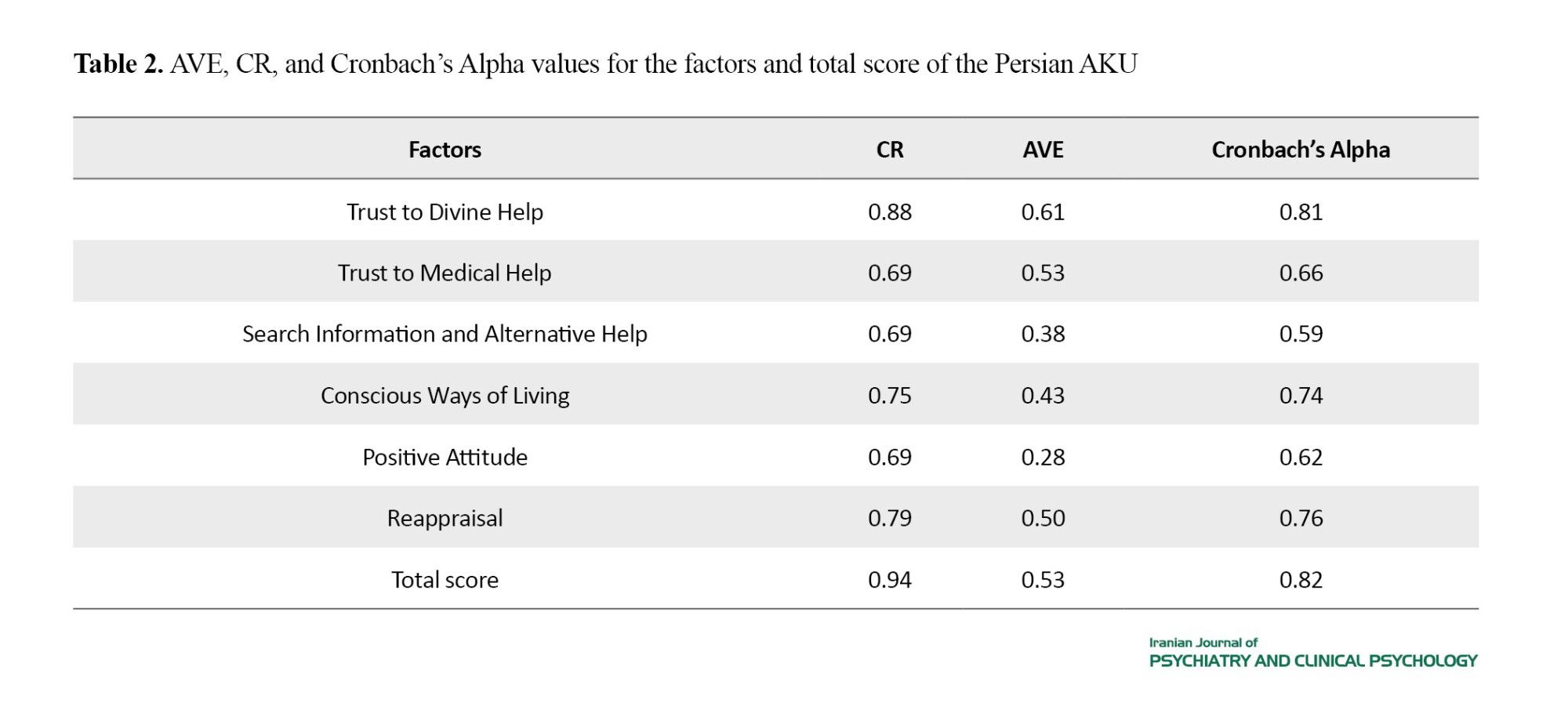
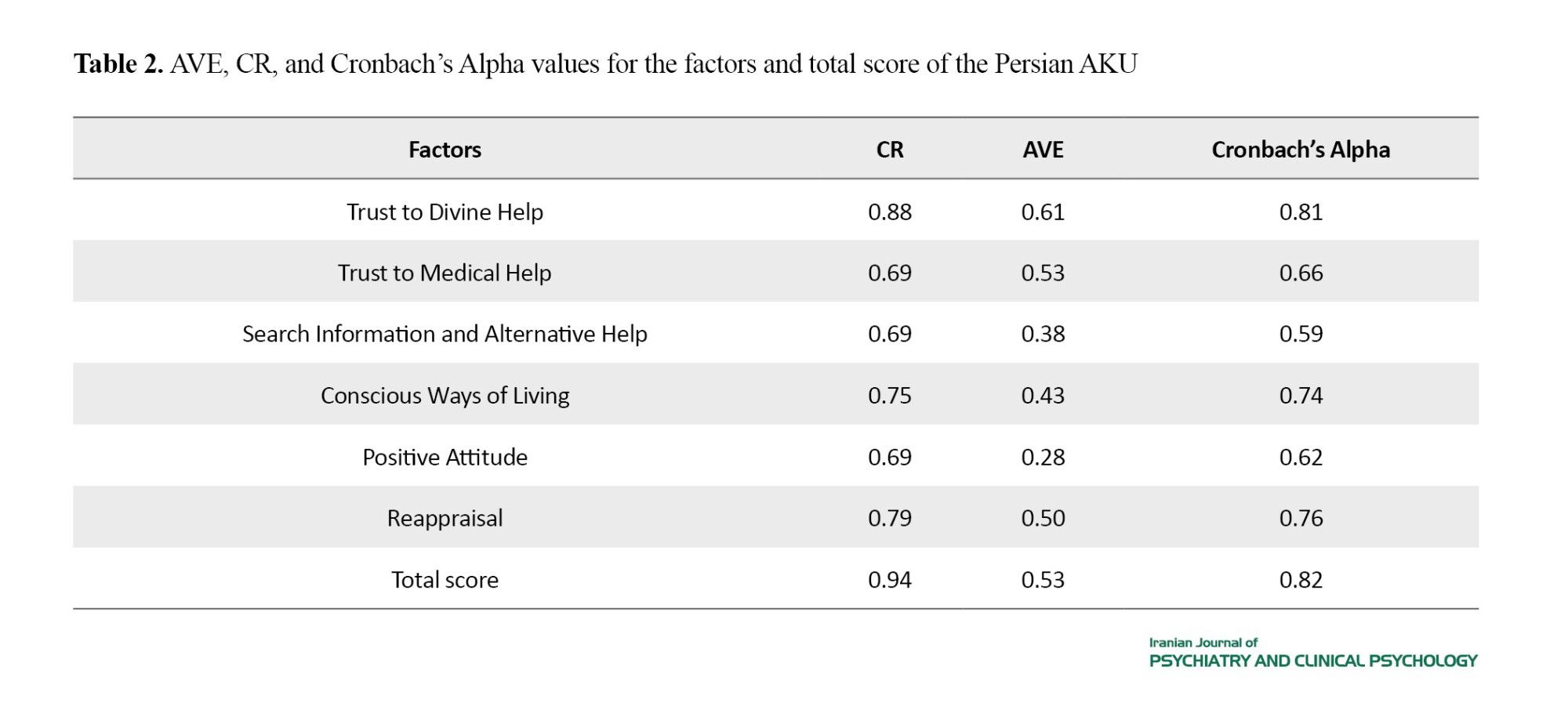
The Persian AKU questionnaire demonstrated good internal consistency (α> 0.7), and acceptable composite reliability (CR>0.7) (Table 2). The Persian AKU scores exhibited significant correlations with the emotion-focused and problem-focused coping subscales of the WCQ (r=1 and 0.92, respectively; P<0.001), and with the physical health and mental health dimensions of the SF-36 (r=0.27 and 0.39, respectively; P<0.001), indicating good convergent validity.
Conclusion
This study confirmed the validity and reliability of the Persian AKU questionnaire for Iranian patients with chronic diseases. It has good internal consistency and the CFA supported the 6-factor structure of the questionnaire, consistent with results of Bussing et al. [13,14]. However, two items (6 and 19) were removed. Considering the importance of the Item 19, it is recommended to exclude it only for diseases that do not require medication. An important finding of this study was the positive and significant correlation between the total AKU score and both emotion-focused and problem-focused coping domains of the WCQ. Existing research on coping styles has reported the link between emotion-focused coping strategies and reduced levels of adaptation and health-related quality of life [15]. However, our finding is against these results. For adaptation to chronic diseases, both emotion- and problem-focused coping strategies are needed. These strategies include therapeutic procedures to improve or control symptoms (problem-focused), as well as religious or spiritual coping strategies (emotion-focused) that help patients to accept challenging conditions caused by the disease and increase their tolerance levels [5, 13, 16]. Thus, problem-focused and emotion-focused strategies, when applied in the appropriate context, are both adaptive coping mechanisms. This finding is consistent with existing literature on the importance of emotion-focused strategies for chronic diseases [5, 17, 18].
The AKU score also showed a significant positive correlation with the physical and mental health domains of the SF-36, albeit it was at a weak to moderate level. This finding is consistent with the study by Bussing et al., who also reported a weak positive correlation between the AKU score and physical and mental health domains of the SF-12 [7]. It should be noted that, regardless of the extent to which people use adaptive coping strategies, a significant part of a person’s quality of life, especially in the physical aspect, is out of the person’s complete control, considering that there is no possibility of complete recovery, and is affected by the nature, severity, and course of the disease, and makes a person inevitably change her/his living conditions in line with her/his physical condition. Consequently, the person has to face a change in role and function in different areas of life and accept and adapt to it.
One of the strengths of this study was the relatively large sample size with a wide range of chronic diseases and age ranges. However, the results cannot be generalized to all patients in Iran. In the current study, participants included both patients requiring medication and those without such interventions. Therefore, the exclusion of the item 19, which is related to medication use and is a crucial item, may pose challenges. It is recommended that future studies investigate this issue again in patients with and without pharmacotherapy.
Ethical Considerations
Compliance with ethical guidelines
The research protocol was approved by the ethics committee of Iran University of Medical Sciences (code: IR.IUMS.REC.1399.950).
Funding
This study was funded by the Mental Health Research Center, Psychosocial Health Research Institute, Iran University of Medical Sciences.
Authors contributions
Conceptualization, methodology, validation: Sara Sobhani, Fahimeh Fathali Lavasani and Hojjatollah Farahani; Project administration: Sara Sobhani, Reihaneh Moniri and Arezoo Samadi; Formal analysis: Hojjatollah Farahani; Supervision: Fahimeh Fathali Lavasani; Investigation, writing – original draft: Sara Sobhani; Review & Editing: All authors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all the patients participated in this study as well as the personnel of Rasool-e Akram Hospital, Firouzgar Hospital, and Abadis Spine Clinic for their cooperation in the study. The authors also thank the Mental Health Research Center, Psychosocial Health Research Institute, Iran University of Medical Sciences for their financial support.
Chronic diseases put high pressure on patients, families, and society [1، 2]. According to the World Health Organization, nearly one in three adults globally suffers from multiple chronic diseases [3]. These diseases have negative impact on various aspects of life, including physical, emotional, and social aspects [4-7]. Challenges with managing chronic diseases lead to losing self-esteem in patients, and make them vulnerable to mental health problems such as depression and anxiety, as well as fatigue and decreased quality of life [3, 8-11]. When there is no specific treatment for chronic diseases, patients need to improve coping strategies to enhance their quality of life. According to studies, coping strategies have two types of adaptive and maladaptive. Adaptive coping is associated with a decrease in psychological distress [9], while maladaptive coping is associated with psychological pressure and impaired function [9, 12]. The Adaptive Coping with Disease (AKU) questionnaire was designed by Bussing et al. [13] to identify adaptive coping strategies for chronic diseases. This study aims to assess the psychometric properties of the Persian version of the AKU questionnaire for Iranian patients with chronic diseases.
Methods
After translating, the questionnaire was completed by 477 patients with chronic diseases referred to medical centers in Tehran, Iran in 2022. To determine convergent validity, 153 participants also completed Lazarus’ ways of coping questionnaire (WCQ) and the 36-item short form health survey (SF-36) questionnaires. The internal consistency was assessed using Cronbach’s alpha coefficient. Construct validity was evaluated using the confirmatory factor analysis (CFA), the calculation of the Average Variance Extracted (AVE) and Composite Reliability (CR) indices.
Results
The average age of participants was 39 years (SD=13.43). The results of CFA to evaluate construct validity are presented in Table 1.
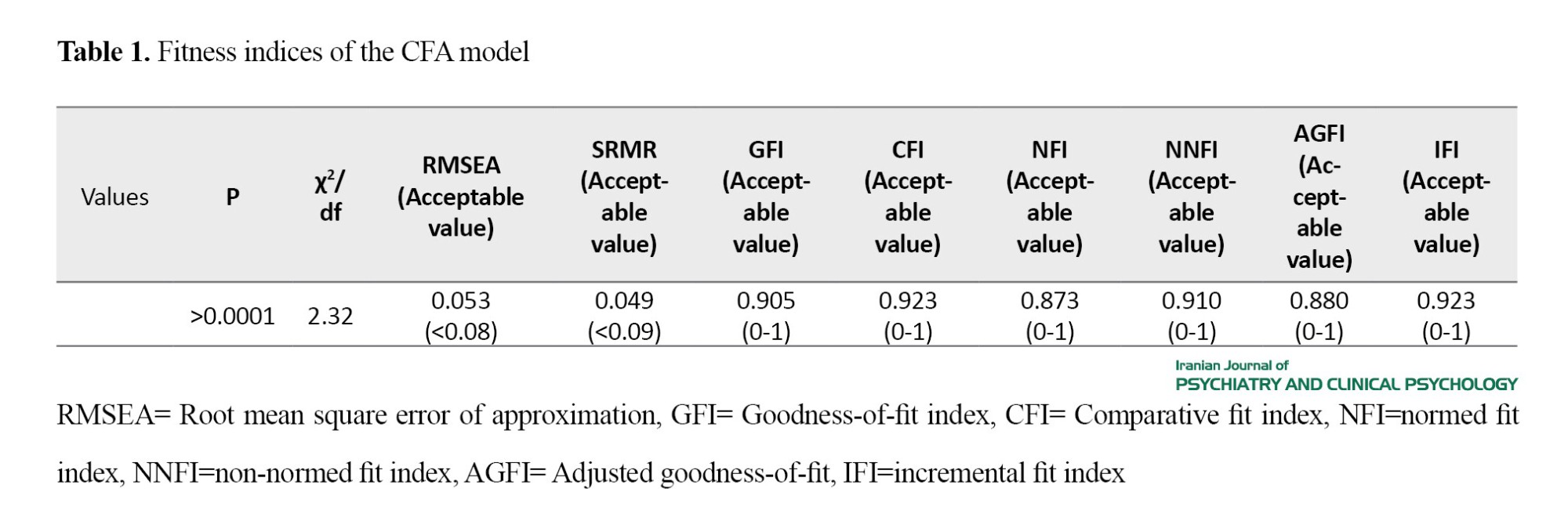
The results of CFA confirmed the 6-factor structure of the Persian AKU questionnaire, but two items (6 and 19) were removed due to non-significant factor loadings (Figure 1).
The Persian AKU questionnaire demonstrated good internal consistency (α> 0.7), and acceptable composite reliability (CR>0.7) (Table 2). The Persian AKU scores exhibited significant correlations with the emotion-focused and problem-focused coping subscales of the WCQ (r=1 and 0.92, respectively; P<0.001), and with the physical health and mental health dimensions of the SF-36 (r=0.27 and 0.39, respectively; P<0.001), indicating good convergent validity.
Conclusion
This study confirmed the validity and reliability of the Persian AKU questionnaire for Iranian patients with chronic diseases. It has good internal consistency and the CFA supported the 6-factor structure of the questionnaire, consistent with results of Bussing et al. [13,14]. However, two items (6 and 19) were removed. Considering the importance of the Item 19, it is recommended to exclude it only for diseases that do not require medication. An important finding of this study was the positive and significant correlation between the total AKU score and both emotion-focused and problem-focused coping domains of the WCQ. Existing research on coping styles has reported the link between emotion-focused coping strategies and reduced levels of adaptation and health-related quality of life [15]. However, our finding is against these results. For adaptation to chronic diseases, both emotion- and problem-focused coping strategies are needed. These strategies include therapeutic procedures to improve or control symptoms (problem-focused), as well as religious or spiritual coping strategies (emotion-focused) that help patients to accept challenging conditions caused by the disease and increase their tolerance levels [5, 13, 16]. Thus, problem-focused and emotion-focused strategies, when applied in the appropriate context, are both adaptive coping mechanisms. This finding is consistent with existing literature on the importance of emotion-focused strategies for chronic diseases [5, 17, 18].
The AKU score also showed a significant positive correlation with the physical and mental health domains of the SF-36, albeit it was at a weak to moderate level. This finding is consistent with the study by Bussing et al., who also reported a weak positive correlation between the AKU score and physical and mental health domains of the SF-12 [7]. It should be noted that, regardless of the extent to which people use adaptive coping strategies, a significant part of a person’s quality of life, especially in the physical aspect, is out of the person’s complete control, considering that there is no possibility of complete recovery, and is affected by the nature, severity, and course of the disease, and makes a person inevitably change her/his living conditions in line with her/his physical condition. Consequently, the person has to face a change in role and function in different areas of life and accept and adapt to it.
One of the strengths of this study was the relatively large sample size with a wide range of chronic diseases and age ranges. However, the results cannot be generalized to all patients in Iran. In the current study, participants included both patients requiring medication and those without such interventions. Therefore, the exclusion of the item 19, which is related to medication use and is a crucial item, may pose challenges. It is recommended that future studies investigate this issue again in patients with and without pharmacotherapy.
Ethical Considerations
Compliance with ethical guidelines
The research protocol was approved by the ethics committee of Iran University of Medical Sciences (code: IR.IUMS.REC.1399.950).
Funding
This study was funded by the Mental Health Research Center, Psychosocial Health Research Institute, Iran University of Medical Sciences.
Authors contributions
Conceptualization, methodology, validation: Sara Sobhani, Fahimeh Fathali Lavasani and Hojjatollah Farahani; Project administration: Sara Sobhani, Reihaneh Moniri and Arezoo Samadi; Formal analysis: Hojjatollah Farahani; Supervision: Fahimeh Fathali Lavasani; Investigation, writing – original draft: Sara Sobhani; Review & Editing: All authors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank all the patients participated in this study as well as the personnel of Rasool-e Akram Hospital, Firouzgar Hospital, and Abadis Spine Clinic for their cooperation in the study. The authors also thank the Mental Health Research Center, Psychosocial Health Research Institute, Iran University of Medical Sciences for their financial support.
References
- Dennison L, Moss-Morris R, Silber E, Galea I, Chalder T. Cognitive and behavioural correlates of different domains of psychological adjustment in early-stage multiple sclerosis. Journal of Psychosomatic Research. 2010; 69(4):353-61. [DOI:10.1016/j.jpsychores.2010.04.009] [PMID]
- Finkelstein-Fox L, Park CL. Control-coping goodness-of-fit and chronic illness: A systematic review of the literature. Health Psychology Review. 2019; 13(2):137-62. [DOI:10.1080/17437199.2018.1560229] [PMID]
- Hajat C, Stein E. The global burden of multiple chronic conditions: A narrative review. Preventive Medicine Reports. 2018; 12:284-93. [DOI:10.1016/j.pmedr.2018.10.008] [PMID]
- Maguire R, Hanly P, Maguire P. Living well with chronic illness: How social support, loneliness and psychological appraisals relate to well-being in a population-based European sample. Journal of Health Psychology. 2021; 26(10):1494-507. [DOI:10.1177/1359105319883923] [PMID]
- World Health Organization. Noncommunicable diseases country profiles 2018. Geneva: World Health Organization; 2018. [Link]
- Sandison B. Australian Institute of health and welfare. Impact. 2018; 2018(2):80-1. [DOI:10.21820/23987073.2018.2.80]
- Temkin SM, Barr E, Moore H, Caviston JP, Regensteiner JG, Clayton JA. Chronic conditions in women: The development of a National Institutes of health framework. BMC Womens Health. 2023; 23(1):162. [DOI:10.1186/s12905-023-02319-x] [PMID]
- Dehkordi AH, Dehabadi EZ, Rezaei MR, Dehkordi AH, Fattahi F, Oskui AG, et al. Empowerment and self-efficacy in patients with chronic disease; A systematic review study. Journal of Nephropharmacology. 2023; 12(2):e10596. [DOI:10.34172/npj.2023.10596]
- Watson KB, Carlson SA, Loustalot F, Town M, Eke PI, Thomas CW, et al. Chronic conditions among adults aged 18─ 34 years-United States, 2019. MMWR. Morbidity and Mortality Weekly Report. 2022; 71(30):964-70. [DOI:10.15585/mmwr.mm7130a3] [PMID]
- Kim GM, Lim JY, Kim EJ, Park SM. Resilience of patients with chronic diseases: A systematic review. Health & Social Care in The Community. 2019; 27(4):797-807. [DOI:10.1111/hsc.12620] [PMID]
- Hu RY, Wang JY, Chen WL, Zhao J, Shao CH, Wang JW, et al. Stress, coping strategies and expectations among breast cancer survivors in China: A qualitative study. BMC Psychology. 2021; 9(1):26. [DOI:10.1186/s40359-021-00515-8] [PMID]
- Işık Ulusoy S, Kal Ö. Relationship among coping strategies, quality of life, and anxiety and depressive disorders in hemodialysis patients. Therapeutic Apheresis and Dialysis. 2020; 24(2):189-96. [DOI:10.1111/1744-9987.12914] [PMID]
- Nazarov S, Manuwald U, Leonardi M, Silvaggi F, Foucaud J, Lamore K, et al. Chronic diseases and employment: which interventions support the maintenance of work and return to work among workers with chronic illnesses? A systematic review. International Journal of Environmental Research and Public Health. 2019; 16(10):1864. [DOI:10.3390/ijerph16101864] [PMID]
- Van Wilder L, Rammant E, Clays E, Devleesschauwer B, Pauwels N, De Smedt D. A comprehensive catalogue of EQ-5D scores in chronic disease: Results of a systematic review. Quality of life Research. 2019; 28(12):3153-61. [DOI:10.1007/s11136-019-02300-y] [PMID]
- Kristofferzon ML, Engström M, Nilsson A. Coping mediates the relationship between sense of coherence and mental quality of life in patients with chronic illness: A cross-sectional study. Quality of Life Research. 2018; 27(7):1855-63. [DOI:10.1007/s11136-018-1845-0] [PMID]
- Kraaij V, Garnefski N. Coping and depressive symptoms in adolescents with a chronic medical condition: A search for intervention targets. Journal of Adolescence. 2012; 35(6):1593-600. [DOI:10.1016/j.adolescence.2012.06.007]
- Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. The lancet. 2015; 385(9968):640-8. [DOI:10.1016/s0140-6736(13)61489-0] [PMID]
- Davis S, Serfaty M, Low J, Armstrong M, Kupeli N, Lanceley A. Experiential avoidance in advanced cancer: A mixed-methods systematic review. International Journal of Behavioral Medicine. 2023; 30(5):585-604. [DOI:10.1007/s12529-022-10131-4] [PMID]
- Masià-Plana A, Sitjar-Suñer M, Mantas-Jiménez S, Suñer-Soler R. The influence of emotional intelligence on quality of life in patients undergoing chronic hemodialysis focused on age and gender. Behavioral Sciences. 2024; 14(3):220. [DOI:10.3390/bs14030220] [PMID]
- Lebel S, Mutsaers B, Tomei C, Leclair CS, Jones G, Petricone-Westwood D, et al. Health anxiety and illness-related fears across diverse chronic illnesses: A systematic review on conceptualization, measurement, prevalence, course, and correlates. PLoS One. 2020; 15(7):e0234124. [DOI:10.1371/journal.pone.0234124] [PMID]
- Siu AM, Chan SC, Cheung MK, Shek DT. Predictors of psychosocial adaptation and mental well-being among people with chronic illnesses and disabilities in Hong Kong. Rehabilitation Counseling Bulletin. 2024; 67(2):147-58. [DOI:10.1177/00343552221115864]
- Doran C, Duits AJ, Gerstenbluth I, Tami A, Bailey A. Adaptive coping strategies among individuals living with long-term chikungunya disease: A qualitative study in Curaçao. BMJ Open. 2024; 14(2):e076352. [DOI:10.1136/bmjopen-2023-076352] [PMID]
- Folkman S, Moskowitz JT. Coping: Pitfalls and promise. Annual Review of Psychology. 2004; 55:745-74. [DOI:10.1146/annurev.psych.55.090902.141456] [PMID]
- Dev R, Agosta M, Fellman B, Reddy A, Baldwin S, Arthur J, et al. Coping strategies and associated symptom burden among patients with advanced cancer. Oncologist. 2024; 29(2):166-75. [DOI:10.1093/oncolo/oyad253] [PMID]
- Liebermann JD, Witte OW, Prell T. Association between different coping styles and health-related quality of life in people with Parkinson’s disease: A cross-sectional study. BMJ Open. 2020; 10(7):e036870 [DOI:10.1136/bmjopen-2020-036870] [PMID]
- Büssing A, Ostermann T, Neugebauer EA, Heusser P. Adaptive coping strategies in patients with chronic pain conditions and their interpretation of disease. BMC Public Health. 2010; 10:507. [DOI:10.1186/1471-2458-10-507] [PMID]
- Büssing A, Fischer J, Haller A, Heusser P, Ostermann T, Matthiessen PF. Validation of the brief multidimensional life satisfaction scale in patients with chronic diseases. European Journal of Medical Research. 2009; 14(4):171-7. [DOI:10.1186/2047-783x-14-4-171] [PMID]
- Büssing A, Fischer J. Interpretation of illness in cancer survivors is associated with health-related variables and adaptive coping styles. BMC Womens Health. 2009; 9:2. [DOI:10.1186/1472-6874-9-2] [PMID]
- Büssing A, Michalsen A, Balzat HJ, Grünther RA, Ostermann T, Neugebauer EA, et al. Are spirituality and religiosity resources for patients with chronic pain conditions? Pain Medicine. 2009; 10(2):327-39. [DOI:10.1111/j.1526-4637.2009.00572.x] [PMID]
- Hair JF. Multivariate data analysis: A global perspective. London: Pearson; 2010. [Link]
- Ostermann T, Büssing A, Matthiessen PF. [Pilot study for the development of a questionnaire for the measuring of the patients' attitude towards spirituality and religiosity and their coping with disease(SpREUK)]. Forsch Komplementarmed Klass Naturheilkd. 2004; 11(6):346-53. [DOI:10.1159/000082816] [PMID]
- Lazarus RS. Coping theory and research: past, present, and future. Psychosomatic Medicine. 1993; 55(3):234-47. [DOI:10.1097/00006842-199305000-00002] [PMID]
- Alipour A, Hashemi T, Babapour J, Tousi F. [Relationship between coping strategies and happiness among university students (Persian)]. Journal of Psychology. 2010; 5(18):71-86. [Link]
- Wu Q, Chen Y, Zhou Y, Zhang X, Huang Y, Liu R. Reliability, validity, and sensitivity of short-form 36 health survey (SF-36) in patients with sick sinus syndrome. Medicine. 2023; 102(24):e33979. [DOI:10.1097%2FMD.0000000000033979] [PMID]
- Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Quality of Life Research. 2005; 14(3):875-82. [PMID]
- Chiniforoushan F, Azadfallah P, Farahani H. [Psychometric properties of the Persian version of the psychological adaptation scale (Persian)]. Clinical Psychology and Personality. 2020; 17(2):125-38. [DOI:10.22070/cpap.2020.2913]
- Wheaton B, Muthen B, Alwin DF, Summers GF. Assessing reliability and stability in panel models. Sociological Methodology. 1977; 8:84-136. [DOI:10.2307/270754]
- Eskandari A, Naeimi M, Fathi-Ashtiani A, Farahani H. [Psychometric properties of the Persian Version of the Orthorexia Nervosa Scale (ORTO-15) (Persian)]. Quarterly Journal of Health Psychology. 2022; 11(43):21-40. [Link]
- Büssing A, Ostermann T, Matthiessen PF. Wer kontrolliert die Gesundheit? Deutsche Zeitschrift für Onkologie. 2008; 40(04):150-6. [DOI:10.1055/s-0028-1082647]
- Niihata K, Fukuma S, Akizawa T, Fukuhara S. Association of coping strategies with mortality and health-related quality of life in hemodialysis patients: The Japan Dialysis Outcomes and Practice Patterns Study. PLoS One. 2017; 12(7):e0180498. [DOI:10.1371%2Fjournal.pone.0180498] [PMID]
- Zamanian H, Poorolajal J, Taheri-Kharameh Z. Relationship between stress coping strategies, psychological distress, and quality of life among hemodialysis patients. Perspectives in Psychiatric Care. 2018; 54(3):410-5. [PMID]
- McCabe MP, McKern S, McDonald E. Coping and psychological adjustment among people with multiple sclerosis. Journal of Psychosomatic Research. 2004; 56(3):355-61. [DOI:10.1016/s0022-3999(03)00132-6] [PMID]
- Desalegn GT, Zeleke TA, Shumet S, Mirkena Y, Kassew T, Angaw DA, et al. Coping strategies and associated factors among people with physical disabilities for psychological distress in Ethiopia. BMC Public Health. 2023; 23(1):20. [DOI:10.1186/s12889-022-14877-0] [PMID]
- Cruz JP, Colet PC, Qubeilat H, Al-Otaibi J, Coronel EI, Suminta RC. Religiosity and health-related quality of life: A cross-sectional study on Filipino Christian hemodialysis patients. Journal of Religion and Health. 2016; 55(3):895-08. [DOI:10.1007/s10943-015-0103-9] [PMID]
- Rahnama P, Javidan AN, Saberi H, Montazeri A, Tavakkoli S, Pakpour AH, et al. Does religious coping and spirituality have a moderating role on depression and anxiety in patients with spinal cord injury? A study from Iran. Spinal Cord. 2015; 53(12):870-4. [PMID]
- Taheri Kharame Z, Zamanian H, Foroozanfar S, Afsahi S. Religious wellbeing as a predictor for quality of life in Iranian hemodialysis patients. Global Journal of Health Science. 2014; 6(4):261-9. [PMID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2024/01/31 | Accepted: 2024/06/11 | Published: 2024/08/19
Received: 2024/01/31 | Accepted: 2024/06/11 | Published: 2024/08/19
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |