Sun, Feb 1, 2026
| فارسی
Volume 29, Issue 1 (Spring 2023)
IJPCP 2023, 29(1): 66-77 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Loghmani L, Mardom M A, Fatemi M, Kalantari S, Shafiei Kisomi Z, Ghasemnegad S M et al . Factors Affecting the Sense of Dignity in Patients With Psychiatric Disorders During Hospitalization in a Psychiatric Hospital in Tehran, Iran. IJPCP 2023; 29 (1) :66-77
URL: http://ijpcp.iums.ac.ir/article-1-3917-en.html
URL: http://ijpcp.iums.ac.ir/article-1-3917-en.html
Laleh Loghmani1 

 , Mohammad Ali Mardom2
, Mohammad Ali Mardom2 

 , Massod Fatemi3
, Massod Fatemi3 

 , Soheyla Kalantari4
, Soheyla Kalantari4 

 , Zahra Shafiei Kisomi5
, Zahra Shafiei Kisomi5 

 , Seideh Madineh Ghasemnegad6
, Seideh Madineh Ghasemnegad6 

 , Hadi Ranjbar7
, Hadi Ranjbar7 




 , Mohammad Ali Mardom2
, Mohammad Ali Mardom2 

 , Massod Fatemi3
, Massod Fatemi3 

 , Soheyla Kalantari4
, Soheyla Kalantari4 

 , Zahra Shafiei Kisomi5
, Zahra Shafiei Kisomi5 

 , Seideh Madineh Ghasemnegad6
, Seideh Madineh Ghasemnegad6 

 , Hadi Ranjbar7
, Hadi Ranjbar7 


1- Department of Nursing, School of Nursing and Midwifery, Bam University of Medical Sciences, Bam, Iran.
2- Department of Nursing, School of Nursing and Midwifery, Arak University of Medical Sciences, Arak, Iran.
3- Department of Nursing, School of Nursing and Midwifery, Tarbiat Modares University, Tehran, Iran.
4- Department of Surgical Technology, Paramedical School, Golestan University of Medical Sciences, Gorgan, Iran.
5- Department of Nursing, School of Nursing and Midwifery, Qazvin University of Medical Sciences, Qazvin, Iran.
6- Department of Nursing, Lahijan Branch, Islamic Azad University, Lahijan, Iran.
7- Mental Health Research Center, Social Injury Prevention Research Institute, Iran University of Medical Sciences, Tehran, Iran. ,ranjbar.h@iums.ac.ir
2- Department of Nursing, School of Nursing and Midwifery, Arak University of Medical Sciences, Arak, Iran.
3- Department of Nursing, School of Nursing and Midwifery, Tarbiat Modares University, Tehran, Iran.
4- Department of Surgical Technology, Paramedical School, Golestan University of Medical Sciences, Gorgan, Iran.
5- Department of Nursing, School of Nursing and Midwifery, Qazvin University of Medical Sciences, Qazvin, Iran.
6- Department of Nursing, Lahijan Branch, Islamic Azad University, Lahijan, Iran.
7- Mental Health Research Center, Social Injury Prevention Research Institute, Iran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 4232 kb]
(857 Downloads)
| Abstract (HTML) (2656 Views)
Full-Text: (1031 Views)
Introduction
Patients’ dignity is related to their respect, autonomy, and satisfaction with the quality of care. In healthcare settings, preserving patients’ dignity is essential for their well-being and satisfaction with the healthcare system. Psychiatric disorders are important public health problems, affecting a significant proportion of people worldwide. Psychiatric patients often require hospitalization to ensure their safety and provide appropriate treatment. However, these patients are at an increased risk of disrespect and losing dignity during their hospitalization, which can further exacerbate their diseases and impede their recovery. Therefore, it is crucial to understand the factors that affect the sense of dignity among patients with psychiatric disorders during their hospitalization. By identifying and addressing the factors, healthcare providers and policy makers can create a more supportive and empowering environment for them to promote their recovery and well-being. This study aims to determine the factors affecting the sense of dignity in patients with psychiatric disorders during hospitalization in Iran Psychiatric Hospital, in Tehran, Iran.
Methods
This cross-sectional study was conducted on 253 adult patients with psychiatric disorders admitted to Iran Psychiatry Hospital. A convenient sampling method was employed to recruit participants. A researcher-made questionnaire was used to assess the patient’s sense of dignity and demographic factors including gender, age, education level, knowledge of diagnosis, history of hospitalization, marital status, diagnosis, and insurance. The questionnaire had 24 items and five dimensions: General respect, respecting autonomy, empowerment, respecting privacy, and acceptance. The questionnaire were distributed in the hospital.
To analyze the collected data, Independent t-test, Pearson’s correlation test, analysis of variance (ANOVA), and linear regression analysis were used. Independent t-test was used to compare the means of the dignity questionnaire between patients with different characteristics. Pearson’s correlation test was used to examine the relationship between the patient’s dignity and age. ANOVA was used to determine whether there were significant differences in the mean scores of the dignity questionnaire among patients with different marital status. Finally, linear regression was used to identify the factors that predict the patient’s dignity during hospitalization.
Results
The majority of patients was female (52.6%) and their mean age was 37.07±10.27 years; 52% were neurotic and 48% were psychotic. The factors of gender, insurance, marital status, and diagnosis had no significant correlation with patient dignity. However, age, educational level, history of hospitalization due to having a mental health disorder, and knowledge of own disease diagnosis were found to be significantly related to the patient dignity.
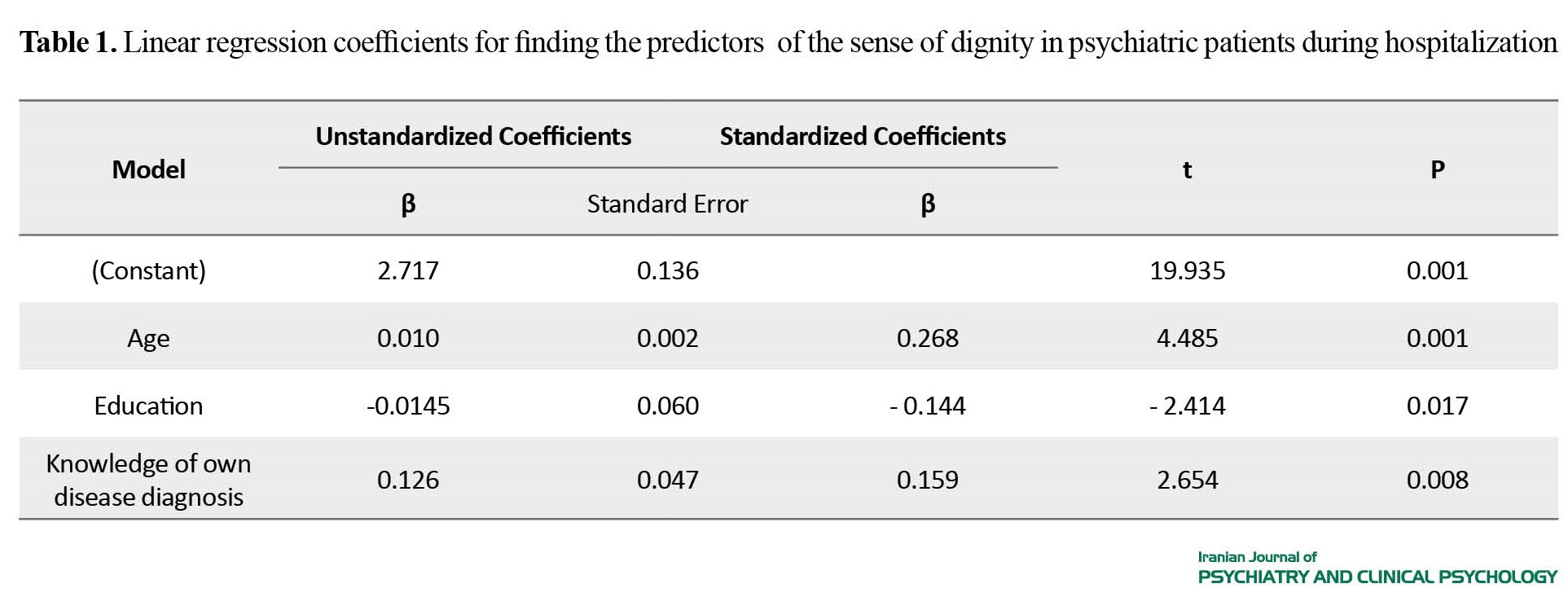
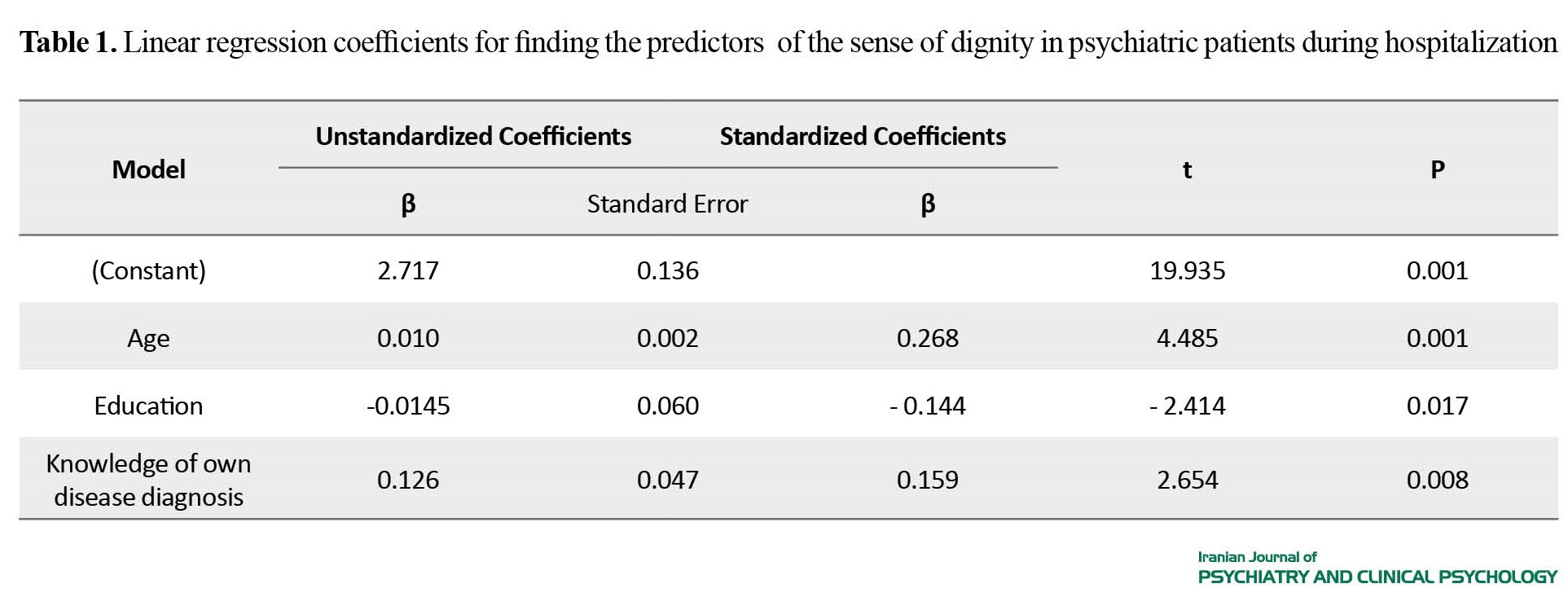
The study found a significant correlation between age and total score of dignity (r=0.266, P<0.001). Those with lower age had lower sense of dignity during hospitalization. Patients with an education level above a diploma had a lower sense of dignity than those with a diploma or lower (3.01 vs. 3.15, P=0.023). Patients who were aware of their own disease diagnosis reported a lower sense of dignity than those who were not aware (3.06 vs. 3.17, P<0.001). Linear regression analysis revealed the significant ability of age, knowledge of own disease diagnosis, and education level to predict the sense of dignity in patients (Table 1).
Conclusion
This study showed the significant effect of factors such as age, education level, and knowledge of own disease diagnosis on the sense of dignity among patients with psychiatric disorders during hospitalization. Healthcare providers and policy makers should pay attention to these factors during interventions to improve the psychiatric patient’s sense of dignity. It is essential to provide age-appropriate care to these patients, address the specific needs of psychiatric patients with higher educational levels, and support them in understanding their disease diagnosis. Such interventions can promote their recovery process and well-being and ensure that they receive the care and respect they deserve. By the preservation of the dignity of psychiatric patients during hospitalization, healthcare providers and policy makers can create a more supportive and better therapeutic environment that fosters positive outcomes for patients.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.096). Participation in this study was voluntary. The personal information of the participants was kept confidential. The purpose of the study was explained to the participants and their informed consent was obtained.
Funding
The research was funded by Iran University of Medical Sciences (Grant No.: 14166).
Authors contributions
Conceptualization: Hadi Ranjbar; Investigation: Mohammad Ali Mardom, Massod Fatemi, Soheyla Kalantari, and Zahra Shafiei Kisomi; Review & editing: Laleh Loghmani and Seyedah Madineh Ghasemnegad; Supervision: Hadi Ranjbar.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank participants for their cooperation in conducting this research.
References
Patients’ dignity is related to their respect, autonomy, and satisfaction with the quality of care. In healthcare settings, preserving patients’ dignity is essential for their well-being and satisfaction with the healthcare system. Psychiatric disorders are important public health problems, affecting a significant proportion of people worldwide. Psychiatric patients often require hospitalization to ensure their safety and provide appropriate treatment. However, these patients are at an increased risk of disrespect and losing dignity during their hospitalization, which can further exacerbate their diseases and impede their recovery. Therefore, it is crucial to understand the factors that affect the sense of dignity among patients with psychiatric disorders during their hospitalization. By identifying and addressing the factors, healthcare providers and policy makers can create a more supportive and empowering environment for them to promote their recovery and well-being. This study aims to determine the factors affecting the sense of dignity in patients with psychiatric disorders during hospitalization in Iran Psychiatric Hospital, in Tehran, Iran.
Methods
This cross-sectional study was conducted on 253 adult patients with psychiatric disorders admitted to Iran Psychiatry Hospital. A convenient sampling method was employed to recruit participants. A researcher-made questionnaire was used to assess the patient’s sense of dignity and demographic factors including gender, age, education level, knowledge of diagnosis, history of hospitalization, marital status, diagnosis, and insurance. The questionnaire had 24 items and five dimensions: General respect, respecting autonomy, empowerment, respecting privacy, and acceptance. The questionnaire were distributed in the hospital.
To analyze the collected data, Independent t-test, Pearson’s correlation test, analysis of variance (ANOVA), and linear regression analysis were used. Independent t-test was used to compare the means of the dignity questionnaire between patients with different characteristics. Pearson’s correlation test was used to examine the relationship between the patient’s dignity and age. ANOVA was used to determine whether there were significant differences in the mean scores of the dignity questionnaire among patients with different marital status. Finally, linear regression was used to identify the factors that predict the patient’s dignity during hospitalization.
Results
The majority of patients was female (52.6%) and their mean age was 37.07±10.27 years; 52% were neurotic and 48% were psychotic. The factors of gender, insurance, marital status, and diagnosis had no significant correlation with patient dignity. However, age, educational level, history of hospitalization due to having a mental health disorder, and knowledge of own disease diagnosis were found to be significantly related to the patient dignity.
The study found a significant correlation between age and total score of dignity (r=0.266, P<0.001). Those with lower age had lower sense of dignity during hospitalization. Patients with an education level above a diploma had a lower sense of dignity than those with a diploma or lower (3.01 vs. 3.15, P=0.023). Patients who were aware of their own disease diagnosis reported a lower sense of dignity than those who were not aware (3.06 vs. 3.17, P<0.001). Linear regression analysis revealed the significant ability of age, knowledge of own disease diagnosis, and education level to predict the sense of dignity in patients (Table 1).
Conclusion
This study showed the significant effect of factors such as age, education level, and knowledge of own disease diagnosis on the sense of dignity among patients with psychiatric disorders during hospitalization. Healthcare providers and policy makers should pay attention to these factors during interventions to improve the psychiatric patient’s sense of dignity. It is essential to provide age-appropriate care to these patients, address the specific needs of psychiatric patients with higher educational levels, and support them in understanding their disease diagnosis. Such interventions can promote their recovery process and well-being and ensure that they receive the care and respect they deserve. By the preservation of the dignity of psychiatric patients during hospitalization, healthcare providers and policy makers can create a more supportive and better therapeutic environment that fosters positive outcomes for patients.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.096). Participation in this study was voluntary. The personal information of the participants was kept confidential. The purpose of the study was explained to the participants and their informed consent was obtained.
Funding
The research was funded by Iran University of Medical Sciences (Grant No.: 14166).
Authors contributions
Conceptualization: Hadi Ranjbar; Investigation: Mohammad Ali Mardom, Massod Fatemi, Soheyla Kalantari, and Zahra Shafiei Kisomi; Review & editing: Laleh Loghmani and Seyedah Madineh Ghasemnegad; Supervision: Hadi Ranjbar.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank participants for their cooperation in conducting this research.
References
- Ricciardelli R, Mitchell M, Taillieu T, Angehrn A, Afifi T, Carleton RN. Pervasive uncertainty under threat: mental health disorders and experiences of uncertainty for correctional workers. Criminal Justice and Behavior. 2022; 49(7):991-1009. [DOI:10.1177/00938548211050112]
- Gadermann AM, Gagné Petteni M, Janus M, Puyat JH, Guhn M, Georgiades K. Prevalence of mental health disorders among immigrant, refugee, and nonimmigrant children and youth in British Columbia, Canada. JAMA Network Open. 2022; 5(2):e2144934. [DOI:10.1001/jamanetworkopen.2021.44934] [PMID] [PMCID]
- Bahrami G, Takaffoli M, Vameghi M. [Protective and risk factors of mental health in Iranian Children during the covid-19 pandemic: A systematic review study (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2022; 28(3):300-13. [DOI:10.32598/ijpcp.28.3.3976.1]
- WHO. Dignity in mental health. Geneva: WHO; 2015. [Link]
- van der Geugten W, Goossensen A. Dignifying and undignifying aspects of care for people with dementia: A narrative review. Scandinavian Journal of Caring Sciences. 2020; 34(4):818-38. [DOI:10.1111/scs.12791] [PMID] [PMCID]
- Sandgren A, Axelsson L, Bylund-Grenklo T, Benzein E. Family members’ expressions of dignity in palliative care: A qualitative study. Scandinavian Journal of Caring Sciences. 2021; 35(3):937-44. [DOI:10.1111/scs.12913] [PMID] [PMCID]
- Brożek B, Fopka-Kowalczyk M, Łabuś-Centek M, Damps-Konstańska I, Ratajska A, Jassem E, et al. Dignity therapy as an aid to coping for COPD patients at their end-of-life stage. Advances in Respiratory Medicine. 2019; 87(3):135-45. [DOI:10.5603/ARM.a2019.0021]
- Ota K, Maeda J, Gallagher A, Yahiro M, Niimi Y, Chan MF, et al. Development of the inpatient dignity scale through studies in Japan, Singapore, and the United Kingdom. Asian Nursing Research. 2019; 13(1):76-85. [DOI:10.1016/j.anr.2019.01.008] [PMID]
- Dakessian Sailian S, Salifu Y, Saad R, Preston N. Dignity of patients with palliative needs in the Middle East: An integrative review. BMC Palliative Care. 2021; 20(1):112. [DOI:10.1186/s12904-021-00791-6] [PMID] [PMCID]
- Bylund-Grenklo T, Werkander-Harstäde C, Sandgren A, Benzein E, Östlund U. Dignity in life and care: The perspectives of Swedish patients in a palliative care context. International Journal of Palliative Nursing. 2019; 25(4):193-201. [DOI:10.12968/ijpn.2019.25.4.193] [PMID]
- Avestan Z, Pakpour V, Rahmani A, Mohammadian R, Soheili A. The correlation between respecting the dignity of cancer patients and the quality of nurse-patient communication. Indian Journal of Palliative Care. 2019; 25(2):190-6. [DOI:10.4103/IJPC.IJPC_46_18] [PMID] [PMCID]
- Banerjee D, Rabheru K, de Mendonca Lima CA, Ivbijaro G. Role of Dignity in mental healthcare: Impact on ageism and human rights of older persons. American Journal of Geriatric Psychiatry. 2021; 29(10):1000-8. [DOI:10.1016/j.jagp.2021.05.011] [PMID]
- Khosropanah AH, Hoseini AS, Dehghan Nayeri N. Comparison of the concept of patient dignity in Islamic and nursing texts. Medical Research Archives. 2020; 8(6):1-12. [Link]
- Manookian A, Cheraghi MA, Nikbakht Nasrabadi A, Peiravi H, Shali M. Nurses’ lived experiences of preservation of patients’ dignity. Journal of Medical Ethics & History of Medicine. 2014; 7(1):22-33. [Link]
- Sadeghi T, Dehghan Nayyeri N. [Patients’ dignity: Patients’ and nurses’ perspectives (Persian)]. Iranian Journal of Medical Ethics and History of Medicine. 2009; 3(1):9-20. [Link]
- Plunkett R, Kelly BD. Dignity: The elephant in the room in psychiatric inpatient care? A systematic review and thematic synthesis. International Journal of Law and Psychiatry. 2021; 75:101672. [DOI:10.1016/j.ijlp.2021.101672] [PMID]
- Shojaei A, Raziani Y, Bernstein C, Asgari A, Alazmani-Noodeh F, Arab M, et al. The experiences of psychiatric patients, their caregivers and companions in upholding patient dignity during hospitalization: A qualitative study. Health Expectations. 2023. [PMID]
- Weber CA, Juruena MF. Day hospital and psychosocial care center: Expanding the discussion of partial hospitalization in mental health. Revista da Associacao Medica Brasileira (1992). 2016; 62(4):361-7. [DOI:10.1590/1806-9282.62.04.361] [PMID]
- Peyvakht A, Sanagoo A, Behnampour N, Roshandel G, Jouybari L. [Perspectives of nurses and the elderly hospitalized patients eegard respecting the human dignity of elderly patients in educational and Medical Centers of Golestan University of Medical Sciences in 2019 (Persian)]. Journal of Nursing Education. 2020; 9(3):79-87. [Link]
- Hadler RA, Goldshore M, Rosa WE, Nelson J.“What do I need to know about you?”: The Patient Dignity Question, age, and proximity to death among patients with cancer. Supportive Care in Cancer. 2022; 30(6):5175-86. [DOI:10.1007/s00520-022-06938-2] [PMID] [PMCID]
- Sizer MA, Bhatta D, Acharya B, Paudel KP. Determinants of telehealth service use among mental health patients: A case of rural Louisiana. International Journal of Environmental Research and Public Health. 2022; 19(11):6930.[DOI:10.3390/ijerph19116930] [PMID] [PMCID]
- SarikoÇ G, Unay E. Mental health literacy in individuals diagnosed with diabetes. Online Türk Sağlık Bilimleri Dergisi. 2023; 8(2):213-9. [DOI:10.26453/otjhs.1213619]
- Wibowo Y, Mulyanto J, Siswandari VMW, Munfiah S. Study of knowledge, attitude, anxiety and perception of mental health service needs related to the covid-19 pandemic in Banyumas Regency, Central Java, Indonesia: A cross-sectional study. Journal of Health Promotion and Behavior. 2022; 7(2):142-51. [Link]
- Elnemais Fawzy M. Balancing indications for hospitalization and legal consideration: Moving from problems to solutions: A culturally sensitive debate review in Middle East and Arab world. International Journal of Mental Health. 2021; 50(3):271-84. [DOI:10.1080/00207411.2021.1919821]
- Gallagher A, Wainwright P, Baillie L, Ford P. The RCN dignity survey: Implications for leaders. Nursing Management (Harrow, London, England : 1994). 2009; 16(4):12-6. [DOI:10.7748/nm2009.07.16.4.12.c7132] [PMID]
- Tew J, Ramon S, Slade M, Bird V, Melton J, Le Boutillier C. Social factors and recovery from mental health difficulties: A review of the evidence. The British Journal of Social Work. 2012; 42(3):443-60. [DOI:10.1093/bjsw/bcr076]
- Chochinov HM. Dignity therapy: Final words for final days. Oxford Oxford: University Press; 2012. [DOI:10.1093/acprof:oso/9780195176216.001.0001]
- Bagheri A. Elements of human dignity in healthcare settings: The importance of the patient’s perspective. Journal of Medical Ethics. 2012; 38(12):729-30. [DOI:10.1136/medethics-2012-100743] [PMID]
- Skorpen F, Thorsen AA, Forsberg C, Rehnsfeldt AW. Suffering related to dignity among patients at a psychiatric hospital. Nursing Ethics. 2014; 21(2):148-62. [DOI:10.1177/0969733013493216] [PMID]
- Chambers M, Gallagher A, Borschmann R, Gillard S, Turner K, Kantaris X. The experiences of detained mental health service users: Issues of dignity in care. BMC Medical Ethics. 2014; 15:50. [DOI:10.1186/1472-6939-15-50] [PMID] [PMCID]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2023/01/6 | Accepted: 2023/03/12 | Published: 2023/04/1
Received: 2023/01/6 | Accepted: 2023/03/12 | Published: 2023/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |