Sun, Feb 15, 2026
| فارسی
Volume 27, Issue 4 (Winter 2022)
IJPCP 2022, 27(4): 412-427 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shareh H, Robati Z. Effect of Acceptance and Commitment Group Therapy on Cognitive Flexibility, Suicidal Ideation, Depression, and Hopelessness in Conscripts. IJPCP 2022; 27 (4) :412-427
URL: http://ijpcp.iums.ac.ir/article-1-3095-en.html
URL: http://ijpcp.iums.ac.ir/article-1-3095-en.html
1- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Hakim Sabzevari University, Sabzevar, Iran. , hsharreh@yahoo.com.au
2- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Semnan University, Semnan, Iran.
2- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Semnan University, Semnan, Iran.
Keywords: Flexibility, Suicide, Depression, Hopelessness, Acceptance and commitment therapy, conscripts
Full-Text [PDF 6018 kb]
(3036 Downloads)
| Abstract (HTML) (7612 Views)
Full-Text: (3052 Views)
1. Introduction
Iranian society is a young society because more than 33% of its population comprised of young people. Of these, eligible males enters the military service according to the laws and in order to protect the Islamic Republic System. Entering the military service leads to major changes in individual, family and social life of people, and is a sensitive period. This period is associated with a lot of stress caused by separation from family and loved ones, changes in dietary habits, restrictions on freedom of choice and action, high and imposed discipline, frequent and forced relocation, changes in sleeping habits, performance anxiety on expectations, fear of having a relationship with others, and inability to resolve problems properly.
Suicide exists in all age groups, but it is more common among young people, especially conscripts, due to their specific situations. According to the World Health Organization, about 800,000 people commit suicide worldwide each year, and it was predicted that this figure would reach 1.5 million people a year by 2020. Nosratabadi et al. found that 28.4% of conscripts are at a high risk of suicidal ideation [8]. Depression is the most important and well-known predictor of suicidal ideation and suicide attempt. Depressed people who commit suicide believe that there is no hope for their future. Hopelessness is an important cause of suicide attempt in depressed people. Cognitive factors such as negativism and hopelessness along with a pessimistic view of the future, belief in disability and inadequacy, and social isolation can increase one’s vulnerability to depression and suicide.
One of the effective approaches in the treatment of depression is Acceptance and Commitment Therapy (ACT), which was introduced by Hayes et al. in the early 1980. The main purpose of ACT is to increase cognitive flexibility through six core processes of acceptance, cognitive defusion, self as context, contact with the present moment, values, and committed action. Cognitive flexibility is a major characteristic of human cognition and refers to one’s ability to simultaneously consider the two conflicting aspects of an object or event. Given the effectiveness of ACT in patients with a variety of psychological disorders, it seems to improve cognitive flexibility and thus reduce suicidal ideation, depression, and hopelessness in conscripts. Therefore, the present study aims to evaluate the effect of ACT group therapy on suicidal ideation, depression, hopelessness and cognitive flexibility among conscripts.
2. Methods
This is a clinical trial with a pretest/posttest design using a control group. The study population consisted of all depressed conscripts referred to military counseling centers in Khorasan Razavi Province of Iran. Of these, 60 conscripts who met the inclusion criteria were randomly selected and assigned into two groups of intervention (n=30) and control (n=30), using a convenience sampling method. The data collection tools were the Beck Scale for Suicidal Ideation, Beck Hopelessness Scale, Beck Depression Inventory-II, and Cognitive Flexibility Inventory. The intervention group received ACT at eight 90-minute sessions, while the control group received no intervention and remained on the waiting list. To analyze the collected data, one-way Analysis of Covariance (ANCOVA) was used in SPSS v. 24 software.
3. Results
Depression, suicidal ideation and hopelessness scores of both groups were very high in the pretest phase. The scores of these variables changed reduced in the intervention group after treatment. The results of ANCOVA comparing the two groups after removing the pretest effects are presented in Table 1.
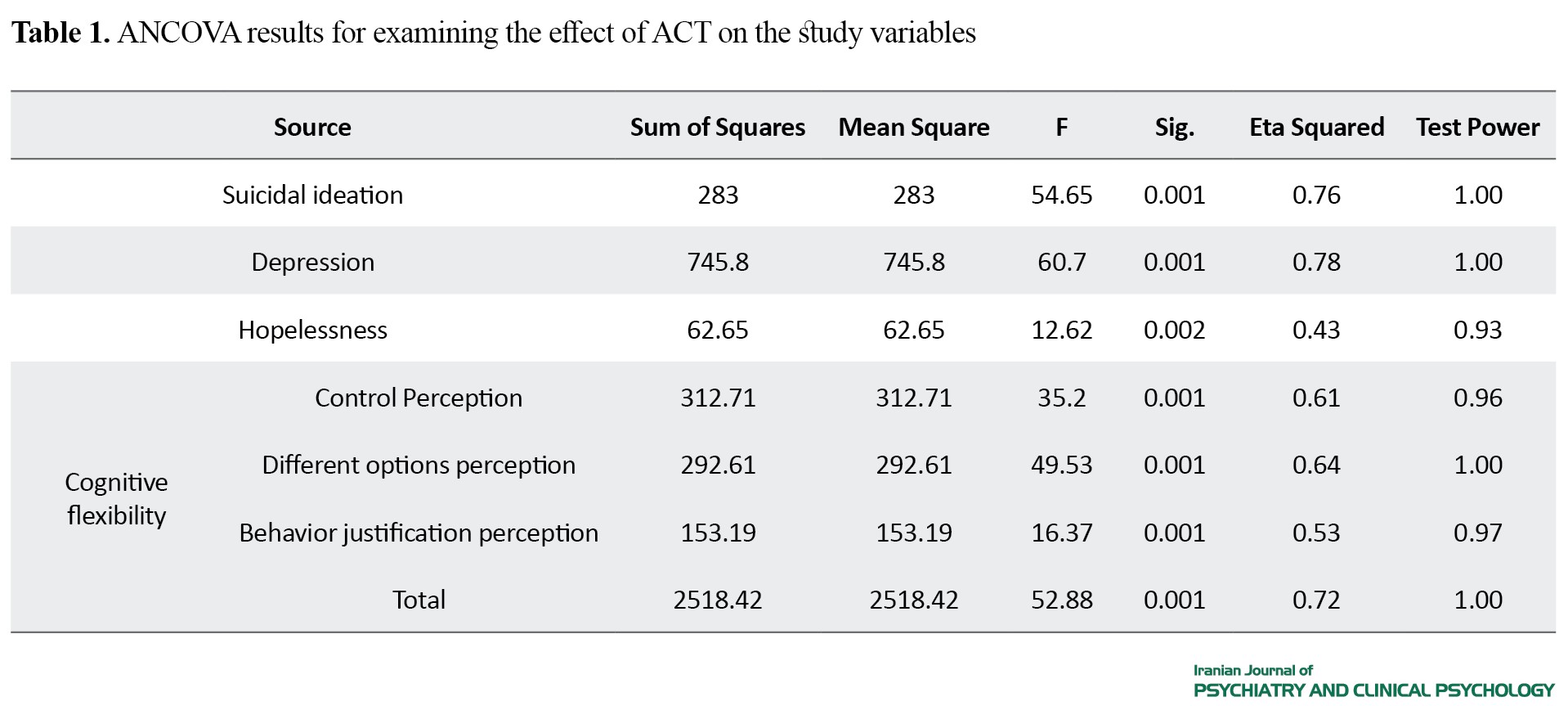
The results revealed that ACT group therapy caused a significant decrease in suicidal ideation, depression and hopelessness, and a significant increase in cognitive flexibility and its components.
4. Discussion
Based on the results of the current study, suicidal ideation, depression and hopelessness in conscripts were significantly reduced compared to controls after ACT, and their cognitive flexibility and its components (control perception, different options perception, and behavior justification perception) improved significantly. Several studies using the ACT have shown that this intervention leads to the development of cognitive flexibility in people suffering from depression, resulting in changes in their life expectancy and quality of life. The goal of ACT is to increase the patients’ ability to connect with their present and be at the moment. Mindfulness and connection with the present (as opposed to overcoming the conceptualized past and future) which lead to cognitive flexibility, can help people get rid of disturbed thoughts, habits and unhealthy behavior patterns and thus play a crucial role in regulating behaviors and reducing depression, suicidal ideation, and hopelessness. People with cognitive flexibility does not avoid unwanted events and does not attempt to control or modify them. They put their energy on values and quality of life instead of avoiding unwanted events.
Overall, it can be concluded that ACT group therapy, through mindfulness training and use of experiential exercises and metaphors, leads to increased cognitive flexibility and individual commitment to perform meaningful actions based on individual values, and ultimately decreases depression, suicidal ideation and hopelessness in conscripts.
Ethical Considerations
Compliance with ethical guidelines
All participants signed a written informed consent form prior to study and they were assured that their information would remain completely confidential. This study obtained its ethical approval from the Ethics Committee of Hakim Sabzevari University (Code: IR.HSU.REC.1398.016) in Iran and registered by Iranian Registry of Clinical Trial (Code: IRCT 20180218038786N2).
Funding
This study was funded by the Deputy for Research of Hakim Sabzevari University, Sabzevar, Iran.
Authors contributions
Conceptualization: Hossein Shareh; Methodology: Hossein Shara, Validation: Hossein Shara, Zahra Robati; Research: Hossein Shareh and Zahra Robati; Sources: Hossein Shareh and Zahra Robati; Drafting: Zahra Robati; Editing and finalizing By: Hossein Shareh; Visualization: Hossein Shareh, Zahra Robati; Supervision: Hossein Shareh; Project Management: Hossein Shareh.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank the managers, physicians and personnel of military counseling centers in Khorasan Razavi Province for cooperation, and all the conscripts who participated in the study.
References
Iranian society is a young society because more than 33% of its population comprised of young people. Of these, eligible males enters the military service according to the laws and in order to protect the Islamic Republic System. Entering the military service leads to major changes in individual, family and social life of people, and is a sensitive period. This period is associated with a lot of stress caused by separation from family and loved ones, changes in dietary habits, restrictions on freedom of choice and action, high and imposed discipline, frequent and forced relocation, changes in sleeping habits, performance anxiety on expectations, fear of having a relationship with others, and inability to resolve problems properly.
Suicide exists in all age groups, but it is more common among young people, especially conscripts, due to their specific situations. According to the World Health Organization, about 800,000 people commit suicide worldwide each year, and it was predicted that this figure would reach 1.5 million people a year by 2020. Nosratabadi et al. found that 28.4% of conscripts are at a high risk of suicidal ideation [8]. Depression is the most important and well-known predictor of suicidal ideation and suicide attempt. Depressed people who commit suicide believe that there is no hope for their future. Hopelessness is an important cause of suicide attempt in depressed people. Cognitive factors such as negativism and hopelessness along with a pessimistic view of the future, belief in disability and inadequacy, and social isolation can increase one’s vulnerability to depression and suicide.
One of the effective approaches in the treatment of depression is Acceptance and Commitment Therapy (ACT), which was introduced by Hayes et al. in the early 1980. The main purpose of ACT is to increase cognitive flexibility through six core processes of acceptance, cognitive defusion, self as context, contact with the present moment, values, and committed action. Cognitive flexibility is a major characteristic of human cognition and refers to one’s ability to simultaneously consider the two conflicting aspects of an object or event. Given the effectiveness of ACT in patients with a variety of psychological disorders, it seems to improve cognitive flexibility and thus reduce suicidal ideation, depression, and hopelessness in conscripts. Therefore, the present study aims to evaluate the effect of ACT group therapy on suicidal ideation, depression, hopelessness and cognitive flexibility among conscripts.
2. Methods
This is a clinical trial with a pretest/posttest design using a control group. The study population consisted of all depressed conscripts referred to military counseling centers in Khorasan Razavi Province of Iran. Of these, 60 conscripts who met the inclusion criteria were randomly selected and assigned into two groups of intervention (n=30) and control (n=30), using a convenience sampling method. The data collection tools were the Beck Scale for Suicidal Ideation, Beck Hopelessness Scale, Beck Depression Inventory-II, and Cognitive Flexibility Inventory. The intervention group received ACT at eight 90-minute sessions, while the control group received no intervention and remained on the waiting list. To analyze the collected data, one-way Analysis of Covariance (ANCOVA) was used in SPSS v. 24 software.
3. Results
Depression, suicidal ideation and hopelessness scores of both groups were very high in the pretest phase. The scores of these variables changed reduced in the intervention group after treatment. The results of ANCOVA comparing the two groups after removing the pretest effects are presented in Table 1.
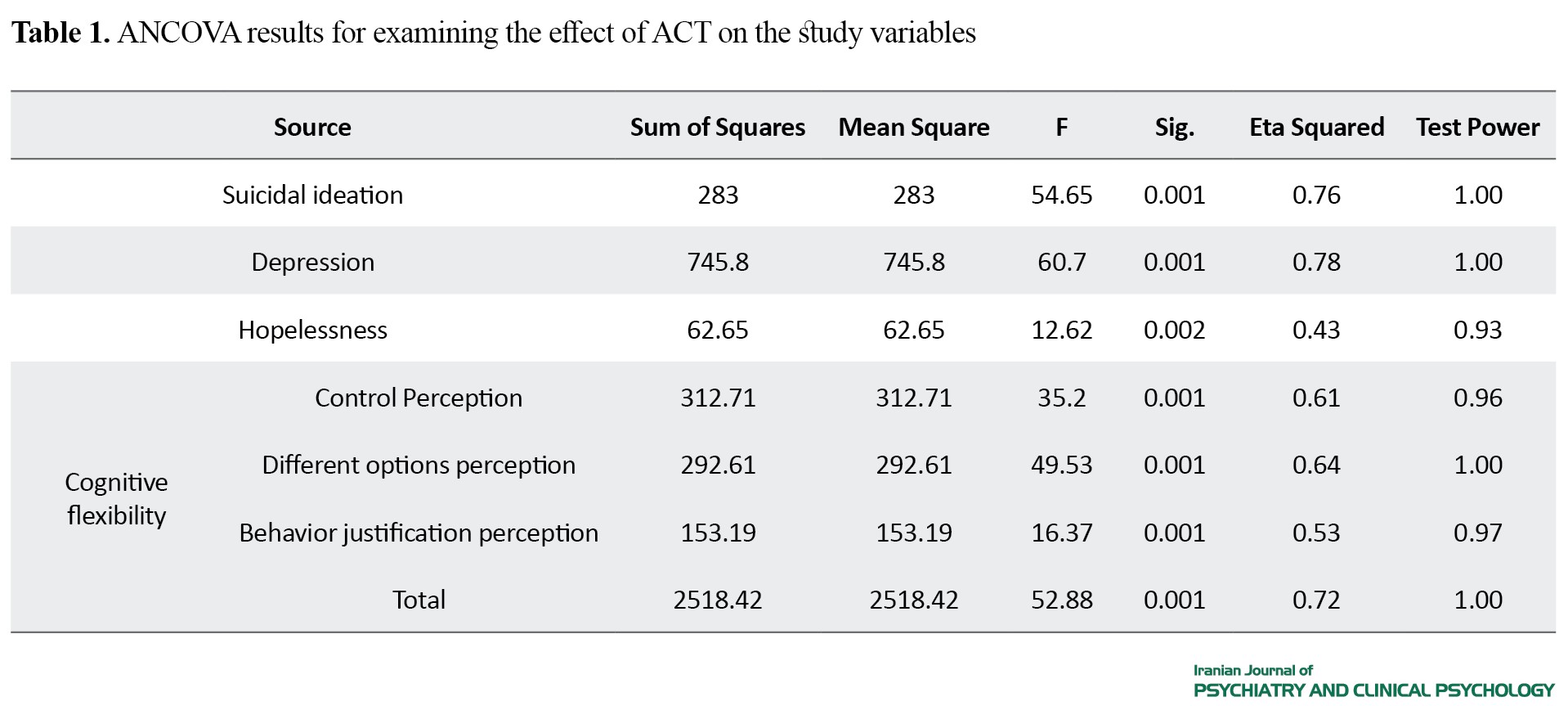
The results revealed that ACT group therapy caused a significant decrease in suicidal ideation, depression and hopelessness, and a significant increase in cognitive flexibility and its components.
4. Discussion
Based on the results of the current study, suicidal ideation, depression and hopelessness in conscripts were significantly reduced compared to controls after ACT, and their cognitive flexibility and its components (control perception, different options perception, and behavior justification perception) improved significantly. Several studies using the ACT have shown that this intervention leads to the development of cognitive flexibility in people suffering from depression, resulting in changes in their life expectancy and quality of life. The goal of ACT is to increase the patients’ ability to connect with their present and be at the moment. Mindfulness and connection with the present (as opposed to overcoming the conceptualized past and future) which lead to cognitive flexibility, can help people get rid of disturbed thoughts, habits and unhealthy behavior patterns and thus play a crucial role in regulating behaviors and reducing depression, suicidal ideation, and hopelessness. People with cognitive flexibility does not avoid unwanted events and does not attempt to control or modify them. They put their energy on values and quality of life instead of avoiding unwanted events.
Overall, it can be concluded that ACT group therapy, through mindfulness training and use of experiential exercises and metaphors, leads to increased cognitive flexibility and individual commitment to perform meaningful actions based on individual values, and ultimately decreases depression, suicidal ideation and hopelessness in conscripts.
Ethical Considerations
Compliance with ethical guidelines
All participants signed a written informed consent form prior to study and they were assured that their information would remain completely confidential. This study obtained its ethical approval from the Ethics Committee of Hakim Sabzevari University (Code: IR.HSU.REC.1398.016) in Iran and registered by Iranian Registry of Clinical Trial (Code: IRCT 20180218038786N2).
Funding
This study was funded by the Deputy for Research of Hakim Sabzevari University, Sabzevar, Iran.
Authors contributions
Conceptualization: Hossein Shareh; Methodology: Hossein Shara, Validation: Hossein Shara, Zahra Robati; Research: Hossein Shareh and Zahra Robati; Sources: Hossein Shareh and Zahra Robati; Drafting: Zahra Robati; Editing and finalizing By: Hossein Shareh; Visualization: Hossein Shareh, Zahra Robati; Supervision: Hossein Shareh; Project Management: Hossein Shareh.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank the managers, physicians and personnel of military counseling centers in Khorasan Razavi Province for cooperation, and all the conscripts who participated in the study.
References
- Youth's National Organization. [Investigation of youths' suicide (Persian)]. Tehran: Ahle Qalam; 2004. http://opac.nlai.ir/opac-prod/bibliographic/674535.
- Farsi Z, Jabari Morouei M, Ebadi A. [General health assessment of army soldiers seen in a military medical outpatient clinic in Tehran (Persian)]. Annals of Military and Health Sciences Research. 2006; 4(3):923-30. https://www.sid.ir/fa/journal/ViewPaper.aspx?id=60866
- Curtis A. Health psychology. London: Routledge; 2000. https://www.routledge.com/Health-Psychology/Curtis/p/book/9780415192736
- Anisi J, Fathi-Ashtiani A, Soltani Nejad A, Amiri M. [Prevalence of suicidal ideation in soldiers and its associated factors (Persian)]. Journal of Military Medicine. 2006; 8(2):113-8. http://militarymedj.ir/article-1-207-fa.html
- Mental Health Advisory Team (MHAT). Operation Iraqi Freedom (OIF) Mental Health Advisory Team (MHAT) report [Internet]. 2003 [Updated 2003 December 16]. Available from: https://www-tc.pbs.org/wgbh/pages/frontline/shows/heart/readings/mhat.pdf
- Sadock BJ, Sadock VA. Kaplan and Sadock’s synopsis of psychiatry behavioral sciences/clinical psychiatry. Philadelphia: Lippincott Williams & Wilkins; 2007. https://books.google.com/books?id=u-ohbTtxCeYC&dq
- World Health Organization. Preventing suicide: A global imperative [Internet]. 2014 [Updated 2014 August 17]. Available from: https://www.who.int/publications/i/item/9789241564779
- Nosratabadi M, Halvaiepoor Z, Ghaed Amini Harooni GR. [Predicting suicide ideation based on psycho-social factors and probability of drug abuse in soldiers: A structural model (Persian)]. Scientific Journal of Ilam University of Medical Sciences. 2017; 24(6):87-96. [DOI:10.18869/acadpub.sjimu.24.6.87]
- Lemaire CM, Graham DP. Factors associated with suicidal ideation in OEF/OIF veterans. Journal of Affective Disorders. 2011; 130(1-2):231-8. [DOI:10.1016/j.jad.2010.10.021]
- Pietrzak RH, Goldstein MB, Malley JC, Rivers AJ, Johnson DC, Southwick SM. Risk and protective factors associated with suicidal ideation in veterans of Operations Enduring Freedom and Iraqi Freedom. Journal of Affective Disorders. 2010; 123(1-3):102-7. [DOI:10.1016/j.jad.2009.08.001] [PMID]
- Kazemi J, Donyavi V, Hosseini SR, Shafighi F, Rouhani SM, Arghanoun Sh, et al. [The prevalence of mood disorder in conscript and official staff of NEZAJA in Tehran by 2005-6 (Persian)]. Annals of Military and Health Sciences Research. 2007; 4(4):993-7. https://www.sid.ir/fa/journal/ViewPaper.aspx?ID=60804
- Assari Sh, Moghani Lankarani M. Depressive symptoms are associated with more hopelessness among white than black older adults. Frontiers in Public Health. 2016; 4:82. [DOI:10.3389/fpubh.2016.00082]
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Gibb BE, Hankin BL, et al. The hopelessness theory of suicidality. In: Joiner TE, Rudd MD, editors. Suicide Science: Expanding the Boundaries. Boston: Kluwer Academic Publishers; 2000. pp. 17-32. https://books.google.com/books?id=m_hfCQ5F2YAC&source=gbs_navlinks_s
- Soltaninejad A, Fathi Ashtiani A, Ahmadi Kh, Yahaghi E, Nikmorad AR, Karimi R, et al. [Structural equation model of borderline personality disorder, emotion-focused coping styles, impulsivity and suicide ideation in soldiers (Persian)]. Journal of Police Medicine. 2012; 1(3):176-82. http://jpmed.ir/article-1-170-fa.html
- Fadaei Z, Ashouri A, Hooshyari Z, Ezanloo B. [Path analysis of locus of control, symptoms of depression and suicidal ideation on academic achievement: The role of gender as moderator (Persian)]. Journal of Fundamentals of Mental Health. 2011; 13(50):148-59. [DOI:10.22038/JFMH.2011.1015]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: The process and practice of mindful change. 2nd ed. New York, NY: Guilford Press; 2012. https://books.google.com/books?id=RvIxDwAAQBAJ&dq
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006; 44(1):1-25. [DOI:10.1016/j.brat.2005.06.006]
- Happel MFK, Niekisch H, Castiblanco Rivera LL, Ohl FW, Deliano M, Frischknecht R. Enhanced cognitive flexibility in reversal learning induced by removal of the extracellular matrix in auditory cortex. Proceedings of the National Academy of Sciences. 2014; 111(7):2800-5. [DOI:10.1073/pnas.1310272111]
- Masuda A, Tully EC. The role of mindfulness and psychological flexibility in somatization depression, anxiety, and general psychological distress in a Nonclinical College Sample. Journal of Evidence-Based Complementary & Alternative Medicine. 2012; 17(1):66-71 [DOI:10.1177/2156587211423400]
- Jacobs ML, Luci K, Hagemann L. Group-based Acceptance and Commitment Therapy (ACT) for older veterans: Findings from a quality improvement project. Clinical Gerontologist. 2018; 41(5):458-67. [DOI:10.1080/07317115.2017.1391917]
- Harvey S, Bimler D, Dickson D, Pack J, Sievwright O, Baken D, et al. Acceptance and commitment therapy group treatment with the military: A preliminary study. Journal of Military and Veterans’ Health. 2018, 26(4):6-15. https://jmvh.org/article/acceptance-and-commitment-therapy-group-treatment-with-the-military-a-preliminary-study/
- Mirzaeidoostan Z, Zargar Y, Zandi Payam A. [The effectiveness of acceptance and commitment therapy on death anxiety and mental health in women with HIV in Abadan city, Iran (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2019; 25 (1):2-13. [DOI:10.32598/ijpcp.25.1.2]
- Karlin BE , Walser RD, Yesavage J, Zhang A, Trockel M, Taylor CB. Effectiveness of acceptance and commitment therapy for depression: Comparison among older and younger veterans. Aging & Mental Health. 2013; 17(5):555-63. [DOI:10.1080/13607863.2013.789002]
- Hiraoka R, Cook AJ, Bivona JM, Meyer EC, Morissette SB. Acceptance and commitment therapy in the treatment of depression related to military sexual trauma in a woman veteran: A case study. Clinical Case Studies. 2016; 15(1):84-97. [DOI:10.1177/1534650115594004]
- Heidari F, Asgari P, Heidari AR, Pasha R, Makvandi B. [The effectiveness of acceptance and commitment therapy on psychological flexibility and rumination in patients with non-cardiac chest pain (Persian)]. Middle Eastern Journal of Disability Studies. 2018; 8:46. http://jdisabilstud.org/article-1-891-en.html
- Scott W, Hann KEJ, McCracken LM. A comprehensive examination of changes in psychological flexibility following acceptance and commitment therapy for chronic pain. Journal of Contemporary Psychotherapy. 2016; 46(3):139-48. [DOI:10.1007/s10879-016-9328-5]
- Ducasse D, Jaussent I, Arpon-Brand V, Vienot M, Laglaoui C, Béziat S, et al. Acceptance and commitment therapy for the management of suicidal patients: A randomized controlled trial. Psychotherapy and Psychosomatics. 2018; 87(4):211-22. [DOI:10.1159/000488715]
- Walser RD, Garvert DW, Karlin BE, Trockel M, Ryu DM, Taylor CB. Effectiveness of acceptance and commitment therapy in treating depression and suicidal ideation in veterans. Behaviour Research and Therapy. 2015; 74:25-31. [DOI:10.1016/j.brat.2015.08.012]
- Rostami H, Fathi A, Kheyri A. [The effectiveness of mindfulness training on reducing aggression and increasing the mental health of soldiers (Persian)]. Iranian Journal of Health Education and Health Promotion. 2019; 7(1):109-17. [DOI:10.30699/ijhehp.7.1.109]
- Farokhzadian AA, Ahmadian F, Andalib L. [The effectiveness of acceptance and commitment therapy on the severity of symptoms and quality of life in soldiers with irritable bowel syndrome (Persian)]. Journal of Military Medicine. 2019; 21(1):44-52. http://militarymedj.ir/article-1-2006-fa.html
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Publications; 1999. https://books.google.com/books?id=DjndwAEACAAJ&dq
- Zhang J, Brown GK. Psychometric properties of the scale for suicide ideation in China. Archives of Suicide Research. 2007; 11(2):203-10. [DOI:10.1080/13811110600894652]
- Anisi J, Fathi Ashtiani A, Salimi SH, Ahmadi Noudeh Kh. [Validity and reliability of Beck Suicide Scale Ideation (BSSI) among soldiers (Persian)]. Journal of Military Medicine. 2005; 7(1):33-7. https://www.sid.ir/fa/journal/ViewPaper.aspx?ID=22790
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology. 1974; 42(6):861-5. [DOI:10.1037/h0037562]
- Aiken LR. Psychological testing and assessment. New York: Allyn & Bacon; 2003. https://www.google.com/books/edition/Psychological_Testing_and_Assessment/XWF9AAAAMAAJ?hl=en
- Tarsafi M, Kalantari Kouche SM, Lester D. [Exploratory factor analysis of the defeat scale and its relationship with depression and hopelessness among Iranian university students (Persian)]. Clinical Psychology Studies. 2015; 5(19):81-98. https://jcps.atu.ac.ir/article_1498.html
- Dejkam N. [Conformity and norm of the Beck hopelessness scale among students of Tehran Islamic Azad University (Persian)] [MA. thesis]. Tehran: The Islamic Azad University, Central Tehran Branch; 2004. http://opac.nlai.ir/opac-prod/bibliographic/832493
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: The Psychological Corporation; 1996. https://www.nctsn.org/measures/beck-depression-inventory-second-edition
- Grothe KB, Dutton GR, Jones GN, Bodenlos J, Ancona M, Brantley PJ. Validation of the Beck Depression Inventory-II in a low-income African American sample of medical outpatients. Psychological Assessment. 2005; 17(1):110-4. [DOI:10.1037/1040-3590.17.1.110]
- Kapci EG, Uslu R, Turkcapar H, Karaoglan A. Beck Depression Inventory II: Evaluation of the psychometric properties and cut- off points in a Turkish adult population. Depression and Anxiety. 2008; 25(10):E104-10. [DOI:10.1002/da.20371]
- Stefan-Dabson K, Mohammadkhani P, Massah-Choulabi O. [Psychometrics characteristic of Beck Depression Inventory-II in patients with major depressive disorder (Persian)]. Archives of Rehabilitation. 2007; 8:80-6. http://rehabilitationj.uswr.ac.ir/article-1-135-en.html
- Dennis JP, Vander Wal JS. The cognitive flexibility inventory: Instrument development and estimates of reliability and validity. Cognitive Therapy and Research. 2010; 34(3):241-53. [DOI:10.1007/s10608-009-9276-4]
- Shareh H, Farmani A, Soltani E. Investigating the reliability and validity of the Cognitive Flexibility Inventory (CFI-I) among Iranian university students. Practice in Clinical Psychology. 2014; 2(1):43-50. http://jpcp.uswr.ac.ir/article-1-163-en.html
- Shekari HR, Dabbaghi P, Dowran B, Taghva A. [Effectiveness of group training of acceptance and commitment therapy on depression symptoms in soldiers (Persian)]. Ebnesina Journal. 2016; 18(2):19-25. http://ebnesina.ajaums.ac.ir/article-1-399-fa.html
- Tighe J, Nicholas J, Shand F, Christensen H. Efficacy of acceptance and commitment therapy in reducing suicidal ideation and deliberate self-harm: Systematic review. JMIR Mental Health. 2018; 5(2):e10732. [DOI:10.2196/10732] [PMID] [PMCID]
- Goudarzi AH, Golmahammadi AA, Bashirgonabadi S, Samadi S. [Effectiveness based on reducing stress (MBSR) on suicidal thoughts and aggression in the soldiers with normal task force of Malek-e-Ashtar Arak garrison training course (Persian)]. Journal of Police Medicine. 2018; 7(4):147-152. [DOI:10.30505/7.4.147]
- Yazarloo M, Kalantari M, Mehrabi H. [Effectiveness of acceptance and commitment therapy on military personnel mental health (Persian)]. Journal of Police Medicine. 2018; 7(1):13-8. [DOI:10.30505/7.1.13]
- Moghadam N, Amraae R, Asadi F, Amani O. [The efficacy of Acceptance and Commitment Therapy (ACT) on hope and psychological well-being in women with breast cancer under chemotherapy (Persian)]. Iranian Journal of Psychiatric Nursing. 2018; 6(5):1-8. http://ijpn.ir/article-1-1155-en.html
- Forman EM, Herbert JD. New directions in cognitive behavior therapy: Acceptance-based therapies. In: O’Donohue WT, Fisher JE, editors. General principles and empirically supported techniques of cognitive behavior therapy. New York: John Wiley & Sons; 2009. https://psycnet.apa.org/record/2009-02305-005
- Soltani E, Shareh H, Bahrainian SA, Farmani A. [The mediating role of cognitive flexibility in correlation of coping styles and resilience with depression (Persian)]. Pajoohandeh. 2013; 18(2):88-96. http://pajoohande.sbmu.ac.ir/article-1-1518-en.html
- Sadri Damirchi E, Samadifard HR. [The role of irrational beliefs, mindfulness and cognitive avoidance in the prediction of suicidal thoughts in soldiers (Persian)]. Journal of Military Medicine . 2018; 20(4):431-8. http://militarymedj.ir/article-1-1659-en.html
- Barnhofer T, Crane C, Brennan K, Duggan DS, Crane RS, Eames C, et al. Mindfulness-Based Cognitive Therapy (MBCT) reduces the association between depressive symptoms and suicidal cognitions in patients with a history of suicidal depression. Journal of Consulting and Clinical Psychology. 2015; 83(6):1013-20. [DOI:10.1037/ccp0000027]
- Sheydayi Aghdam Sh, Shamseddini Lory S, Abassi S, Yosefi S, Abdollahi S, Moradi Joo M. [The effectiveness of treatment based on acceptance and commitment in reducing distress and inefficient attitudes in patients with MS (Persian)]. Thoughts and Behavior in Clinical Psychology. 2015; 9(34):57-66. https://jtbcp.riau.ac.ir/article_108.html
Type of Study: Original Research |
Subject:
Psychiatry and Psychology
Received: 2020/04/19 | Accepted: 2020/10/6 | Published: 2022/01/1
Received: 2020/04/19 | Accepted: 2020/10/6 | Published: 2022/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






