Sun, Nov 9, 2025
| فارسی
Volume 29, Issue 1 (Spring 2023)
IJPCP 2023, 29(1): 48-65 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Borji M, Hajebi A, Naserbakht M, Ranjbar H, Fazeli A, Khorrami Z et al . Evaluating the Efficacy of School Mental Health Promotion Program in Iranian Schools: A Qualitative Study. IJPCP 2023; 29 (1) :48-65
URL: http://ijpcp.iums.ac.ir/article-1-3902-en.html
URL: http://ijpcp.iums.ac.ir/article-1-3902-en.html
Mitra Borji1 

 , Amirali Hajebi2
, Amirali Hajebi2 

 , Morteza Naserbakht3
, Morteza Naserbakht3 

 , Helia Ranjbar4
, Helia Ranjbar4 

 , Asal Fazeli5
, Asal Fazeli5 

 , Zahra Khorrami6
, Zahra Khorrami6 

 , Ahmad Hajebi7
, Ahmad Hajebi7 




 , Amirali Hajebi2
, Amirali Hajebi2 

 , Morteza Naserbakht3
, Morteza Naserbakht3 

 , Helia Ranjbar4
, Helia Ranjbar4 

 , Asal Fazeli5
, Asal Fazeli5 

 , Zahra Khorrami6
, Zahra Khorrami6 

 , Ahmad Hajebi7
, Ahmad Hajebi7 


1- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health, Iran University of Medical Sciences, Tehran, Iran.
2- Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
3- Mental Health Research Center, Health Research Institute, Iran University of Medical Sciences, Tehran, Iran. ,mnaserbakht@gmail.com
4- Department of administration, Faculty of Management, Tehran University, Tehran, Iran.
5- Department of psychology, Faculty of Psychology and Education, Allameh Tabataba'i University, Tehran, Iran.
6- Department of clinical psychology, School of Behavioral Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
7- Research Center for Addiction & Risky Behaviors (ReCARB), Health research Institute, Iran Psychiatric Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
3- Mental Health Research Center, Health Research Institute, Iran University of Medical Sciences, Tehran, Iran. ,
4- Department of administration, Faculty of Management, Tehran University, Tehran, Iran.
5- Department of psychology, Faculty of Psychology and Education, Allameh Tabataba'i University, Tehran, Iran.
6- Department of clinical psychology, School of Behavioral Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
7- Research Center for Addiction & Risky Behaviors (ReCARB), Health research Institute, Iran Psychiatric Hospital, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 6538 kb]
(907 Downloads)
| Abstract (HTML) (2577 Views)
Full-Text: (1784 Views)
Introduction
Over the past twenty years, mental health problems among children and adolescents have been increasing worldwide. Research showed that nearly half of all psychiatric disorders diagnosed in adulthood actually begin in childhood and adolescence. In recent years, the prevalence of mental illness in Iran has been on the rise. This indicates the need to pay attention to the effectiveness of existing interventions and adopt strategies to manage these conditions. Schools can help identify and address significant mental health problems in children and adolescents.
Therefore, due to the need to identify problems related to mental health among students and their proper management by offering specialized medical services to them, recently a relevant research project has been fully implemented in schools of all grades in Iran. The research project, entitled the School Mental Health (SMH) Program, is evidence-based and its protocol is published in the form of a handbook. The handbook is approved by all member states of the World Health Organization (WHO) in the Eastern Mediterranean Region. The present study aims to assess the efficacy of this program in Iranian schools, find its shortcomings, and provide recommendations to improve it.
Methods
The present study was a qualitative study using conventional content analysis that used a semi-structured in-depth interview and FGD to obtain information from groups of stakeholders. Purposeful sampling was used in this study. In this study, a total of 5 focus groups were held. The interviews continued until the saturation was reached so that no new code was found. Accordingly, a pilot project, according to the above-mentioned published handbook, has been implemented in schools after translation and customization.
Results
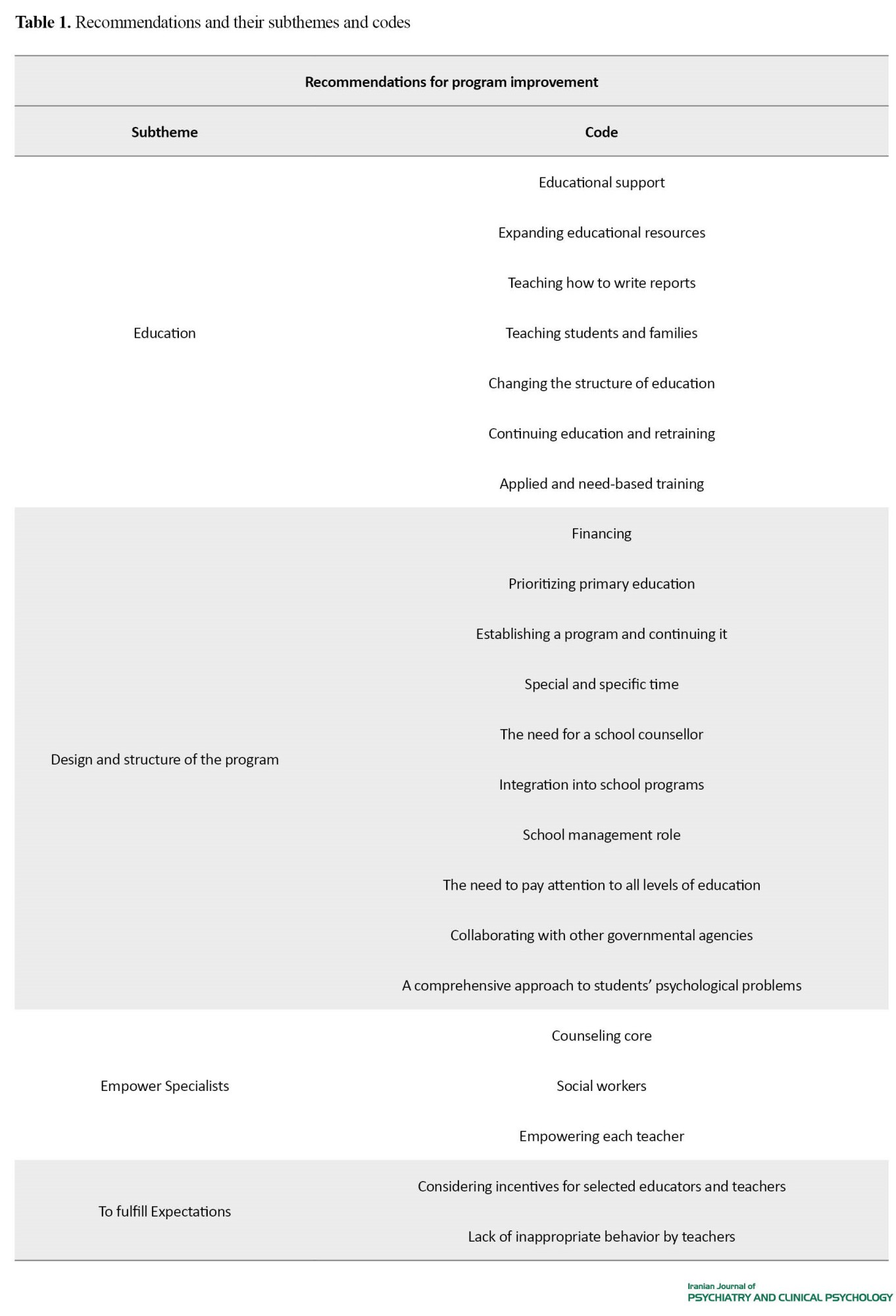
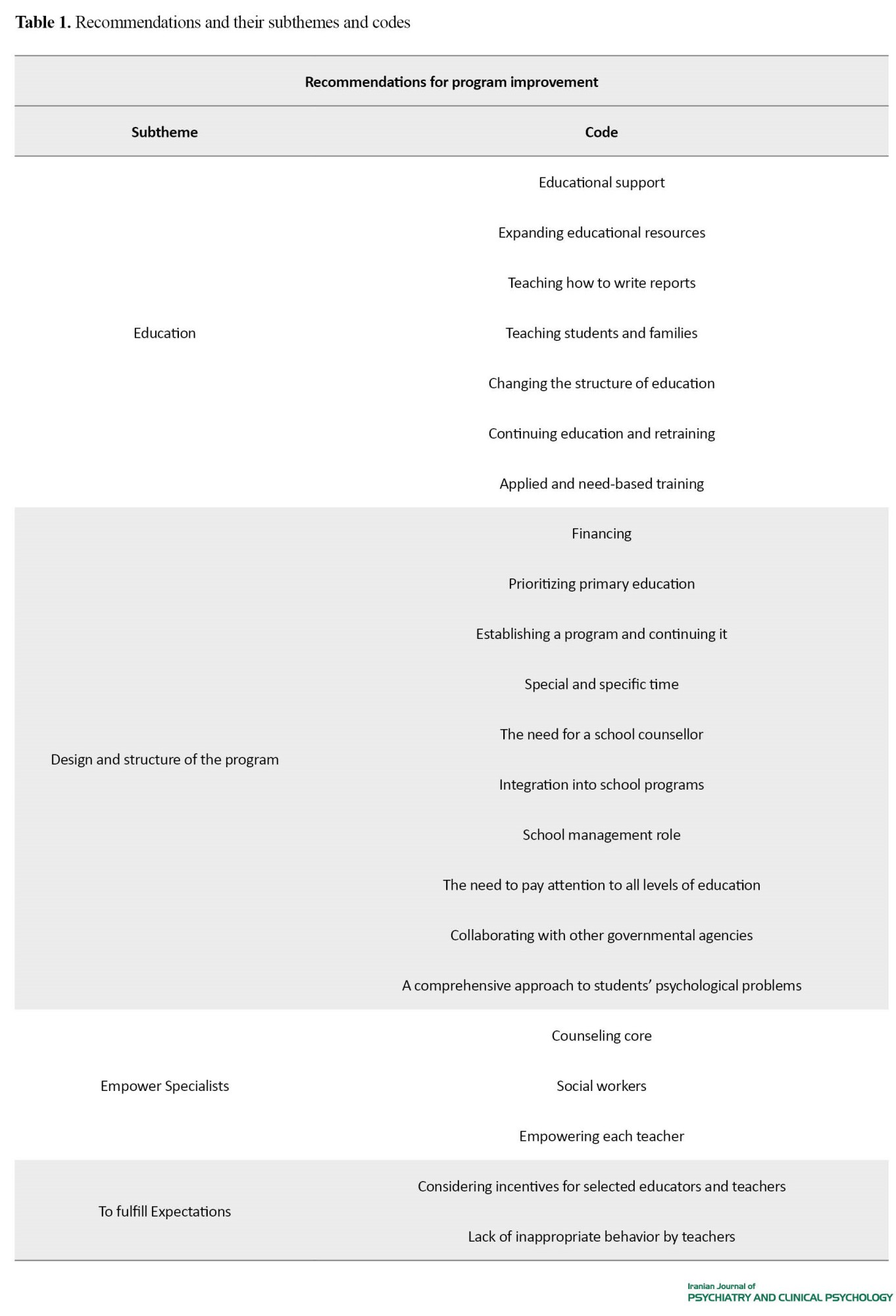
The findings of the present study were presented in four themes: 1. Program strengths, 2. program weaknesses, 3. factors preventing the achievement of program objectives and 4. recommendations for program improvement. It is to be noted that 50 codes were extracted and 14 subcategories were obtained.
According to some participant 's opinion about strengths: "The course has made us a little more open, a little more focused on some kids" and "one of the strengths of empowerment was, raising the sense of responsibility in the selected instructors and their strong commitment, which was the basis for these interventions in schools ".
According to some participant 's opinion about Weaknesses: "I think the issue of families is a gap in this project", "we have to have feedback; we don't get specialized results" and "the selected trainers were people who had 1. Not enough time, 2. Lack of expertise and 3. That, like a social worker, did not have a wide field of work."
According to some participant 's opinion about factors preventing the achievement: "The problem in the treatment process is that the families don't cooperate, or if they do, it's not continuous, and also they don't go for treatment and there is a fear of stigmatization."
According to some participant 's opinion about program improvement
"Keep in mind that these teachings are very effective for children and teachers, as well as parents "and "we really need to have one person on the subject of psychology in every school" (Table 1).
Conclusion
The present study evaluated the School Mental Health Program, and since the research in this field is small and vague, we examined the mentioned topics using the stakeholders’ perspectives.
School-centered interventions mostly involved school members and context for primary interventions. The results of the study showed that the interventions led to the empowerment of teachers and educators in these schools for identifying students’ psychiatric disorders compared to pre-intervention status, reducing teachers’ burnout and improving classroom management, as well as changing their attitudes toward students' psychological problems. Studies have shown that trained teachers have a high potential to participate in the provision of mental health services and that educational interventions in the group of teachers who were not trained have been able to improve teachers' attitudes toward identifying and referring students. Thus, the teacher is at the forefront of mental health programs that are in direct contact with students.
Factors that prevent the achievement of the project goals were: financial problems and lack of education of students and their families for seeking counseling, the quality of counseling services at the core of counseling (lack of expertise in various fields and lack of feedback to lower levels), the high workload of some teachers and time constraints of the selected trainers.
One of the limitations of this plan was the lack of attention to family education and their justification for participation and follow-up. Moreover, programs that focused on multiple target groups (such as individuals, families, and school staff) and combination programs that focused on behavioral changes of students, teachers, families, and relationships between school, family, and other social institutions were the most influential.
Modifications to some rules and regulations in education, feedback, and appropriate responses from specialized levels (counselling centers and community-based mental health centers) to lower levels. Improving enrollment and reporting, continuous and gradual retraining, lack of intensive training, coordination of all project members, including teachers, educators, counselling centers, considering incentives for the positive performance of teachers and educators are also recommended.
Among the recommendations made one is that the project results should continue and the participation of all stakeholders should be sought and supported for its sustainability
The overall results of the evaluation of the School Mental Health Program showed its effectiveness. The new and practical model of the School Mental Health Program has opened a new perspective on school-based interventions. Change in organizations is more complex and requires resources, facilities, expertise, and time. Therefore, by foreseeing and drawing a broad and appropriate outlook, while realistically recognizing the situation, proper steps should be planned and implemented to organize the establishment of mental health services in schools.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.865).
Funding
This study was funded by Iran University of Medical Sciences.
Authors contributions
The authors contributed equally to preparing this paper.
Conflicts of interest
The authors declare no conflict of interests.
Acknowledgements
The authors would like to thank the participants for their cooperation.
References
Over the past twenty years, mental health problems among children and adolescents have been increasing worldwide. Research showed that nearly half of all psychiatric disorders diagnosed in adulthood actually begin in childhood and adolescence. In recent years, the prevalence of mental illness in Iran has been on the rise. This indicates the need to pay attention to the effectiveness of existing interventions and adopt strategies to manage these conditions. Schools can help identify and address significant mental health problems in children and adolescents.
Therefore, due to the need to identify problems related to mental health among students and their proper management by offering specialized medical services to them, recently a relevant research project has been fully implemented in schools of all grades in Iran. The research project, entitled the School Mental Health (SMH) Program, is evidence-based and its protocol is published in the form of a handbook. The handbook is approved by all member states of the World Health Organization (WHO) in the Eastern Mediterranean Region. The present study aims to assess the efficacy of this program in Iranian schools, find its shortcomings, and provide recommendations to improve it.
Methods
The present study was a qualitative study using conventional content analysis that used a semi-structured in-depth interview and FGD to obtain information from groups of stakeholders. Purposeful sampling was used in this study. In this study, a total of 5 focus groups were held. The interviews continued until the saturation was reached so that no new code was found. Accordingly, a pilot project, according to the above-mentioned published handbook, has been implemented in schools after translation and customization.
Results
The findings of the present study were presented in four themes: 1. Program strengths, 2. program weaknesses, 3. factors preventing the achievement of program objectives and 4. recommendations for program improvement. It is to be noted that 50 codes were extracted and 14 subcategories were obtained.
According to some participant 's opinion about strengths: "The course has made us a little more open, a little more focused on some kids" and "one of the strengths of empowerment was, raising the sense of responsibility in the selected instructors and their strong commitment, which was the basis for these interventions in schools ".
According to some participant 's opinion about Weaknesses: "I think the issue of families is a gap in this project", "we have to have feedback; we don't get specialized results" and "the selected trainers were people who had 1. Not enough time, 2. Lack of expertise and 3. That, like a social worker, did not have a wide field of work."
According to some participant 's opinion about factors preventing the achievement: "The problem in the treatment process is that the families don't cooperate, or if they do, it's not continuous, and also they don't go for treatment and there is a fear of stigmatization."
According to some participant 's opinion about program improvement
"Keep in mind that these teachings are very effective for children and teachers, as well as parents "and "we really need to have one person on the subject of psychology in every school" (Table 1).
Conclusion
The present study evaluated the School Mental Health Program, and since the research in this field is small and vague, we examined the mentioned topics using the stakeholders’ perspectives.
School-centered interventions mostly involved school members and context for primary interventions. The results of the study showed that the interventions led to the empowerment of teachers and educators in these schools for identifying students’ psychiatric disorders compared to pre-intervention status, reducing teachers’ burnout and improving classroom management, as well as changing their attitudes toward students' psychological problems. Studies have shown that trained teachers have a high potential to participate in the provision of mental health services and that educational interventions in the group of teachers who were not trained have been able to improve teachers' attitudes toward identifying and referring students. Thus, the teacher is at the forefront of mental health programs that are in direct contact with students.
Factors that prevent the achievement of the project goals were: financial problems and lack of education of students and their families for seeking counseling, the quality of counseling services at the core of counseling (lack of expertise in various fields and lack of feedback to lower levels), the high workload of some teachers and time constraints of the selected trainers.
One of the limitations of this plan was the lack of attention to family education and their justification for participation and follow-up. Moreover, programs that focused on multiple target groups (such as individuals, families, and school staff) and combination programs that focused on behavioral changes of students, teachers, families, and relationships between school, family, and other social institutions were the most influential.
Modifications to some rules and regulations in education, feedback, and appropriate responses from specialized levels (counselling centers and community-based mental health centers) to lower levels. Improving enrollment and reporting, continuous and gradual retraining, lack of intensive training, coordination of all project members, including teachers, educators, counselling centers, considering incentives for the positive performance of teachers and educators are also recommended.
Among the recommendations made one is that the project results should continue and the participation of all stakeholders should be sought and supported for its sustainability
The overall results of the evaluation of the School Mental Health Program showed its effectiveness. The new and practical model of the School Mental Health Program has opened a new perspective on school-based interventions. Change in organizations is more complex and requires resources, facilities, expertise, and time. Therefore, by foreseeing and drawing a broad and appropriate outlook, while realistically recognizing the situation, proper steps should be planned and implemented to organize the establishment of mental health services in schools.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.865).
Funding
This study was funded by Iran University of Medical Sciences.
Authors contributions
The authors contributed equally to preparing this paper.
Conflicts of interest
The authors declare no conflict of interests.
Acknowledgements
The authors would like to thank the participants for their cooperation.
References
- World Health Organization. Creating an environment for emotional and social well-being: An important responsibility of a health promoting and child-friendly school. Geneva: World Health Organization; 2003.
- Imran N, Rahman A, Chaudhry N, Asif A. World Health Organization “School Mental Health Manual”-based training for school teachers in Urban Lahore, Pakistan: Study protocol for a randomized controlled trial. Trials. 2018; 19(1):290. [DOI:10.1186/s13063-018-2679-3] [PMID] [PMCID]
- Bowyer M, Fein EC, Krishnamoorthy G. Teacher mental health literacy and child development in Australian primary schools: A program evaluation. Education Sciences. 2023; 13(4):329. [DOI:10.3390/educsci13040329]
- Chisholm KE, Patterson P, Torgerson C, Turner E, Birchwood M. A randomised controlled feasibility trial for an educational school-based mental health intervention: Study protocol. BMC Psychiatry. 2012; 12:23. [DOI:10.1186/1471-244X-12-23] [PMID] [PMCID]
- Copeland WE, Wolke D, Shanahan L, Costello EJ. Adult functional outcomes of common childhood psychiatric problems: A prospective, longitudinal study. JAMA Psychiatry. 2015; 72(9):892-9. [DOI:10.1001/jamapsychiatry.2015.0730] [PMID] [PMCID]
- Weare K, Nind M. Mental health promotion and problem prevention in schools: What does the evidence say? Health Promotion International. 2011; 26(Suppl 1):i29-69. [DOI:10.1093/heapro/dar075] [PMID]
- Weare K. Mental health and social and emotional learning: Evidence, principles, tensions, balances. Advances in School Mental Health Promotion. 2010; 3(1):5-17. [DOI:10.1080/1754730X.2010.9715670]
- O'Reilly M, Svirydzenka N, Adams S, Dogra N. Review of mental health promotion interventions in schools. Social Psychiatry and Psychiatric Epidemiology. 2018; 53(7):647-62. [DOI:10.1007/s00127-018-1530-1] [PMID] [PMCID]
- Wignall A, Kelly C, Grace P. How are whole-school mental health programmes evaluated? A systematic literature review. Pastoral Care in Education. 2022; 40(2):217-37. [DOI:10.1080/02643944.2021.1918228]
- Jorm AF, Kitchener BA, Sawyer MG, Scales H, Cvetkovski S. Mental health first aid training for high school teachers: A cluster randomized trial. BMC Psychiatry. 2010; 10:51. [DOI:10.1186/1471-244X-10-51] [PMID] [PMCID]
- Yamaguchi S, Foo JC, Nishida A, Ogawa S, Togo F, Sasaki T. Mental health literacy programs for school teachers: A systematic review and narrative synthesis. Early Intervention in Psychiatry. 2020; 14(1):14-25. [DOI:10.1111/eip.12793] [PMID]
- Weist MD, Murray M. Advancing school mental health promotion globally. Advances in School Mental Health Promotion. 2008; 1(sup1):2-12. [DOI:10.1080/1754730X.2008.9715740]
- Hamoda HM, Hoover S, Bostic J, Rahman A, Saaed K. Development of a World Health Organization mental health in schools programme in the Eastern Mediterranean Region. Eastern Mediterranean Health Journal. 2022; 28(3):225-32. [DOI:10.26719/emhj.22.022] [PMID]
- WHO. Mental health in schools: A manual. Cairo: World Health Organization, Eastern Mediterranean Regional Office; 2016. [Link]
- Tyler RW. Basic principles of curriculum and instruction. Chicago: University of Chicago Press; 1950. [Link]
- Becker KD, Park AL, Boustani MM, Chorpita BF. A pilot study to examine the feasibility and acceptability of a coordinated intervention design to address treatment engagement challenges in school mental health services. Journal of School Psychology. 2019; 76:78-88. [DOI:10.1016/j.jsp.2019.07.013] [PMID]
- Jennings J, Pearson G, Harris M. Implementing and maintaining school-based mental health services in a large, urban school district. The Journal of School Health. 2000; 70(5):201-5. [DOI:10.1111/j.1746-1561.2000.tb06473.x] [PMID]
- Nabors LA, Reynolds MW. Program evaluation activities: Outcomes related to treatment for adolescents receiving school-based mental health services. Children’s Services: Social Policy, Research, and Practice. 2000; 3(3):175-89. [DOI:10.1207/S15326918CS0303_4]
- Ross SW, Horner RH. Bully prevention in positive behavior support. Journal of Applied Behavior Analysis. 2009; 42(4):747-59. [DOI:10.1901/jaba.2009.42-747] [PMID] [PMCID]
- Lynch D, Keenan M. The good behaviour game: Maintenance effects. International Journal of Educational Research. 2018; 87:91-9. [DOI:10.1016/j.ijer.2016.05.005]
- Wallace MD, Iwata BA, Hanley GP, Thompson RH, Roscoe EM. Noncontingent reinforcement: A further examination of schedule effects during treatment. Journal of Applied Behavior Analysis. 2012; 45(4):709-19. [DOI:10.1901/jaba.2012.45-709] [PMID] [PMCID]
- Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006; 18(1):59-82. [DOI:10.1177/1525822X05279903]
- Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, CA: Sage Publications; 2002. [Link]
- Denzin NK, Lincoln YS. The SAGE handbook of qualitative research. Thousand Oaks, CA: Sage Publications; 2018. [Link]
- Murano D, Sawyer JE, Lipnevich AA. A meta-analytic review of preschool social and emotional learning interventions. Review of Educational Research. 2020; 90(2):227-63. [DOI:10.3102/0034654320914743]
- Sklad M, Diekstra R, Ritter MD, BEN J, Gravesteijn C. Effectiveness of school-based universal social, emotional, and behavioral programs: Do they enhance students’ development in the area of skill, behavior, and adjustment? Psychology in The Schools. 2012; 49(9):892-909. [DOI:10.1002/pits.21641]
- Colomeischi AA, Duca DS, Bujor L, Rusu PP, Grazzani I, Cavioni V. Impact of a school mental health program on children’s and adolescents’ socio-emotional skills and psychosocial difficulties. Children. 2022; 9(11):1661. [DOI:10.3390/children9111661] [PMID] [PMCID]
- Kaveh MH, Shojaeezadeh D, Shahmohammadi D, Rahimi A, Bolhari J. [Teachers’ role in elementary school mental health: Results of an interventional study (Persian)]. Payesh (Health Monitor) Journal. 2003; 2(2):101-9. [Link]
- Mohit A. Mental health promotion for schoolchildren: A manual for schoolteachers and school health workers. Alexandria WHO, Regional Office for the Eastern Mediterranean; 1998. [Link]
- Franklin CGS, Kim JS, Ryan TN, Kelly M, Montgomery KL. Teacher involvement in school mental health interventions: A systematic review. Children and Youth Services Review. 2012; 34(5):973-82. [DOI:10.1016/j.childyouth.2012.01.027]
- Cefai C, Arlove A, Duca M, Galea N, Muscat M, Cavioni V. RESCUR Surfing the Waves: An evaluation of a resilience programme in the early years. Pastoral Care in Education. 2018; 36(3):189-204. [DOI:10.1080/02643944.2018.1479224]
- Cavioni V, Grazzani I, Ornaghi V. Mental health promotion in schools: A comprehensive theoretical framework. International Journal of Emotional Education. 2020; 12(1):65-82. [Link]
- Kratochwill TR, Mcdonald L, Levin JR, Scalia PA, Coover G. Families and schools together: An experimental study of multi-family support groups for children at risk. Journal of School Psychology. 2009; 47(4):245-65. [DOI:10.1016/j.jsp.2009.03.001] [PMID]
- Greenberg MT, Domitrovich C, Bumbarger B. The prevention of mental disorders in school-aged children: Current state of the field. Prevention & Treatment. 2001; 4(1):Article 1a. [DOI:10.1037/1522-3736.4.1.41a]
- Durlak JA, Wells AM. Primary prevention mental health programs for children and adolescents: A meta-analytic review. American Journal of Community Psychology. 1997; 25(2):115-52. [DOI:10.1023/A:1024654026646] [PMID]
- Egan TE, Wymbs FA, Owens JS, Evans SW, Hustus C, Allan DM. Elementary school teachers’ preferences for school-based interventions for students with emotional and behavioral problems. Psychology in the Schools. 2019; 56(10):1633-53. [DOI:10.1002/pits.22294]
- Weist MD, Goldstein J, Evans SW, Lever NA, Axelrod J, Schreters R, et al. Funding a full continuum of mental health promotion and intervention programs in the schools. The Journal of Adolescent Health. 2003; 32(6 Suppl):70-8. [DOI:10.1016/S1054-139X(03)00067-3] [PMID]
- Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child Development. 2011; 82(1):405-32. [DOI:10.1111/j.1467-8624.2010.01564.x] [PMID]
- Gibson JE, Stephan S, Brandt NE, Lever NA. Supporting teachers through consultation and training in mental health. In: Weist M, Lever N, Bradshaw C, Owens J, editors. Handbook of school mental health. issues in clinical child psychology. Boston: Springer; 2014. [DOI:10.1007/978-1-4614-7624-5_20]
- Sutan R, NurEzdiani M, Abd Rahim MA, Mokhtar D, Abdul Rahman R, Hafiz Johani F, et al. Systematic review of school-based mental health intervention among primary school children. Journal of community Medicine & Health Education. 2018; 8(1):589. [DOI:10.4172/2161-0711.1000589]
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2023/01/3 | Accepted: 2023/03/11 | Published: 2023/04/1
Received: 2023/01/3 | Accepted: 2023/03/11 | Published: 2023/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |